Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2023;38(6):679-689. Published online December 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1760

- 1,219 View
- 66 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Limited longitudinal evidence exists regarding the potential association between smoking status and hip fracture among individuals with type 2 diabetes. We investigated this association using large-scale, nationwide cohort data for the Korean population.
Methods
This nationwide cohort study included 1,414,635 adults aged 40 and older who received Korean National Health Insurance Service health examinations between 2009 and 2012. Subjects with type 2 diabetes were categorized according to their smoking status, amount smoked (pack-years), number of cigarettes smoked per day, and duration of smoking. The results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between smoking status parameters and risk of hip fracture in multivariable Cox proportional hazard regression analysis.
Results
Compared with never-smokers, an increased adjusted HR (aHR) for hip fracture was observed in current smokers (1.681; 95% CI, 1.578 to 1.791), and a comparable aHR for hip fracture was found in former smokers (1.065; 95% CI, 0.999 to 1.136). For former smokers who had smoked 20 pack-years or more, the risk was slightly higher than that for never-smokers (aHR, 1.107; 95% CI, 1.024 to 1.196). The hip fracture risk of female former smokers was similar to that of female current smokers, but the hip fracture risk in male former smokers was similar to that of male never-smokers.
Conclusion
Smoking is associated with an increased risk of hip fracture in patients with type 2 diabetes. Current smokers with diabetes should be encouraged to quit smoking because the risk of hip fracture is greatly reduced in former smokers.

- Diabetes, obesity and metabolism
- The Impact of Taurine on Obesity-Induced Diabetes Mellitus: Mechanisms Underlying Its Effect
- Kainat Ahmed, Ha-Neul Choi, Jung-Eun Yim
- Endocrinol Metab. 2023;38(5):482-492. Published online October 17, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1776

- 2,807 View
- 163 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - This review explores the potential benefits of taurine in ameliorating the metabolic disorders of obesity and type 2 diabetes (T2D), highlighting the factors that bridge these associations. Relevant articles and studies were reviewed to conduct a comprehensive analysis of the relationship between obesity and the development of T2D and the effect of taurine on those conditions. The loss of normal β-cell function and development of T2D are associated with obesity-derived insulin resistance. The occurrence of diabetes has been linked to the low bioavailability of taurine, which plays critical roles in normal β-cell function, anti-oxidation, and anti-inflammation. The relationships among obesity, insulin resistance, β-cell dysfunction, and T2D are complex and intertwined. Taurine may play a role in ameliorating these metabolic disorders through different pathways, but further research is needed to fully understand its effects and potential as a therapeutic intervention.
-
Citations
Citations to this article as recorded by- Effect of a Very Low-Calorie Diet on Oxidative Stress, Inflammatory and Metabolomic Profile in Metabolically Healthy and Unhealthy Obese Subjects
Neus Bosch-Sierra, Carmen Grau-del Valle, Christian Salom, Begoña Zaragoza-Villena, Laura Perea-Galera, Rosa Falcón-Tapiador, Susana Rovira-Llopis, Carlos Morillas, Daniel Monleón, Celia Bañuls
Antioxidants.2024; 13(3): 302. CrossRef
- Effect of a Very Low-Calorie Diet on Oxidative Stress, Inflammatory and Metabolomic Profile in Metabolically Healthy and Unhealthy Obese Subjects

- Thyroid
Thyroid Cancer Screening - A Comprehensive Assessment of the Harms of Fine-Needle Aspiration Biopsy for Thyroid Nodules: A Systematic Review
- Ji Yong Park, Wonsuk Choi, A Ram Hong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2023;38(1):104-116. Published online February 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1669
- 3,777 View
- 162 Download
- 4 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There have concerns related with the potential harms of fine-needle aspiration biopsy (FNAB). We aimed to summarize the clinical complications and evaluate the safety of FNAB.
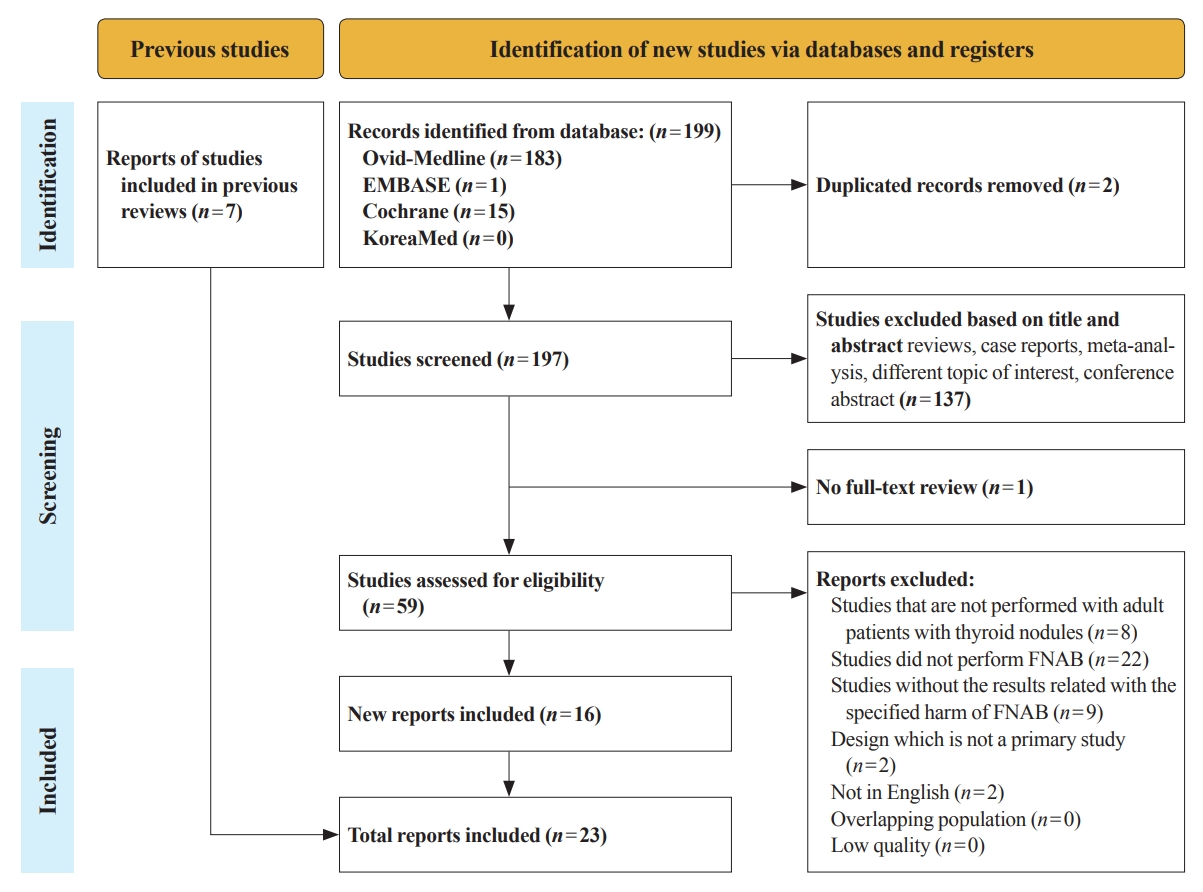
Methods
Studies related with the harms of FNAB were searched on MEDLINE, Embase, Cochrane library, and KoreaMed from 2012 to 2022. Also, studies reviewed in the previous systematic reviews were evaluated. Included clinical complications were postprocedural pain, bleeding events, neurological symptoms, tracheal puncture, infections, post-FNAB thyrotoxicosis, and needle tract implantation of thyroid cancers.
