Search
- Page Path
- HOME > Search
Original Article
- Diabetes, obesity and metabolism
- Effects of an Electronic Medical Records-Linked Diabetes Self-Management System on Treatment Targets in Real Clinical Practice: Retrospective, Observational Cohort Study
- So Jung Yang, Sun-Young Lim, Yoon Hee Choi, Jin Hee Lee, Kun-Ho Yoon
- Endocrinol Metab. 2024;39(2):364-374. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1878

- 427 View
- 11 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study evaluated the effects of a mobile diabetes management program called “iCareD” (College of Medicine, The Catholic University of Korea) which was integrated into the hospital’s electronic medical records system to minimize the workload of the healthcare team in the real clinical practice setting.
Methods
In this retrospective observational study, we recruited 308 patients. We categorized these patients based on their compliance regarding their use of the iCareD program at home; compliance was determined through self-monitored blood glucose inputs and message subscription rates. We analyzed changes in the ABC (hemoglobin A1c, blood pressure, and low-density lipoprotein cholesterol) levels from the baseline to 12 months thereafter, based on the patients’ iCareD usage patterns.
Results
The patients comprised 92 (30%) non-users, 170 (55%) poor-compliance users, and 46 (15%) good-compliance users; the ABC target achievement rate showed prominent changes in good-compliance groups from baseline to 12 months (10.9% vs. 23.9%, P<0.05), whereas no significant changes were observed for poor-compliance users and non-users (13.5% vs. 18.8%, P=0.106; 20.7% vs. 14.1%, P=0.201; respectively).
Conclusion
Implementing the iCareD can improve the ABC levels of patients with diabetes with minimal efforts of the healthcare team in real clinical settings. However, the improvement of patients’ compliance concerning the use of the system without the vigorous intervention of the healthcare team needs to be solved in the future.

Review Article
- Diabetes, obesity and metabolism
- Initial Combination Therapy in Type 2 Diabetes
- Ji Yoon Kim, Nam Hoon Kim
- Endocrinol Metab. 2024;39(1):23-32. Published online November 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1816
- 2,086 View
- 250 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
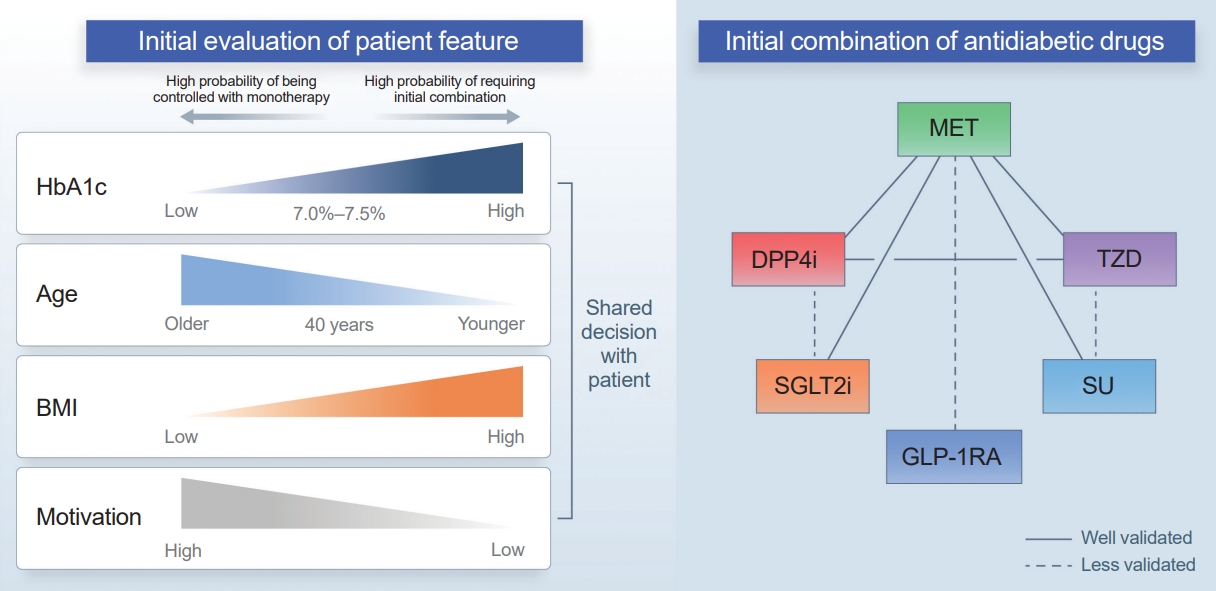
ePub - Type 2 diabetes (T2D) is a progressive disease in which it is challenging to achieve long-term durable glycemic control. However, intensive glycemic control is crucial for preventing diabetes-related complications. Previous studies showed that monotherapy with a stepwise add-on approach was seldom effective for long-term durable glycemic control. Combination therapy, which refers to the use of two or more drugs to control hyperglycemia, has multiple benefits, including the ability to target a variety of pathophysiological processes underlying hyperglycemia. In clinical trials, initial combination therapy showed better glycemic control than monotherapy or a stepwise approach. Emerging evidence indicates that initial combination therapy is associated with preserved β-cell function and fewer complications in T2D. However, cost-effectiveness and adverse events with combination therapy are issues that should be considered. Therefore, initial combination therapy is an important option for patients with T2D that clinicians should consider with a view toward balancing benefits and potential harms. In this review, we summarize the literature addressing initial combination therapy in T2D, and we suggest optimal strategies based on clinical situations and patient characteristics.

Original Articles
- Thyroid
- Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
- Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
- Endocrinol Metab. 2023;38(6):729-738. Published online November 2, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1769
- 1,112 View
- 73 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study investigates the association between thyroid function and frailty in the old patients using representative data.
Methods
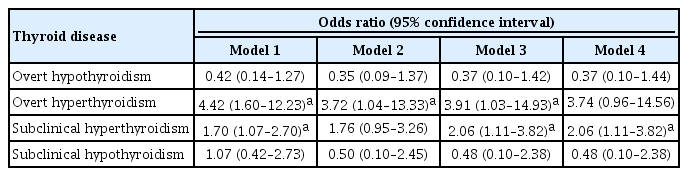
The study was conducted using data from the Korea National Health and Nutrition Examination Survey conducted from 2013 to 2015. The study population included 2,416 participants aged 50 years and older with available thyroid function test data. Frailty assessment was performed using the Fried frailty phenotype. The prevalence of frailty was analyzed across different thyroid diseases and thyroid function parameters.
Results
The significant association between thyroid dysfunction and frailty was observed in overt hyperthyroidism and subclinical hyperthyroidism. After adjusting for various factors, the association between thyroid dysfunction and frailty remained significant. On the other hand, overt hypothyroidism did not show a significant association with frailty in the adjusted analysis. For individuals with overt hyperthyroidism and subclinical hyperthyroidism, higher levels of free thyroxine (FT4) were significantly associated with an increased risk of frailty (aOR >999; 95% CI, >999 to 999). Among individuals with overt hypothyroidism, lower level of FT4 levels and high thyrotropin (TSH) levels showed a significant association with frailty risk (FT4: aOR, <0.01; TSH: aOR, 999). In participants with subclinical hypothyroidism, there were no significant associations between parameters for thyroid and frailty risk.
Conclusion
These findings suggest that thyroid dysfunction, particularly overt hyperthyroidism and subclinical hyperthyroidism, may be associated with an increased risk of frailty in the old patients. -
Citations
Citations to this article as recorded by- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China
Heng Wan, Genfeng Yu, Yajun He, Siyang Liu, Xingying Chen, Yuqi Jiang, Hualin Duan, Xu Lin, Lan Liu, Jie Shen
Annals of Medicine.2024;[Epub] CrossRef
- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China

- Diabetes, obesity and metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
- Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee, Committee of Big Data, Korean Endocrine Society
- Endocrinol Metab. 2023;38(5):525-537. Published online September 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1765
- 1,587 View
- 91 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
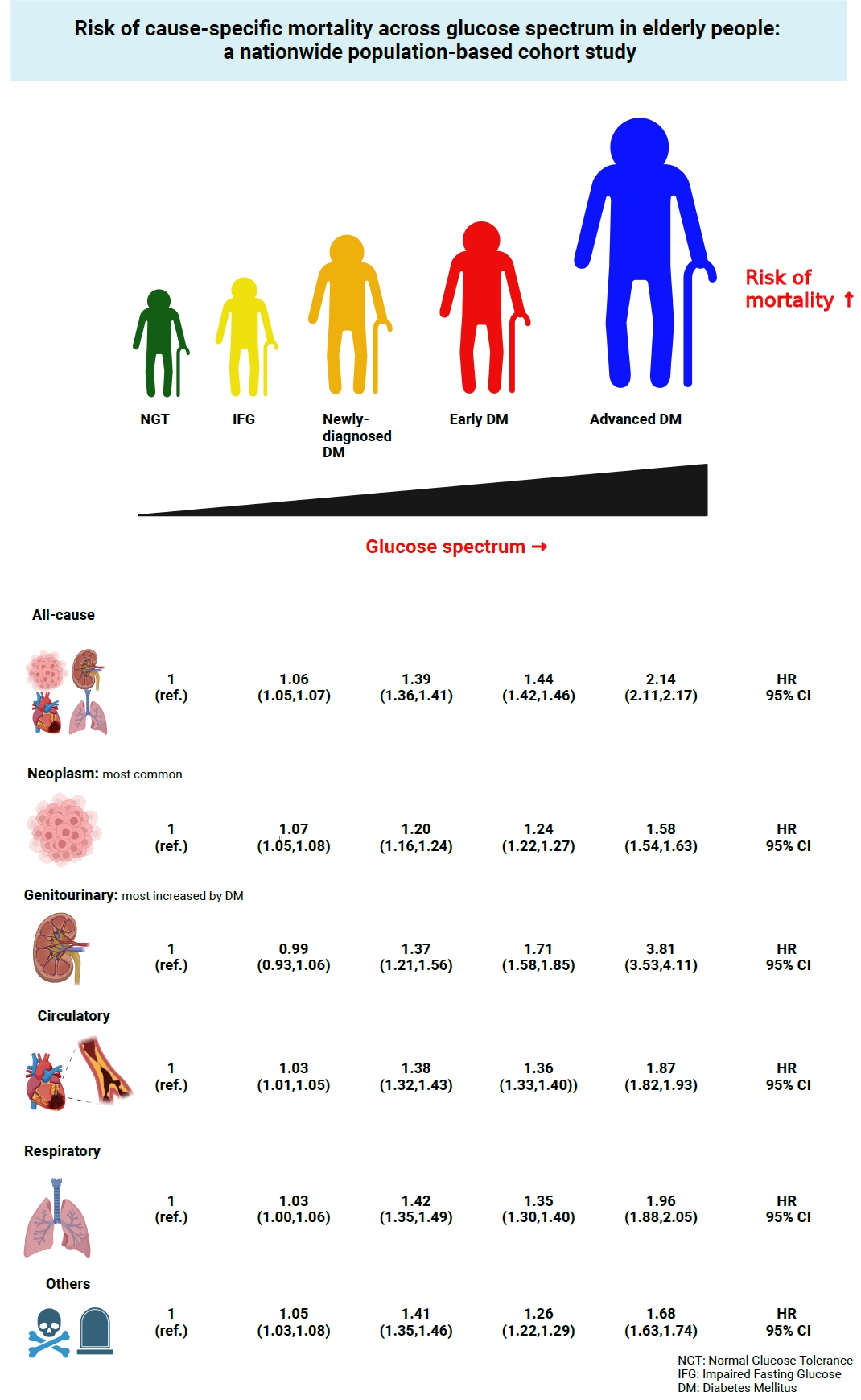
This study investigated the risk of cause-specific mortality according to glucose tolerance status in elderly South Koreans.
Methods
A total of 1,292,264 individuals aged ≥65 years who received health examinations in 2009 were identified from the National Health Information Database. Participants were classified as normal glucose tolerance, impaired fasting glucose, newly-diagnosed diabetes, early diabetes (oral hypoglycemic agents ≤2), or advanced diabetes (oral hypoglycemic agents ≥3 or insulin). The risk of system-specific and disease-specific deaths was estimated using multivariate Cox proportional hazards analysis.
Results
During a median follow-up of 8.41 years, 257,356 deaths were recorded. Diabetes was associated with significantly higher risk of all-cause mortality (hazard ratio [HR], 1.58; 95% confidence interval [CI], 1.57 to 1.60); death due to circulatory (HR, 1.49; 95% CI, 1.46 to 1.52), respiratory (HR, 1.51; 95% CI, 1.47 to 1.55), and genitourinary systems (HR, 2.22; 95% CI, 2.10 to 2.35); and neoplasms (HR, 1.30; 95% CI, 1.28 to 1.32). Diabetes was also associated with a significantly higher risk of death due to ischemic heart disease (HR, 1.70; 95% CI, 1.63 to 1.76), cerebrovascular disease (HR, 1.46; 95% CI, 1.41 to 1.50), pneumonia (HR, 1.69; 95% CI, 1.63 to 1.76), and acute or chronic kidney disease (HR, 2.23; 95% CI, 2.09 to 2.38). There was a stepwise increase in the risk of death across the glucose spectrum (P for trend <0.0001). Stroke, heart failure, or chronic kidney disease increased the risk of all-cause mortality at every stage of glucose intolerance.
Conclusion
A dose-dependent association between the risk of mortality from various causes and severity of glucose tolerance was noted in the elderly population. -
Citations
Citations to this article as recorded by- The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef
- The Characteristics and Risk of Mortality in the Elderly Korean Population