Results
Twenty-three cohort studies were included in this review. Nine studies which were related with FNAB-related pain showed that most of the subjects had no or mild discomfort. The 0% to 6.4% of the patients had hematoma or hemorrhage after FNAB, according to 15 studies. Vasovagal reaction, vocal cord palsy, and tracheal puncture have rarely described in the included studies. Needle tract implantation of thyroid malignancies was described in three studies reporting 0.02% to 0.19% of the incidence rate.
Conclusion
FNAB is considered to be a safe diagnostic procedure with rare complications, which are mainly minor events. Thorough assessement of the patients’ medical condition when deciding to perform FNABs would be advisable to lower potential complications. -
Citations
Citations to this article as recorded by- A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - Fine-needle aspiration cytology for neck lesions in patients with antithrombotic/anticoagulant medications: systematic review and meta-analysis
Dongbin Ahn, Ji Hye Kwak, Gill Joon Lee, Jin Ho Sohn
European Radiology.2024;[Epub] CrossRef - 2023 Update of the Korean Thyroid Association Guidelines for the Management of Thyroid Nodules
Eun Kyung Lee, Young Joo Park
Clinical Thyroidology®.2024; 36(4): 153. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Thyroid Cancer Screening: How to Maximize Its Benefits and Minimize Its Harms
Jung Hwan Baek
Endocrinology and Metabolism.2023; 38(1): 75. CrossRef - Evaluation of the Appropriateness of Thyroid Fine-Needle Aspiration
Lairce Cristina Ribeiro Brito, Iara Beatriz De Carvalho Botêlho, Lanna Matos Silva Fernandes, Nayze Lucena Sangreman Aldeman, Uziel Nunes Silva
International Journal for Innovation Education and Research.2023; 11(6): 8. CrossRef
- A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules

- Diabetes, Obesity and Metabolism
- Effect of the Concomitant Use of Subcutaneous Basal Insulin and Intravenous Insulin Infusion in the Treatment of Severe Hyperglycemic Patients
- Yejee Lim, Jung Hun Ohn, Joo Jeong, Jiwon Ryu, Sun-wook Kim, Jae Ho Cho, Hee-Sun Park, Hye Won Kim, Jongchan Lee, Eun Sun Kim, Nak-Hyun Kim, You Hwan Jo, Hak Chul Jang
- Endocrinol Metab. 2022;37(3):444-454. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1341
- 59,091 View
- 240 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
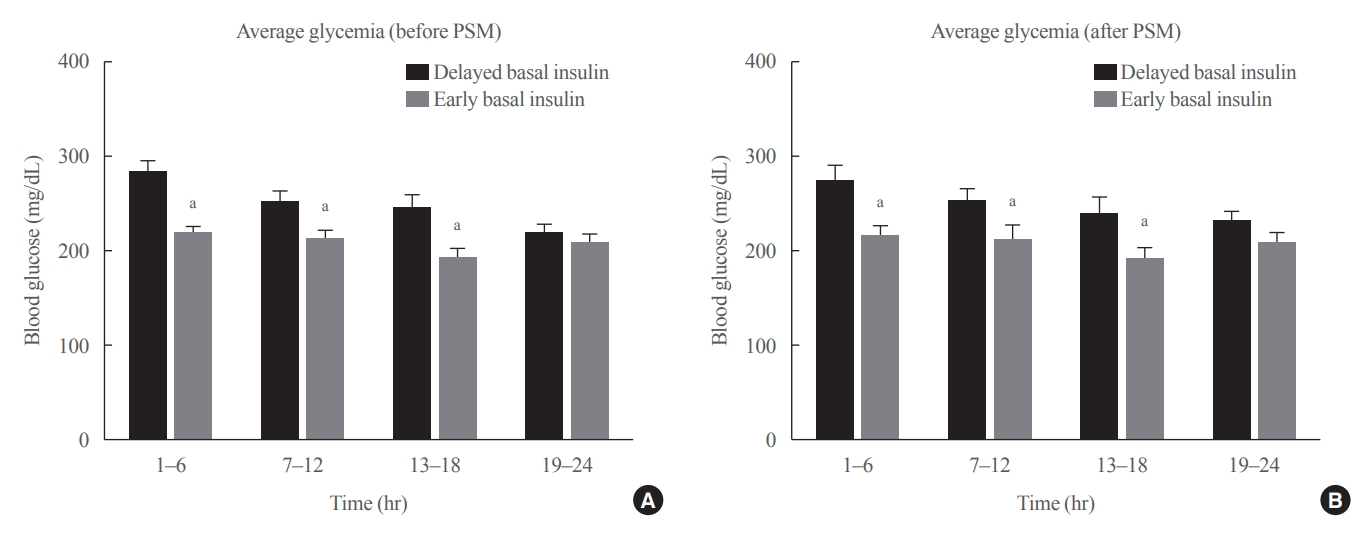
No consensus exists regarding the early use of subcutaneous (SC) basal insulin facilitating the transition from continuous intravenous insulin infusion (CIII) to multiple SC insulin injections in patients with severe hyperglycemia other than diabetic ketoacidosis. This study evaluated the effect of early co-administration of SC basal insulin with CIII on glucose control in patients with severe hyperglycemia.
Methods
Patients who received CIII for the management of severe hyperglycemia were divided into two groups: the early basal insulin group (n=86) if they received the first SC basal insulin 0.25 U/kg body weight within 24 hours of CIII initiation and ≥4 hours before discontinuation, and the delayed basal insulin group (n=79) if they were not classified as the early basal insulin group. Rebound hyperglycemia was defined as blood glucose level of >250 mg/dL in 24 hours following CIII discontinuation. Propensity score matching (PSM) methods were additionally employed for adjusting the confounding factors (n=108).
Results
The rebound hyperglycemia incidence was significantly lower in the early basal insulin group than in the delayed basal insulin group (54.7% vs. 86.1%), despite using PSM methods (51.9%, 85.2%). The length of hospital stay was shorter in the early basal insulin group than in the delayed basal insulin group (8.5 days vs. 9.6 days, P=0.027). The hypoglycemia incidence did not differ between the groups.
Conclusion
Early co-administration of basal insulin with CIII prevents rebound hyperglycemia and shorten hospital stay without increasing the hypoglycemic events in patients with severe hyperglycemia. -
Citations
Citations to this article as recorded by- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Laya Ekhlaspour, Rodolfo J. Galindo, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Mary Lou Perry, Scott J.