Review Article
- Thyroid
- Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
- Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
- Endocrinol Metab. 2023;38(4):381-391. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1778
- 3,045 View
- 462 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
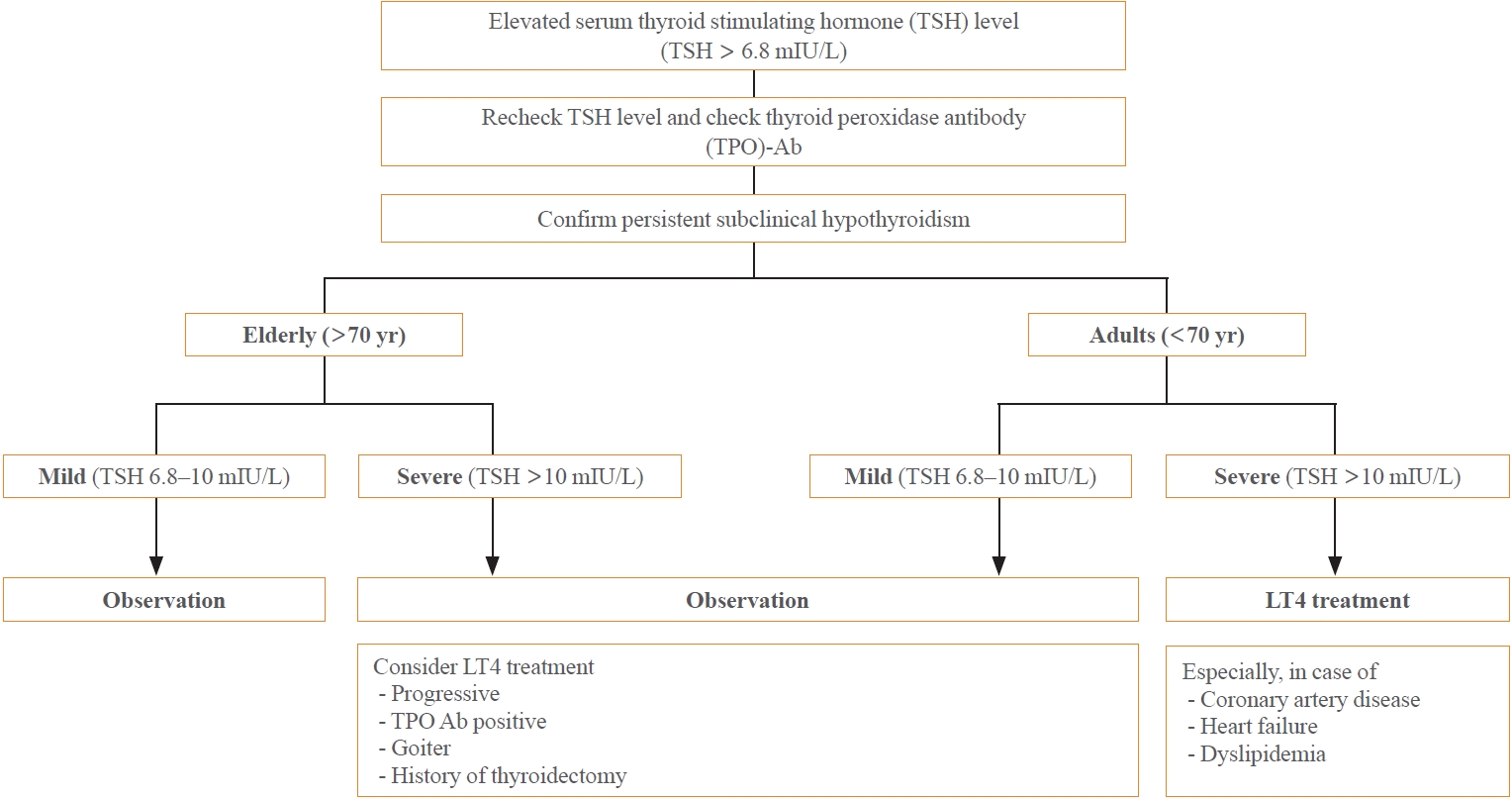
ePub - Subclinical hypothyroidism (SCH) is characterized by elevated thyroid-stimulating hormone (TSH) and normal free thyroxine levels. The Korean Thyroid Association recently issued a guideline for managing SCH, which emphasizes Korean-specific TSH diagnostic criteria and highlights the health benefits of levothyroxine (LT4) treatment. A serum TSH level of 6.8 mIU/L is presented as the reference value for diagnosing SCH. SCH can be classified as mild (TSH 6.8 to 10.0 mIU/L) or severe (TSH >10.0 mIU/L), and patients can be categorized as adults (age <70 years) or elderly (age ≥70 years), depending on the health effects of LT4 treatment. An initial increase in serum TSH levels should be reassessed with a subsequent measurement, including a thyroid peroxidase antibody test, preferably 2 to 3 months after the initial assessment. While LT4 treatment is not generally recommended for mild SCH in adults, it is necessary for severe SCH in patients with underlying coronary artery disease or heart failure and it may be considered for those with concurrent dyslipidemia. Conversely, LT4 treatment is generally not recommended for elderly patients, regardless of SCH severity. For those SCH patients who are prescribed LT4 treatment, the dosage should be personalized, and serum TSH levels should be regularly monitored to maintain the optimal LT4 regimen.
-
Citations
Citations to this article as recorded by- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism
Won Sang Yoo
Endocrinology and Metabolism.2024; 39(1): 188. CrossRef
- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism

Original Articles
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
- Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1684
- 1,816 View
- 127 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
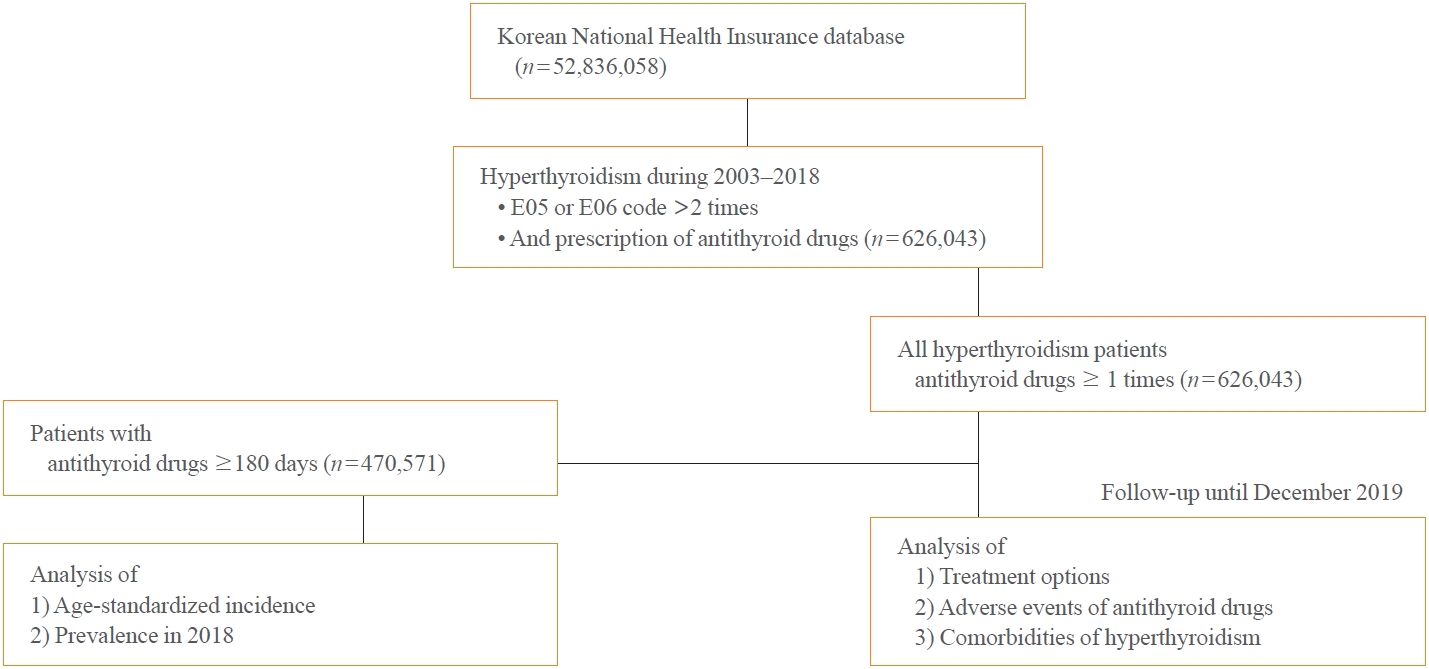
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age. -
Citations
Citations to this article as recorded by- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients

- Thyroid
- Thyroid Hormone Reference Intervals among Healthy Individuals In Lanzhou, China
- Yan Lu, Wen-Xia Zhang, De-Hong Li, Lian-Hua Wei, Yu-Jun Zhang, Fu-Na Shi, Shen Zhou
- Endocrinol Metab. 2023;38(3):347-356. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1638
- 2,009 View
- 119 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
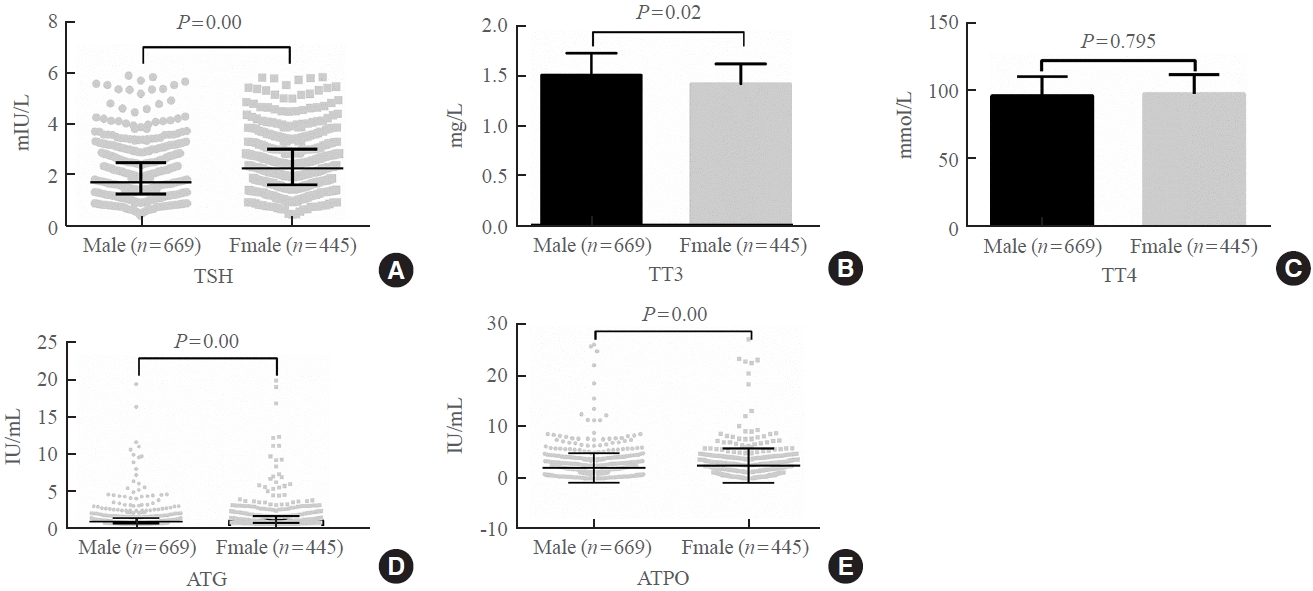
The common reference intervals (RIs) for thyroid hormones currently used in China are provided by equipment manufacturers. This study aimed to establish thyroid hormone RIs in the population of Lanzhou, a city in the subplateau region of northwest China, and compare them with previous reports and manufacturer-provided values.
Methods
In total, 3,123 individuals (1,680 men, 1,443 women) from Lanzhou, an iodine-adequate area of China, perceived as healthy were selected. The Abbott Architect analyzer was used to determine the serum concentration of thyroid hormones. The 95% RI was estimated using the 2.5th and 97.5th percentiles as the lower and upper reference limits, respectively.
Results
The serum levels of thyroid-stimulating hormone (TSH), total triiodothyronine (TT3), antithyroglobulin (ATG) antibody, and antithyroid peroxidase (ATPO) antibody levels were significantly correlated with sex (P<0.05). TSH, total thyroxine (TT4), and ATPO levels were significantly correlated with age (P<0.05). The serum levels of TSH, ATG, and ATPO in men were significantly lower than in women; in contrast, the serum TT3 level was significantly higher in men than in women (P<0.05). Serum TSH, TT3, TT4, and ATG levels differed across age groups (P<0.05), but no such variation was observed for ATG levels (P>0.05). The established RIs of TSH, ATG, and ATPO in this study differed between sexes (P<0.05). The thyroid hormone RIs established herein were inconsistent with the manufacturer-provided values.
Conclusion
The RIs of thyroid hormones in the healthy population of Lanzhou were inconsistent with those in the manufacturer’s manual. Validated sex-specific values are required for diagnosing thyroid diseases.

- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
- Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
- Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1664
- 1,748 View
- 102 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
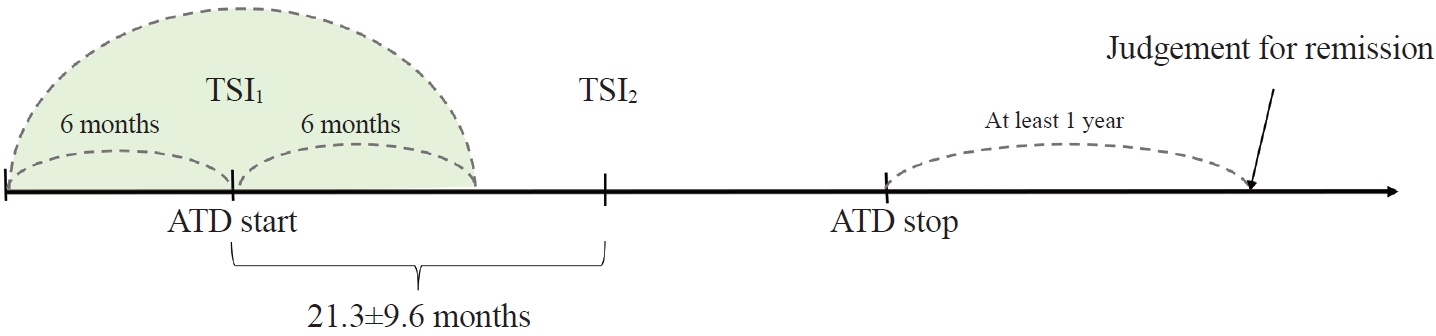
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII,P =0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis. -
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

Review Article
- Calcium & Bone Metabolism
- Updates on Paget’s Disease of Bone
- Yong Jun Choi, Young Bae Sohn, Yoon-Sok Chung
- Endocrinol Metab. 2022;37(5):732-743. Published online October 25, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1575

- 3,780 View
- 317 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Paget’s disease of the bone is a prevalent bone disease characterized by disorganized bone remodeling; however, it is comparatively uncommon in East Asian countries, including China, Japan, and Korea. The exact cause still remains unknown. In genetically susceptible individuals, environmental triggers such as paramyxoviral infections are likely to cause the disease. Increased osteoclast activity results in increased bone resorption, which attracts osteoblasts and generates new bone matrix. Fast bone resorption and formation lead to the development of disorganized bone tissue. Increasing serum alkaline phosphatase or unique radiographic lesions may serve as the diagnostic indicators. Common symptoms include bone pain, bowing of the long bones, an enlarged skull, and hearing loss. The diagnosis is frequently confirmed by radiographic and nuclear scintigraphy of the bone. Further, bisphosphonates such as zoledronic acid and pamidronate are effective for its treatment. Moreover, biochemical monitoring is superior to the symptoms as a recurrence indicator. This article discusses the updates of Paget’s disease of bone with a clinical case.
-
Citations
Citations to this article as recorded by- Effects of Erythropoietin-Promoted Fracture Healing on Bone Turnover Markers in Cats
Radina Vasileva, Tsvetan Chaprazov, Aneliya Milanova
Journal of Functional Biomaterials.2024; 15(4): 106. CrossRef - Newly Diagnosed Monostotic Paget’s Disease of Bone during Living Kidney Donor Candidate Evaluation
Diana Jędrzejuk, Paweł Poznański, Paweł Szewczyk, Oktawia Mazanowska, Marek Bolanowski, Magdalena Krajewska, Dorota Kamińska
Biomedicines.2023; 11(2): 401. CrossRef - Paget's disease of bone in the patient presented with a bowed leg
Mehrzad Hajialiloo, Sepideh Tahsini Tekantapeh
Clinical Case Reports.2023;[Epub] CrossRef
- Effects of Erythropoietin-Promoted Fracture Healing on Bone Turnover Markers in Cats