Diabetes Care.2024; 47(Supplement): S295. CrossRef - 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2023
Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer, Billy S. Collins, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary Lou Perry, Priya
Diabetes Care.2023; 46(Supplement): S267. CrossRef - Effectiveness and safety of early insulin glargine administration in combination with continuous intravenous insulin infusion in the management of diabetic ketoacidosis: A randomized controlled trial
Kitti Thammakosol, Chutintorn Sriphrapradang
Diabetes, Obesity and Metabolism.2023; 25(3): 815. CrossRef
- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024

- Clinical Study
- Association of Vitamin D Deficiency with Diabetic Nephropathy
- So-hyeon Hong, Young Bin Kim, Hoon Sung Choi, Tae-Dong Jeong, Jin Taek Kim, Yeon Ah Sung
- Endocrinol Metab. 2021;36(1):106-113. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.826
- 8,510 View
- 226 Download
- 22 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
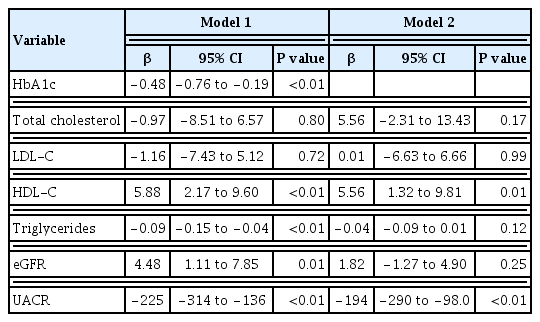
Low 25-hydroxyvitamin D (25OHD) levels are associated with the incidence of type 2 diabetes mellitus (T2DM). However, the association between 25OHD and metabolic health status or diabetic complications is inconclusive. We evaluated this relationship between vitamin D status and metabolic parameters and complications of T2DM.
Methods
This study included 1,392 patients with T2DM who visited Eulji and Ewha Diabetes Center between January 2011 and August 2016. Anthropometric parameters and laboratory tests including glycated hemoglobin (HbA1c), lipid profile, liver and kidney function, and urinary albumin-to-creatinine ratio (UACR) were evaluated. Diabetic macro- and microvascular complications were determined through a medical record review. Serum 25OHD concentrations were measured by chemiluminescent immunoassay.
Results
The mean 25OHD level was 16.8±9.6 ng/mL. Vitamin D deficiency (<20 ng/mL) and severe deficiency (<10 ng/mL) were observed in 990 (71.1%) and 351 (25.2%) participants, respectively. 25OHD level was positively correlated with age and highdensity lipoprotein cholesterol (HDL-C) level and negatively correlated with HbA1c, triglyceride level, and UACR. HDL-C and UACR were significantly associated with 25OHD after adjusting for other variables. Vitamin D deficiency was independently related to nephropathy after adjusting for confounding variables.
Conclusion
Vitamin D deficiency was common among Korean T2DM patients; it was independently associated with microalbuminuria and HDL level, and positively related to diabetic nephropathy. -
Citations
Citations to this article as recorded by- ED-71 ameliorates bone regeneration in type 2 diabetes by reducing ferroptosis in osteoblasts via the HIF1α pathway
Maoshan Wang, Yingxue Liu, Houda Gui, Gaoqiang Ma, Binyang Li, Zhanwei Zhang, Gyeonghwi Yu, Ailin Wu, Xin Xu, Dongjiao Zhang
European Journal of Pharmacology.2024; 969: 176303. CrossRef - Vitamin D metabolism in diabetic nephropathy
Z. V. Abilov, R. Kh. Salimkhanov, A. A. Povaliaeva, A. Yu. Zhukov, E. A. Pigarova, L. K. Dzeranova, L. Ya. Rozhinskaya
Obesity and metabolism.2024; 20(4): 283. CrossRef - COVID-19 infection and metabolic comorbidities: Mitigating role of nutritional sufficiency and drug – nutraceutical combinations of vitamin D
Sumit Kumar Mandal, Meghana Tare, P.R. Deepa
Human Nutrition & Metabolism.2023; 31: 200179. CrossRef - Effects of Vitamin D Supplementation in Diabetic Kidney Disease: A Systematic Review
Thais de Oliveira e Silva Ullmann, Beatrys Juliani Ramalho, Lucas Fornari Laurindo, Ricardo José Tofano, Claudio José Rubira, Elen Landgraf Guiguer, Sandra Maria Barbalho, Uri Adrian Prync Flato, Katia Portero Sloan, Adriano Cressoni Araujo
Journal of Renal Nutrition.2023; 33(5): 618. CrossRef - Diabetic Nephropathy: Significance of Determining Oxidative Stress and Opportunities for Antioxidant Therapies
Marina Darenskaya, Sergey Kolesnikov, Natalya Semenova, Lyubov Kolesnikova
International Journal of Molecular Sciences.2023; 24(15): 12378. CrossRef - Association between serum 25- hydroxyvitamin D and albuminuiria in middle-aged and older Chinese patients with type 2 diabetes
Luyan Zhang, Qian Guo, Yanjia Xu, Wenzhen Wei, Yu Wang
BMC Endocrine Disorders.2023;[Epub] CrossRef - Vitamin D deficiency and its associated factors among patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Mitku Mammo Taderegew, Gashaw Garedew Woldeamanuel, Alemayehu Wondie, Atsede Getawey, Abera Nesiru Abegaz, Fentahun Adane
BMJ Open.2023; 13(10): e075607. CrossRef - Progression of diabetic nephropathy and vitamin D serum levels: A pooled analysis of 7722 patients
Yomna E. Dean, Sameh Samir Elawady, Wangpan Shi, Ahmed A. Salem, Arinnan Chotwatanapong, Haya Ashraf, Tharun Reddi, Prashant Obed Reddy Dundi, Waleed Yasser Habash, Mohamed Yasser Habash, Safaa Ahmed, Hana M. Samir, Ahmed Elsayed, Aryan Arora, Abhinav Aro
Endocrinology, Diabetes & Metabolism.2023;[Epub] CrossRef - Incidence of Vitamin D Deficiency and Its Association With Microalbuminuria in Patients With Type 2 Diabetes Mellitus
Muhammad Hamza Riaz, Ammar Jamil, Hira Yousaf, Muhammad Hassan, Muhammad Ahmer Sohaib, Sharjeel Babar, Muhammad Hassan Ahmad, Ibtesam Allahi, Muhammad Zeshan Mehmood, Tayyab Mumtaz Khan
Cureus.2023;[Epub] CrossRef - The Role of Vitamin D in Diabetic Nephropathy: A Translational Approach
Charlotte Delrue, Reinhart Speeckaert, Joris R. Delanghe, Marijn M. Speeckaert
International Journal of Molecular Sciences.2022; 23(2): 807. CrossRef - Associations of serum amyloid A and 25‐hydroxyvitamin D with diabetic nephropathy: A cross‐sectional study
Qian Liu, Jin Sun, Tongdao Xu, Guangrong Bian, Fumeng Yang
Journal of Clinical Laboratory Analysis.2022;[Epub] CrossRef - Formulation Strategies for Improving the Stability and Bioavailability of Vitamin D-Fortified Beverages: A Review
Elsa F. Vieira, Suene Souza
Foods.2022; 11(6): 847. CrossRef - Association between Vitamin D Status and Mortality among Adults with Diabetic Kidney Disease
Feng Xu, Hongyu Lu, Tianwen Lai, Ling Lin, Yongsong Chen, Pratibha V. Nerurkar
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Assessment of the relationship between 25-hydroxyvitamin D and albuminuria in type 2 diabetes mellitus
Seyed Alireza Zomorodian, Maryam Shafiee, Zeinab Karimi, Fatemeh Masjedi, Amirhossein Roshanshad
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association of Serum 25 (OH) Vitamin D With Chronic Kidney Disease Progression in Type 2 Diabetes
Suyan Duan, Fang Lu, Buyun Wu, Chengning Zhang, Guangyan Nie, Lianqin Sun, Zhimin Huang, Honglei Guo, Bo Zhang, Changying Xing, Yanggang Yuan
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Influence of Dietary Supplementations on Neuropathic Pain
Francesco D’Egidio, Giorgia Lombardozzi, Housem E. Kacem Ben Haj M’Barek, Giada Mastroiacovo, Margherita Alfonsetti, Annamaria Cimini
Life.2022; 12(8): 1125. CrossRef - Emergence of Ectopic Adrenal Tissues-What are the Probable Mechanisms?
Gürkan Tarçın, Oya Ercan
Journal of Clinical Research in Pediatric Endocrinology.2022; 14(3): 258. CrossRef - Nutritional Supplements for the Treatment of Neuropathic Pain
Khaled M. Abdelrahman, Kevin V. Hackshaw
Biomedicines.2021; 9(6): 674. CrossRef - Vitamin D Deficiency as a Predictor of a High Prevalence of Coronary Artery Disease in Pancreas Transplant Candidates With Type 1 Diabetes
Małgorzata Buksińska-Lisik, Przemysław J. Kwasiborski, Robert Ryczek, Wojciech Lisik, Artur Mamcarz
Frontiers in Endocrinology.2021;[Epub] CrossRef - Serum 25-hydroxyvitamin D and Metabolic Parameters in Healthy Korean Adults: Korean National Health and Nutrition Examination Survey VI
Jeonghoon Ha, Hansang Baek, Chaiho Jeong, Hyunsam Kim, Ki-Hyun Baek, Moo Il Kang, Dong-Jun Lim
International Journal of General Medicine.2021; Volume 14: 5233. CrossRef - Association Between 25(OH)Vitamin D, HbA1c and Albuminuria in Diabetes Mellitus: Data From a Population-Based Study (VIDAMAZON)
João Soares Felício, Hana Andrade de Rider Britto, Pedro Celeira Cortez, Fabrício de Souza Resende, Manuela Nascimento de Lemos, Lorena Vilhena de Moraes, Vitória Teixeira de Aquino, Fernanda de Souza Parente, Natércia Neves Marques de Queiroz, João Felíc
Frontiers in Endocrinology.2021;[Epub] CrossRef - Vitamin D Analogs Can Retard the Onset or Progression of Diabetic Kidney Disease: A Systematic Review
Samuel N. Uwaezuoke
Frontiers in Clinical Diabetes and Healthcare.2021;[Epub] CrossRef
- ED-71 ameliorates bone regeneration in type 2 diabetes by reducing ferroptosis in osteoblasts via the HIF1α pathway

- Clinical Study
- Revisiting Rupture of Benign Thyroid Nodules after Radiofrequency Ablation: Various Types and Imaging Features
- Sae Rom Chung, Jung Hwan Baek, Jin Yong Sung, Ji Hwa Ryu, So Lyung Jung
- Endocrinol Metab. 2019;34(4):415-421. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.415
- 5,828 View
- 96 Download
- 22 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background To evaluate the imaging features, clinical manifestations, and prognosis of patients with thyroid nodule rupture after radiofrequency ablation (RFA).
Methods The records of 12 patients who experienced thyroid nodule rupture after RFA at four Korean thyroid centers between March 2010 and July 2017 were retrospectively reviewed. Clinical data evaluated included baseline patient characteristics, treatment methods, initial presenting symptoms, imaging features, treatment, and prognosis.
Results The most common symptoms of post-RFA nodule rupture were sudden neck bulging and pain. Based on imaging features, the localization of nodule rupture was classified into three types: anterior, posterolateral, and medial types. The anterior type is the most often, followed by posterolateral and medial type. Eight patients recovered completely after conservative treatment. Four patients who did not improve with conservative management required invasive procedures, including incision and drainage or aspiration.
Conclusion Thyroid nodule rupture after RFA can be classified into three types based on its localization: anterior, posterolateral, and medial types. Because majority of thyroid nodule ruptures after RFA can be managed conservatively, familiarity with these imaging features is essential in avoiding unnecessary imaging workup or invasive procedures.
-
Citations
Citations to this article as recorded by- Assessing the efficacy of thyroid nodule radiofrequency ablation using patient-reported outcome measures
Ege Akgun, Gustavo Romero-Velez, Eren Berber
Surgery.2024; 175(3): 654. CrossRef - The Comparison of Efficacy and Safety between Radiofrequency Ablation Alone and Ethanol Ablation Followed by Radiofrequency Ablation in the Treatment of Mixed Cystic and Solid Thyroid Nodule
Min Gang Jo, Min Kyoung Lee, Jae Ho Shin, Min Guk Seo, So Lyung Jung
Journal of the Korean Society of Radiology.2024;[Epub] CrossRef - Cutaneous fistula formation after thyroid nodule rupture: A rare complication after radiofrequency ablation
Amanda J. Bastien, Luv Amin, Jeffrey Moses, Wendy Sacks, Allen S. Ho
Head & Neck.2024;[Epub] CrossRef - Thyroid nodule rupture after radiofrequency ablation: case report and literature review
Tatiana Ferraro, Sameeha Sajid, Steven P. Hodak, Chelsey K. Baldwin
Frontiers in Endocrinology.2024;[Epub] CrossRef - Radiofrequency Ablation for Benign Thyroid Nodules: Radiology In Training
Ningcheng Li, Timothy C. Huber
Radiology.2023; 306(1): 54. CrossRef - A Case of Thyroid Abscess Following Ethanol Ablation for Benign Thyroid Nodule
Heungrae Cho, Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2023; 66(9): 624. CrossRef - Radiofrequency Ablation for Benign Thyroid Nodules
Julia E Noel, Catherine F Sinclair
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): e12. CrossRef - 2022 Taiwan clinical multicenter expert consensus and recommendations for thyroid radiofrequency ablation
Wei-Che Lin, Wen-Chieh Chen, Pei-Wen Wang, Yi-Chia Chan, Yen-Hsiang Chang, Harn-Shen Chen, Szu-Tah Chen, Wei-Chih Chen, Kai-Lun Cheng, Shun-Yu Chi, Pi-Ling Chiang, Chen-Kai Chou, Feng-Fu Chou, Shun-Chen Huang, Feng-Hsuan Liu, Sheng-Dean Luo, Fen-Yu Tseng,
Ultrasonography.2023; 42(3): 357. CrossRef - Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
Jin Yong Sung
Journal of the Korean Society of Radiology.2023; 84(5): 985. CrossRef - General Principles for the Safe Performance, Training, and Adoption of Ablation Techniques for Benign Thyroid Nodules: An American Thyroid Association Statement
Catherine F. Sinclair, Jung Hwan Baek, Kathleen E. Hands, Steven P. Hodak, Timothy C. Huber, Iram Hussain, Brian Hung-Hin Lang, Julia E. Noel, Maria Papaleontiou, Kepal N. Patel, Gilles Russ, Jonathon Russell, Stefano Spiezia, Jennifer H. Kuo
Thyroid®.2023; 33(10): 1150. CrossRef - Radiofrequency ablation and thyroid cancer: review of the current literature
Haris Muhammad, Aniqa Tehreem, Jonathon O. Russell
American Journal of Otolaryngology.2022; 43(1): 103204. CrossRef - Microwave Ablation Vs Traditional Thyroidectomy for Benign Thyroid Nodules: A Prospective, Non-Randomized Cohort Study
Shaokun Li, Mingfeng Yang, Haipeng Guo, Muyuan Liu, Shaowei Xu, Hanwei Peng
Academic Radiology.2022; 29(6): 871. CrossRef - Radiofrequency ablation and related ultrasound‐guided ablation technologies for treatment of benign and malignant thyroid disease: An international multidisciplinary consensus statement of the American Head and Neck Society Endocrine Surgery Section with