Original Article
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(4):641-651. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1501
- 6,190 View
- 166 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
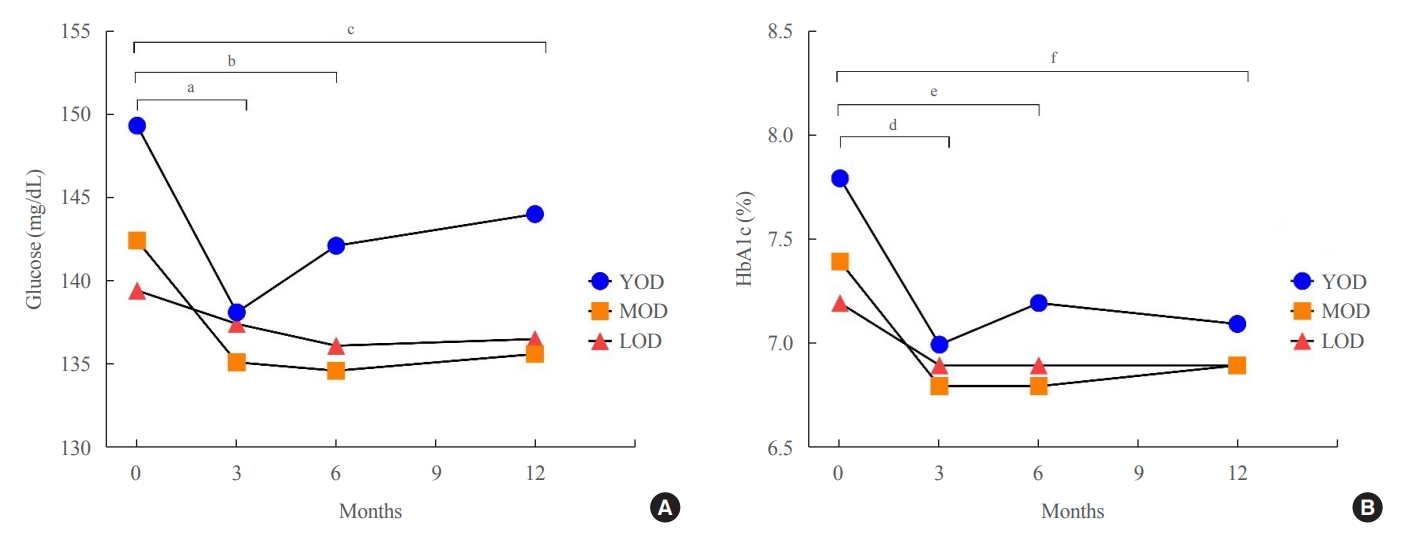
The prevalence of young-onset diabetes (YOD) has been increasing worldwide. As the incidence of YOD increases, it is necessary to determine the characteristics of YOD and the factors that influence its development and associated complications.
Methods
In this retrospective study, we recruited patients who were diagnosed with type 2 diabetes mellitus between June 2001 and December 2021 at a tertiary hospital. The study population was categorized according to age: YOD (age <40 years), middle-age-onset diabetes (MOD, 40≤ age <65 years), and late-onset diabetes (LOD, age ≥65 years). We examined trends in glycemic control by analyzing fasting glucose levels during the first year in each age group. A Cox proportional-hazards model was used to determine the relative risk of developing complications according to glycemic control trends.
Results
The fasting glucose level at the time of diagnosis was highest in the YOD group (YOD 149±65 mg/dL; MOD 143±54 mg/dL; and LOD 140±55 mg/dL; p=0.009). In the YOD group, glucose levels decreased at 3 months, but increased by 12 months. YOD patients and those with poor glycemic control in the first year were at a higher risk of developing complications, whereas the risk in patients with LOD was not statistically significant.
Conclusion
YOD patients had higher glucose levels at diagnosis, and their glycemic control was poorly maintained. As poor glycemic control can influence the development of complications, especially in young patients, intensive treatment is necessary for patients with YOD. -
Citations
Citations to this article as recorded by- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(1): 101505. CrossRef - Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus
Hye-Sun Park, Yongin Cho, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, Suk Chon, Jeong-Taek Woo, Sei Hyun Baik, Kwan Woo Lee, So Hun Kim
Scientific Reports.2024;[Epub] CrossRef - Early onset type 2 diabetes mellitus: an update
Myrsini Strati, Melpomeni Moustaki, Theodora Psaltopoulou, Andromachi Vryonidou, Stavroula A. Paschou
Endocrine.2024;[Epub] CrossRef - Complications and Treatment of Early-Onset Type 2 Diabetes
Fahimeh Soheilipour, Naghmeh Abbasi Kasbi, Mahshid Imankhan, Delaram Eskandari
International Journal of Endocrinology and Metabolism.2023;[Epub] CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
Endocrinology and Metabolism.2022; 37(6): 945. CrossRef -
ISPAD
Clinical Practice Consensus Guidelines 2022: Management of the child, adolescent, and young adult with diabetes in limited resource settings
Anju Virmani, Stuart J. Brink, Angela Middlehurst, Fauzia Mohsin, Franco Giraudo, Archana Sarda, Sana Ajmal, Julia E. von Oettingen, Kuben Pillay, Supawadee Likitmaskul, Luis Eduardo Calliari, Maria E. Craig
Pediatric Diabetes.2022; 23(8): 1529. CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
May Thu Hla Aye, Sajid Adhi Raja, Vui Heng Chong
Endocrinology and Metabolism.2022; 37(6): 943. CrossRef
- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study

Review Article
- Calcium & Bone Metabolism
- A Key Metabolic Regulator of Bone and Cartilage Health
- Elizabeth Pérez-Hernández, Jesús Javier Pastrana-Carballo, Fernando Gómez-Chávez, Ramesh C. Gupta, Nury Pérez-Hernández
- Endocrinol Metab. 2022;37(4):559-574. Published online August 8, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1443

- 7,914 View
- 342 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Taurine, a cysteine-derived zwitterionic sulfonic acid, is a common ingredient in energy drinks and is naturally found in fish and other seafood. In humans, taurine is produced mainly in the liver, and it can also be obtained from food. In target tissues, such as the retina, heart, and skeletal muscle, it functions as an essential antioxidant, osmolyte, and antiapoptotic agent. Taurine is also involved in energy metabolism and calcium homeostasis. Taurine plays a considerable role in bone growth and development, and high-profile reports have demonstrated the importance of its metabolism for bone health. However, these reports have not been collated for more than 10 years. Therefore, this review focuses on taurine–bone interactions and covers recently discovered aspects of taurine’s effects on osteoblastogenesis, osteoclastogenesis, bone structure, and bone pathologies (e.g., osteoporosis and fracture healing), with due attention to the taurine–cartilage relationship.
-
Citations
Citations to this article as recorded by- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis
Mengxing Yin, Dezhi Zhou, Fu Jia, Xiaosan Su, Xiufang Li, Ruifen Sun, Junmin Li
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - An in-silico approach to the potential modulatory effect of taurine on sclerostin (SOST) and its probable role during osteoporosis
Mazumder Adhish, I. Manjubala
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis

Original Article
- Diabetes, Obesity and Metabolism
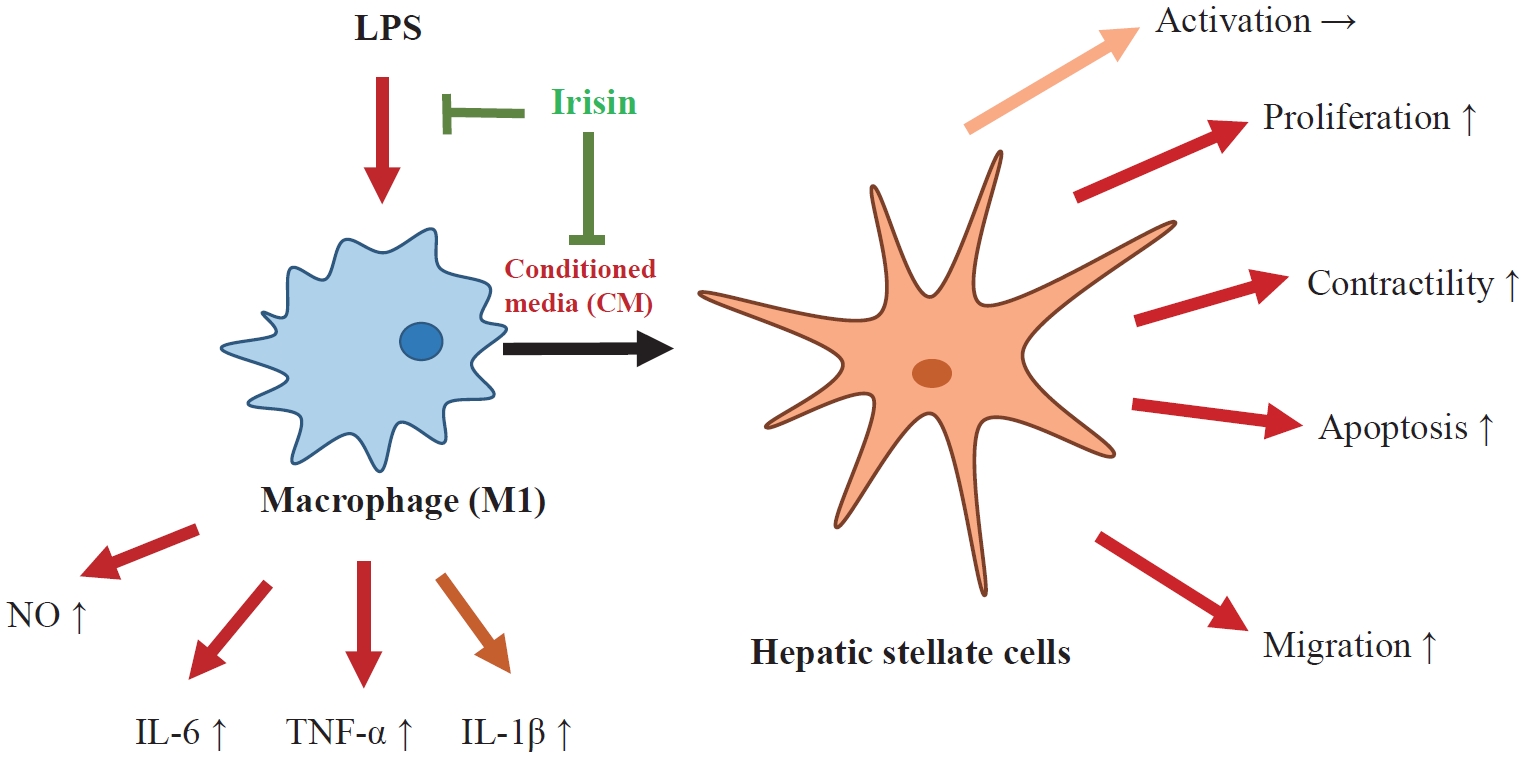
- The Effects of Irisin on the Interaction between Hepatic Stellate Cell and Macrophage in Liver Fibrosis
- Dinh Vinh Do, So Young Park, Giang Thi Nguyen, Dae Hee Choi, Eun-Hee Cho
- Endocrinol Metab. 2022;37(4):620-629. Published online July 22, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1412
- 4,571 View
- 198 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Hepatic stellate cells (HSCs) are the central players interacting with multiple cell types in liver fibrosis. The crosstalk between HSCs and macrophages has recently become clearer. Irisin, an exercise-responsive myokine, was known to have a potentially protective role in liver and renal fibrosis, especially in connection with stellate cells. This study investigated the effects of irisin on the interaction between HSCs and macrophages.
Methods
Tamm-Horsfall protein-1 (THP-1) human monocytes were differentiated into macrophages, polarized into the inflammatory M1 phenotype with lipopolysaccharide. Lieming Xu-2 (LX-2) cells, human HSCs, were treated with conditioned media (CM) from M1 macrophages, with or without recombinant irisin. HSCs responses to CM from M1 macrophages were evaluated regarding activation, proliferation, wound healing, trans-well migration, contractility, and related signaling pathway.
Results
CM from M1 macrophages significantly promoted HSC proliferation, wound healing, transwell migration, and contractility, but not activation of HSCs. Irisin co-treatment attenuated these responses of HSCs to CM. However, CM and irisin treatment did not induce any changes in HSC activation. Further, irisin co-treatment alleviated CM-induced increase of phopho-protein kinase B (pAKT), matrix metalloproteinase-9 (MMP-9), and tissue inhibitor of metalloproteinases-1 (TIMP-1).
Conclusion
These findings suggested that irisin may play a protective role in the pathogenesis of liver fibrosis, especially when working in the crosstalk between HSCs and macrophages. -
Citations
Citations to this article as recorded by- Matrix metalloproteinases induce extracellular matrix degradation through various pathways to alleviate hepatic fibrosis
Liang Shan, Fengling Wang, Dandan Zhai, Xiangyun Meng, Jianjun Liu, Xiongwen Lv
Biomedicine & Pharmacotherapy.2023; 161: 114472. CrossRef - Potential role of irisin in digestive system diseases
Yueming Zhang, Linxian Zhao, Huan Gao, Jinghui Zhai, Yanqing Song
Biomedicine & Pharmacotherapy.2023; 166: 115347. CrossRef - The effect of sarcopenia and serum myokines on prognosis and survival in cirrhotic patients: a multicenter cross-sectional study
Salih Boga, Abdullah Emre Yildirim, Enver Ucbilek, Ali Riza Koksal, Sevil Tokdemir Sisman, Ibrahim Durak, Ilker Sen, Beril Dogu, Erdinc Serin, Ayse Bolat Ucbilek, Makbule Ozge Yildirim, Sukru Mehmet Erturk, Huseyin Alkim, Canan Alkim
European Journal of Gastroenterology & Hepatology.2022; 34(12): 1261. CrossRef
- Matrix metalloproteinases induce extracellular matrix degradation through various pathways to alleviate hepatic fibrosis