Lisa A. Orloff, Julia E. Noel, Brendan C. Stack, Marika D. Russell, Peter Angelos, Jung Hwan Baek, Kevin T. Brumund, Feng‐Yu Chiang, Mary Beth Cunnane, Louise Davies, Andrea Frasoldati, Anne Y. Feng, Laszlo Hegedüs, Ayaka J. Iwata, Emad Kandil, Jennifer K
Head & Neck.2022; 44(3): 633. CrossRef - Thyroid Nodule Radiofrequency Ablation: Complications and Clinical Follow Up
James Y. Lim, Jennifer H. Kuo
Techniques in Vascular and Interventional Radiology.2022; 25(2): 100824. CrossRef - Minimally-invasive treatments for benign thyroid nodules: recommendations for information to patients and referring physicians by the Italian Minimally-Invasive Treatments of the Thyroid group
Giovanni Mauri, Stella Bernardi, Andrea Palermo, Roberto Cesareo, Enrico Papini, Luigi Solbiati, Daniele Barbaro, Salvatore Monti, Maurilio Deandrea, Laura Fugazzola, Giovanni Gambelunghe, Roberto Negro, Stefano Spiezia, Fulvio Stacul, Luca Maria Sconfien
Endocrine.2022; 76(1): 1. CrossRef - American Association of Clinical Endocrinology Disease State Clinical Review: The Clinical Utility of Minimally Invasive Interventional Procedures in the Management of Benign and Malignant Thyroid Lesions
Sina Jasim, Kepal N. Patel, Gregory Randolph, Stephanie Adams, Roberto Cesareo, Edward Condon, Tara Henrichsen, Malak Itani, Maria Papaleontiou, Leonardo Rangel, John Schmitz, Marius N. Stan
Endocrine Practice.2022; 28(4): 433. CrossRef - Radiofrequency Ablation of Benign and Malignant Thyroid Nodules
Patrick J. Navin, Scott M. Thompson, Anil N. Kurup, Robert A. Lee, Matthew R. Callstrom, M. Regina Castro, Marius N. Stan, Brian T. Welch, John J. Schmitz
RadioGraphics.2022; 42(6): 1812. CrossRef - SFE-AFCE-SFMN 2022 consensus on the management of thyroid nodules: Thermal ablation
Adrien Ben Hamou, Edouard Ghanassia, Arnaud Muller, Miriam Ladsous, Nunzia Cinzia Paladino, Laurent Brunaud, Laurence Leenhardt, Gilles Russ
Annales d'Endocrinologie.2022; 83(6): 423. CrossRef - Complications of RFA for Thyroid Nodules: Prevention and Management
Rahul K. Sharma, Jennifer H Kuo
Current Otorhinolaryngology Reports.2021; 9(1): 79. CrossRef - Ultrasonographic characteristics of thyroid nodule rupture after microwave ablation
Peng Tian, Wenyan Du, Xiaoxi Liu, Yiwen Ding, Zekai Zhang, Jing Li, Yanzhen Wang
Medicine.2021; 100(9): e25070. CrossRef - Symptomatic aseptic necrosis of benign thyroid lesions after microwave ablation: risk factors and clinical significance
Jian-ping Dou, Jie Yu, Zhi-gang Cheng, Fang-yi Liu, Xiao-ling Yu, Qi-di Hou, Fang Liu, Zhi-yu Han, Ping Liang
International Journal of Hyperthermia.2021; 38(1): 815. CrossRef - The Importance of Nodule Size in the Management of Ruptured Thyroid Nodule After Radiofrequency Ablation: A Retrospective Study and Literature Review
Wen-Chieh Chen, Sheng-Dean Luo, Wei-Chih Chen, Chen-Kai Chou, Yen-Hsiang Chang, Kai-Lun Cheng, Wei-Che Lin
Frontiers in Endocrinology.2021;[Epub] CrossRef - Long-Term Follow-Up of Single-Fiber Multiple Low-Intensity Energy Laser Ablation Technique of Benign Thyroid Nodules
Mattia Squarcia, Mireia Mora, Gloria Aranda, Enrique Carrero, Daniel Martínez, Ramona Jerez, Ricard Valero, Joan Berenguer, Irene Halperin, Felicia A. Hanzu
Frontiers in Oncology.2021;[Epub] CrossRef - Effectiveness of Injecting Cold 5% Dextrose into Patients with Nerve Damage Symptoms during Thyroid Radiofrequency Ablation
Min Kyoung Lee, Jung Hwan Baek, Sae Rom Chung, Young Jun Choi, Yu-Mi Lee, Tae Yong Kim, Jeong Hyun Lee
Endocrinology and Metabolism.2020; 35(2): 407. CrossRef
- Assessing the efficacy of thyroid nodule radiofrequency ablation using patient-reported outcome measures

- Complication and Prognosis of Craniopharyngioma According to the Age of Onset.
- Eun Jig Lee, Moon Suk Nam, Young Duk Song, Sung Kil Lim, Hyun Chul Lee, Kap Bum Huh, Kyung Rae Kim, Kun Hoon Song, Bong Soo Cha, Ji Hyun Lee
- J Korean Endocr Soc. 1994;10(3):262-272. Published online November 6, 2019
- 1,109 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Craniopharyngioma is the most common tumor involving the hypothalamo-pituitary area in childhood and adolescence. Recently, we carried out collective review of 70 patients with craniopharyngioma treated from January 1980 to December 1994 in order to inverstigate the endocrine outcome and survival according to the age of onset.The following results were obtained:1) The male to female ratio was 1:1. Age at diagnosis ranged from 2 to 64 years(mean age: 23) with the greatest frequency in the 2nd decade of life(28.6%). Of the 70 cases, the first group, 27 cases were under the age of 15, and the other group, 43 cases were over 15 year-old.2) The most common symptom at diagnosis in both groups was headache. In the adult group, symptoms related to hypogonadism(amenorrhea, decreased libido, galactorrhea etc.) were not uncommon. The lag of time between onset of symptom and hospital visit ranged from 3 days to 156 months(mean: 20 months).3) The main site of tumor was suprasellar region in both groups. The most common CT finding in both groups was calcification in sella turcica.4) In pre-operative combined pituitary function test, the most common, abnormal responses were shown in growth hormone and thyroid stimulating hormone in both groups. In addition, prolactin frequently showed abnormal response in the adult group.In post-operative combined pituitary function test, more hormones tended to reveal abnormal response in the group treated with surgery plus radiation therapy.5) The operation by subtotal removal followed by radiation therapy was the most commonly used method in treatment of both groups. After treatment, panhypopituitarism was occurred more frequently in the group treated with RT after surgery than those treated with surgery alone, but the difference was not statistically significant(p=0.136 in childhood, 0.436 in adults). Except the cases with panhypopituitarism, the most commonly encountered endocrine abnormalities were growth retardation in the children group, and hypogonadism in adult. The recurrence was clinically observed in 11 cases. The recurrence rate were 11.1% in children, and 18.6% in adult respectively. The mean time from the initial treatment to recurrence was 23 months. There was no significant difference in recurrence rate between the group treated with RT after subtotal removal and the group treated with total removal(p=0.475).The overall five-year survival rate after treatment was 82.8%. According to the treatment modalities, the patients undergone RT after subtotal removal survived much longer than those treated with other modalities such as subtotal removal only or total removal, but the differences in survival were not statistically significant(Log rank test, p=0.0539).

- Clinical Study
- Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea
- Da Hea Seo, Shinae Kang, Yong-ho Lee, Jung Yoon Ha, Jong Suk Park, Byoung-Wan Lee, Eun Seok Kang, Chul Woo Ahn, Bong-Soo Cha
- Endocrinol Metab. 2019;34(3):282-290. Published online September 26, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.3.282
- 6,008 View
- 87 Download
- 15 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background This study investigated the overall status of diabetes control and screening for diabetic microvascular complications in patients with type 2 diabetes mellitus attending primary care clinics in Korea.
Methods In this cross-sectional observational study, 191 primary care clinics were randomly selected across Korea from 2015 to 2016. In total, 3,227 subjects were enrolled in the study.
Results The patients followed at the primary care clinics were relatively young, with a mean age of 61.4±11.7 years, and had a relatively short duration of diabetes (mean duration, 7.6±6.5 years). Approximately 14% of subjects had diabetic microvascular complications. However, the patients treated at the primary care clinics had suboptimal control of hemoglobin A1c levels, blood pressure, and serum lipid levels, along with a metabolic target achievement rate of 5.9% according to the Korean Diabetes Association guidelines. The screening rates for diabetic nephropathy, retinopathy, and neuropathy within the past 12 months were 28.4%, 23.3%, and 13.3%, respectively.
Conclusion The overall status of diabetes management, including the frequency of screening for microvascular complications, was suboptimal in the primary care clinics. More efforts should be made and more resources need to be allocated for primary care physicians to promote adequate healthcare delivery, which would result in stricter diabetes control and improved management of diabetic complications.
-
Citations
Citations to this article as recorded by- Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(6): 837. CrossRef - Effectiveness of quality of care for patients with type 2 diabetes in China: findings from the Shanghai Integration Model (SIM)
Chun Cai, Yuexing Liu, Yanyun Li, Yan Shi, Haidong Zou, Yuqian Bao, Yun Shen, Xin Cui, Chen Fu, Weiping Jia
Frontiers of Medicine.2022; 16(1): 126. CrossRef - Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study
Hee-Chung Kang, Jae-Seok Hong
Healthcare.2022; 10(2): 334. CrossRef - Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Type 2 Diabetes Mellitus with Early Dry Skin Disorder: A Comparison Study Between Primary and Tertiary Care in Indonesia
Lili Legiawati, Kusmarinah Bramono, Wresti Indriatmi, Em Yunir, Aditya Indra Pratama
Current Diabetes Reviews.2022;[Epub] CrossRef - Long-Term Changes in HbA1c According to Blood Glucose Control Status During the First 3 Months After Visiting a Tertiary University Hospital
Hyunah Kim, Da Young Jung, Seung-Hwan Lee, Jae-Hyoung Cho, Hyeon Woo Yim, Hun-Sung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Effects of Diabetes Quality Assessment on Diabetes Management Behaviors Based on a Nationwide Survey
Chang Kyun Choi, Jungho Yang, Ji-An Jeong, Min-Ho Shin
International Journal of Environmental Research and Public Health.2022; 19(23): 15781. CrossRef - The Impact of the Indonesian Chronic Disease Management Program (PROLANIS) on Metabolic Control and Renal Function of Type 2 Diabetes Mellitus Patients in Primary Care Setting
Firas Farisi Alkaff, Fauzan Illavi, Sovia Salamah, Wiwit Setiyawati, Ristra Ramadhani, Elly Purwantini, Dicky L. Tahapary
Journal of Primary Care & Community Health.2021; 12: 215013272098440. CrossRef - Questionnaire-based Survey of Demographic and Clinical Characteristics, Health Behaviors, and Mental Health of Young Korean Adults with Early-Onset Diabetes
Ji In Park, Hyunjeong Baek, Sang-Wook Kim, Ji Yun Jeong, Kee-Ho Song, Ji Hee Yu, Il Sung Nam-Goong, Eun-Hee Cho
Journal of Korean Medical Science.2021;[Epub] CrossRef - Sodium–Glucose Cotransporter 2 Inhibitors and Risk of Retinal Vein Occlusion Among Patients With Type 2 Diabetes: A Propensity Score–Matched Cohort Study
Min-Kyung Lee, Bongsung Kim, Kyungdo Han, Jae-Hyuk Lee, Minhee Kim, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon, Young-Jung Roh
Diabetes Care.2021; 44(10): 2419. CrossRef - Challenges in the Management of Diabetes in Primary Care
Yeon Kyung Lee
The Journal of Korean Diabetes.2020; 21(3): 161. CrossRef - Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
Sung-Youn Chun, Dong Wook Kim, Sang Ah Lee, Su Jung Lee, Jung Hyun Chang, Yoon Jung Choi, Seong Woo Kim, Sun Ok Song
Diabetes & Metabolism Journal.2020; 44(6): 897. CrossRef - Comprehensive Efforts Are Needed to Improve the Quality of Primary Diabetes Care in Korea
Chan-Hee Jung
Endocrinology and Metabolism.2019; 34(3): 265. CrossRef
- Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study

- Diabetes
- Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
- Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
- Endocrinol Metab. 2019;34(1):80-92. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.80
- 7,665 View
- 267 Download
- 36 Web of Science
- 38 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background To investigate the effects of dipeptidyl peptidase-4 (DPP-4) inhibitors on renal outcomes in patients with type 2 diabetes.
Methods MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials were searched to identify randomized controlled trials (RCTs) of DPP-4 inhibitors from inception to September 2017. We selected eligible RCTs comparing DPP-4 inhibitors with placebo or other antidiabetic agents and reporting at least one renal outcome. A meta-analysis was conducted to calculate standardized mean differences, weighted mean differences (WMDs), relative risks (RRs), and 95% confidence intervals (CIs) for each renal outcome.
Results We included 23 RCTs with 19 publications involving 41,359 patients. Overall changes in urine albumin-to-creatinine ratio were comparable between DPP-4 inhibitors and controls (
P =0.150). However, DPP-4 inhibitors were associated with significantly lower risk of incident microalbuminuria (RR, 0.89; 95% CI, 0.80 to 0.98;P =0.022) and macroalbuminuria (RR, 0.77; 95% CI, 0.61 to 0.97;P =0.027), as well as higher rates of regression of albuminuria (RR, 1.22; 95% CI, 1.10 to 1.35;P <0.001) compared with controls. Although DPP-4 inhibitors were associated with small but significantly lower estimated glomerular filtration rate (WMD, −1.11 mL/min/1.73 m2; 95% CI, −1.78 to −0.44;P =0.001), there was no difference in the risk of end-stage renal disease between two groups (RR, 0.93; 95% CI, 0.76 to 1.14;P =0.475).Conclusion DPP-4 inhibitors had beneficial renal effects mainly by reducing the risk of development or progression of albuminuria compared with placebo or other antidiabetic agents.