Review Article
- Diabetes, Obesity and Metabolism
- Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
- Eun-Jung Rhee
- Endocrinol Metab. 2022;37(3):415-429. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.304

- 4,516 View
- 262 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The world is suffering from a rapid increase in the number of people with diabetes due to the increased prevalence of obesity and lengthened life span. Since the development of insulin thanks to the efforts of Prof. Banting and Dr. Best in 1922, for which they won the Nobel Prize, remarkable developments in anti-diabetic medications have dramatically lengthened the lifespan of patients with diabetes. However, the control rate of hyperglycemia in patients with diabetes remains unsatisfactory, since glycemic control requires both medication and lifestyle modifications to slow the deterioration of pancreatic beta-cell function and prevent diabetic complications. From the initial “triumvirate” to the “ominous octet,” and now the “egregious eleven,” the number of organs recognized as being involved in hyperglycemia and diabetes has increased with the development of anti-diabetic medications. Recent unexpected results from outcome trials of anti-diabetic medications have enabled anti-diabetic medications to be indicated for the prevention of chronic kidney disease and heart failure, even in patients without diabetes. In this review, I would like to summarize the extra-glycemic effects of anti-diabetic medications.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2024; 48(1): 83. CrossRef - To do one and to get more: Part I. Diabetes and bone
Wen-Ling Lee, Peng-Hui Wang, Szu-Ting Yang, Chia-Hao Liu, Wen-Hsun Chang, Fa-Kung Lee
Journal of the Chinese Medical Association.2022; 85(10): 965. CrossRef
- Association between underweight and risk of heart failure in diabetes patients

Original Articles
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
- Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
- Endocrinol Metab. 2022;37(2):281-289. Published online April 6, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1333
- 3,897 View
- 134 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
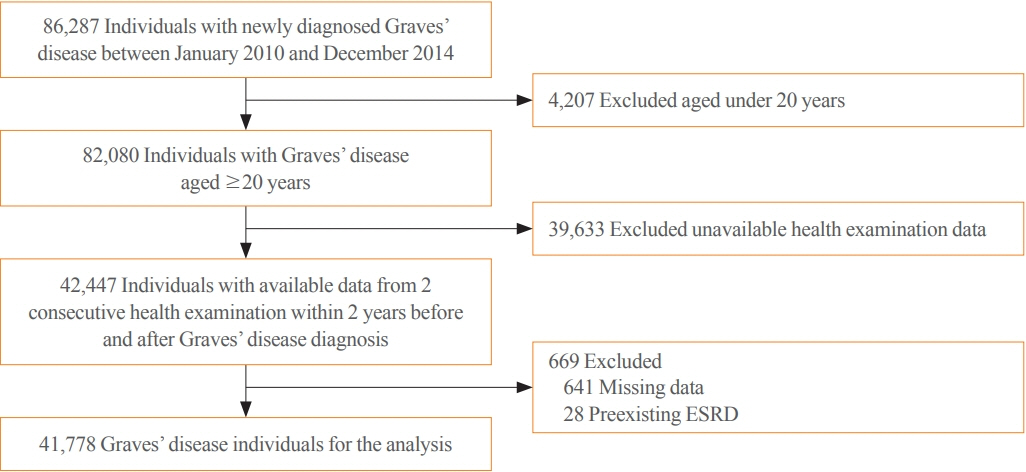
ePub - Background
Hyperthyroidism is associated with an increased glomerular filtration rate (GFR) in the hyperdynamic state, which is reversible after restoring euthyroidism. However, long-term follow-up of renal dysfunction in patients with hyperthyroidism has not been performed.
Methods
This was a retrospective cohort study using the Korean National Health Insurance database and biannual health checkup data. We included 41,778 Graves’ disease (GD) patients and 41,778 healthy controls, matched by age and sex. The incidences of end-stage renal disease (ESRD) were calculated in GD patients and controls. The cumulative dose and duration of antithyroid drugs (ATDs) were calculated for each patient and categorized into the highest, middle, and lowest tertiles.
Results
Among 41,778 GD patients, 55 ESRD cases occurred during 268,552 person-years of follow-up. Relative to the controls, regardless of smoking, drinking, or comorbidities, including chronic kidney disease, GD patients had a 47% lower risk of developing ESRD (hazard ratio [HR], 0.53; 95% confidence interval [CI], 0.37 to 0.76). In particular, GD patients with a higher baseline GFR (≥90 mL/min/1.73 m2; HR, 0.33; 95% CI, 0.11 to 0.99), longer treatment duration (>33 months; HR, 0.31; 95% CI, 0.17 to 0.58) or higher cumulative dose (>16,463 mg; HR, 0.29; 95% CI, 0.15 to 0.57) of ATDs had a significantly reduced risk of ESRD.
Conclusion
This was the first epidemiological study on the effect of GD on ESRD, and we demonstrated that GD population had a reduced risk for developing ESRD. -
Citations
Citations to this article as recorded by- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism
Magdy Mohamed Allam, Hanaa Tarek El-Zawawy, Tarek Hussein El-Zawawy
Endocrine.2023; 82(1): 78. CrossRef - Effect of Hyperthyroidism on Preventing Renal Insufficiency
Tae Yong Kim
Endocrinology and Metabolism.2022; 37(2): 220. CrossRef - Effects and Clinical Value of Peritoneal Dialysis on Water and Water Balance, Adverse Reactions, Quality of Life, and Clinical Prognosis in Patients with Decompensated Chronic Nephropathy: A Systematic Review and Meta-Analysis
Xichao Wang, Miaomiao Zhang, Na Sun, Wenxiu Chang, Gang Chen
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef
- Renal function changes in patients with subclinical hyperthyroidism: a novel postulated mechanism

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251

- 5,188 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience


 KES
KES

 First
First Prev
Prev