-
Citations
Citations to this article as recorded by- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study
Mototsugu Nagao, Jun Sasaki, Kyoko Tanimura-Inagaki, Ichiro Sakuma, Hitoshi Sugihara, Shinichi Oikawa
Cardiovascular Diabetology.2024;[Epub] CrossRef - Effects of glucose‐lowering agents on cardiovascular and renal outcomes in subjects with type 2 diabetes: An updated meta‐analysis of randomized controlled trials with external adjudication of events
Edoardo Mannucci, Marco Gallo, Andrea Giaccari, Riccardo Candido, Basilio Pintaudi, Giovanni Targher, Matteo Monami
Diabetes, Obesity and Metabolism.2023; 25(2): 444. CrossRef - Sitagliptin Mitigates Diabetic Nephropathy in a Rat Model of Streptozotocin-Induced Type 2 Diabetes: Possible Role of PTP1B/JAK-STAT Pathway
Sarah M. AL-Qabbaa, Samaher I. Qaboli, Tahani K. Alshammari, Maha A. Alamin, Haya M. Alrajeh, Lama A. Almuthnabi, Rana R. Alotaibi, Asma S. Alonazi, Anfal F. Bin Dayel, Nawal M. Alrasheed, Nouf M. Alrasheed
International Journal of Molecular Sciences.2023; 24(7): 6532. CrossRef - Take an individualized and multipronged approach when managing older adults with type 2 diabetes
Sheridan M. Hoy
Drugs & Therapy Perspectives.2023; 39(5): 171. CrossRef - Cardiovascular and Renal Outcomes With Sodium-Glucose Cotransporter-2 Inhibitors and Dipeptidyl Peptidase-4 Inhibitors Combination Therapy: A Meta-Analysis of Randomized Cardiovascular Outcome Trials
Awadhesh Kumar Singh, Akriti Singh, Ritu Singh
Endocrine Practice.2023; 29(7): 509. CrossRef - Sodium‐glucose cotransporter 2 inhibitors versus dipeptidyl peptidase 4 inhibitors on new‐onset overall cancer in Type 2 diabetes mellitus: A population‐based study
Cheuk To Chung, Ishan Lakhani, Oscar Hou In Chou, Teddy Tai Loy Lee, Edward Christopher Dee, Kenrick Ng, Wing Tak Wong, Tong Liu, Sharen Lee, Qingpeng Zhang, Bernard Man Yung Cheung, Gary Tse, Jiandong Zhou
Cancer Medicine.2023; 12(11): 12299. CrossRef - Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes
Deborah J. Wexler, Ian H. de Boer, Alokananda Ghosh, Naji Younes, Ionut Bebu, Silvio E. Inzucchi, Janet B. McGill, Sunder Mudaliar, David Schade, Michael W. Steffes, William V. Tamborlane, Meng H. Tan, Faramarz Ismail-Beigi, Jill P. Crandall, Melissa Dian
JAMA Internal Medicine.2023; 183(7): 705. CrossRef - SAFETY PROFILE OF DIPEPTIDYL PEPTIDASE-4 INHIBITORS
M. Ganeva
Trakia Journal of Sciences.2023; 21(1): 54. CrossRef - Chronic Kidney Disease and SGLT2 Inhibitors: A Review of the Evolving Treatment Landscape
Christian W. Mende
Advances in Therapy.2022; 39(1): 148. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Pharmacoeconomic evaluation of dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes mellitus: a systematic literature review
Zhen Ruan, Huimin Zou, Qing Lei, Carolina Oi Lam Ung, Honghao Shi, Hao Hu
Expert Review of Pharmacoeconomics & Outcomes Research.2022; : 1. CrossRef - Effect of Anagliptin versus Sitagliptin on Renal Function: Subanalyzes from the REASON Trial
Hiroki Teragawa, Takeshi Morimoto, Yuichi Fujii, Tomohiro Ueda, Mio Sakuma, Michio Shimabukuro, Osamu Arasaki, Koichi Node, Takashi Nomiyama, Shinichiro Ueda
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 685. CrossRef - Glomerular filtration rate as a kidney outcome of diabetic kidney disease: a focus on new antidiabetic drugs
Hyo Jin Kim, Sang Soo Kim, Sang Heon Song
The Korean Journal of Internal Medicine.2022; 37(3): 502. CrossRef - The Effects of Dipeptidyl Peptidase 4 Inhibitors on Renal Function in Patients with Type 2 Diabetes Mellitus
Wan-Chia Hsu, Chun-Sheng Lin, Jung-Fu Chen, Chih-Min Chang
Journal of Clinical Medicine.2022; 11(9): 2653. CrossRef - Treatment of diabetes mellitus has borne much fruit in the prevention of cardiovascular disease
Hiroaki Yagyu, Hitoshi Shimano
Journal of Diabetes Investigation.2022; 13(9): 1472. CrossRef - Finerenone, a Novel and Safer Approach toward Management of Diabetic Kidney Disease with Heart Failure
Ayesha Abdul Qadir Memon, Sarmad Iqbal
Global Journal of Medical, Pharmaceutical, and Biomedical Update.2022; 17: 12. CrossRef - The effects of dipeptidyl peptidase‐4 inhibitors on kidney outcomes
Daniel V. O'Hara, Thomas R. Parkhill, Sunil V. Badve, Min Jun, Meg J. Jardine, Vlado Perkovic
Diabetes, Obesity and Metabolism.2021; 23(3): 763. CrossRef - Urinary DPP4 correlates with renal dysfunction, and DPP4 inhibition protects against the reduction in megalin and podocin expression in experimental CKD
Acaris Benetti, Flavia Letícia Martins, Letícia Barros Sene, Maria Heloisa M. Shimizu, Antonio C. Seguro, Weverton M. Luchi, Adriana C. C. Girardi
American Journal of Physiology-Renal Physiology.2021; 320(3): F285. CrossRef - Incretin-based drugs and the kidney in type 2 diabetes: choosing between DPP-4 inhibitors and GLP-1 receptor agonists
Johannes F.E. Mann, Marcel H.A. Muskiet
Kidney International.2021; 99(2): 314. CrossRef - Renoprotective Effects of DPP-4 Inhibitors
Daiji Kawanami, Yuichi Takashi, Hiroyuki Takahashi, Ryoko Motonaga, Makito Tanabe
Antioxidants.2021; 10(2): 246. CrossRef - Danegaptide Prevents TGFβ1-Induced Damage in Human Proximal Tubule Epithelial Cells of the Kidney
Paul E. Squires, Gareth W. Price, Ulrik Mouritzen, Joe A. Potter, Bethany M. Williams, Claire E. Hills
International Journal of Molecular Sciences.2021; 22(6): 2809. CrossRef - Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2021; 36(2): 388. CrossRef - Consensus Recommendations by the Asian Pacific Society of Cardiology: Optimising Cardiovascular Outcomes in Patients with Type 2 Diabetes
Jack Wei Chieh Tan, David Sim, Junya Ako, Wael Almahmeed, Mark E Cooper, Jamshed J Dalal, Chaicharn Deerochanawong, David Wei Chun Huang, Sofian Johar, Upendra Kaul, Sin Gon Kim, Natalie Koh, Alice Pik-Shan Kong, Rungroj Krittayaphong, Bernard Kwok, Bien
European Cardiology Review.2021;[Epub] CrossRef - Diabetes and kidney disease: emphasis on treatment with SGLT-2 inhibitors and GLP-1 receptor agonists
Francesco Prattichizzo, Paola de Candia, Antonio Ceriello
Metabolism.2021; 120: 154799. CrossRef - SGLT2 Inhibitors and Other Novel Therapeutics in the Management of Diabetic Kidney Disease
Robert C. Stanton
Seminars in Nephrology.2021; 41(2): 85. CrossRef - Mineralocorticoid Receptor Antagonists in Diabetic Kidney Disease
Nina Vodošek Hojs, Sebastjan Bevc, Robert Ekart, Nejc Piko, Tadej Petreski, Radovan Hojs
Pharmaceuticals.2021; 14(6): 561. CrossRef - Podocyte Glucocorticoid Receptors Are Essential for Glomerular Endothelial Cell Homeostasis in Diabetes Mellitus
Swayam Prakash Srivastava, Han Zhou, Ocean Setia, Alan Dardik, Carlos Fernandez‐Hernando, Julie Goodwin
Journal of the American Heart Association.2021;[Epub] CrossRef - Coronavirus Disease (COVID)-19 and Diabetic Kidney Disease
Swayam Prakash Srivastava, Rohit Srivastava, Subhash Chand, Julie E. Goodwin
Pharmaceuticals.2021; 14(8): 751. CrossRef - Effects of DPP4 inhibitors on renal outcomes in diabetes mellitus: A systematic review and meta-analysis
SaikatK Dalui, Raja Chakraverty, Nafisha Yasmin, Smita Pattanaik, Kaushik Pandit, Suparna Chatterjee
Indian Journal of Endocrinology and Metabolism.2021; 25(4): 283. CrossRef - Comparison of Adverse Kidney Outcomes With Empagliflozin and Linagliptin Use in Patients With Type 2 Diabetic Patients in a Real-World Setting
Yueh-Ting Lee, Chien-Ning Hsu, Chung-Ming Fu, Shih-Wei Wang, Chiang-Chi Huang, Lung-Chih Li
Frontiers in Pharmacology.2021;[Epub] CrossRef - The Role of DPP-4 Inhibitors in Type-2 Diabetes Patients with Chronic Kidney Disease
Mishal Yousef Alqurashi, Khalid Faisal Alharthi, Abdulaziz Abdulrahman Alshehri, Yazeed Khalid Alharbi, Mohammad Abdulmunem Sanousi, Anas Abdullah Almazyed, Khulud Saeed Alghamdi, Sarah Musaad Alrashidi, Waad Abdullah Qaeed, Amjad Aedh Alasmari
Pharmacophore.2021; 12(3): 91. CrossRef - Type 2 diabetes mellitus management in patients with chronic kidney disease: an update
Zoi Kleinaki, Stella Kapnisi, Sofia-Andriani Theodorelou-Charitou, Ilias P. Nikas, Stavroula A. Paschou
Hormones.2020; 19(4): 467. CrossRef - Renal Outcomes in Type 2 Diabetes: A Review of Cardiovascular and Renal Outcome Trials
David M. Williams, Asif Nawaz, Marc Evans
Diabetes Therapy.2020; 11(2): 369. CrossRef - Favorable pleiotropic effects of sodium glucose cotransporter 2 inhibitors: head-to-head comparisons with dipeptidyl peptidase-4 inhibitors in type 2 diabetes patients
Shih-Chieh Shao, Kai-Cheng Chang, Swu-Jane Lin, Rong-Nan Chien, Ming-Jui Hung, Yuk-Ying Chan, Yea-Huei Kao Yang, Edward Chia-Cheng Lai
Cardiovascular Diabetology.2020;[Epub] CrossRef - Novel therapeutic agents for the treatment of diabetic kidney disease
Rachel E. Hartman, P.S.S. Rao, Mariann D. Churchwell, Susan J. Lewis
Expert Opinion on Investigational Drugs.2020; 29(11): 1277. CrossRef - Renal protection with glucagon-like peptide-1 receptor agonists
Martina Vitale, Jonida Haxhi, Tiziana Cirrito, Giuseppe Pugliese
Current Opinion in Pharmacology.2020; 54: 91. CrossRef - Loss of Mitochondrial Control Impacts Renal Health
Swayam Prakash Srivastava, Keizo Kanasaki, Julie E. Goodwin
Frontiers in Pharmacology.2020;[Epub] CrossRef - Effects of Sodium-Glucose Cotransporter 2 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Scientific Reports.2019;[Epub] CrossRef
- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study

- Diabetes
- Evolution of Diabetes Care in Hong Kong: From the Hong Kong Diabetes Register to JADE-PEARL Program to RAMP and PEP Program
- Ivy H.Y. Ng, Kitty K.T. Cheung, Tiffany T.L. Yau, Elaine Chow, Risa Ozaki, Juliana C.N. Chan
- Endocrinol Metab. 2018;33(1):17-32. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.17
- 5,109 View
- 68 Download
- 16 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub The rapid increase in diabetes prevalence globally has contributed to large increases in health care expenditure on diabetic complications, posing a major health burden to countries worldwide. Asians are commonly observed to have poorer β-cell function and greater insulin resistance compared to the Caucasian population, which is attributed by their lower lean body mass and central obesity. This “double phenotype” as well as the rising prevalence of young onset diabetes in Asia has placed Asians with diabetes at high risk of cardiovascular and renal complications, with cancer emerging as an important cause of morbidity and mortality. The experience from Hong Kong had demonstrated that a multifaceted approach, involving team-based integrated care, information technological advances, and patient empowerment programs were able to reduce the incidence of diabetic complications, hospitalizations, and mortality. System change and public policies to enhance implementation of such programs may provide solutions to combat the burgeoning health problem of diabetes at a societal level.
-
Citations
Citations to this article as recorded by- Impact of Body Composition and Anemia on Accuracy of a Real-Time Continuous Glucose Monitor in Diabetes Patients on Continuous Ambulatory Peritoneal Dialysis
James Ling, Jack K.C. Ng, Eric S.H. Lau, Andrea O.Y. Luk, Ronald C.W. Ma, Robert A. Vigersky, Philip K.T. Li, Juliana C.N. Chan, Cheuk Chun Szeto, Elaine Chow
Diabetes Technology & Therapeutics.2024; 26(1): 70. CrossRef - Levels and correlates of risk factor control in diabetes mellitus –ELSA-Brasil
Bruna Cristine Chwal, Rodrigo Citton Padilha dos Reis, Maria Inês Schmidt, Bruce B. Duncan, Sandhi Maria Barreto, Rosane Harter Griep
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Trends in risk factor control and treatment among patients with non‐alcoholic fatty liver disease and type 2 diabetes between 2000 and 2020: A territory‐wide study
Xinrong Zhang, Terry Cheuk‐Fung Yip, Yee‐Kit Tse, Vicki Wing‐Ki Hui, Guanlin Li, Huapeng Lin, Lilian Yan Liang, Jimmy Che‐To Lai, Mandy Sze‐Man Lai, Johnny T. K. Cheung, Henry Lik‐Yuen Chan, Stephen Lam Chan, Alice Pik‐Shan Kong, Grace Lai‐Hung Wong, Vinc
Alimentary Pharmacology & Therapeutics.2023; 57(10): 1103. CrossRef - Team-Based Diabetes Care in Ontario and Hong Kong: a Comparative Review
Calvin Ke, Emaad Mohammad, Juliana C. N. Chan, Alice P. S. Kong, Fok-Han Leung, Baiju R. Shah, Douglas Lee, Andrea O. Luk, Ronald C. W. Ma, Elaine Chow, Xiaolin Wei
Current Diabetes Reports.2023; 23(7): 135. CrossRef - Team-Based Approach to Reduce Malignancies in People with Diabetes and Obesity
Ziyue Zhu, Samuel Yeung Shan Wong, Joseph Jao Yiu Sung, Thomas Yuen Tung Lam
Current Diabetes Reports.2023; 23(10): 253. CrossRef - Professor Juliana Chung Ngor Chan: Tireless Trailblazer for Diabetes Research, Care, and Education in Asia
Ronald C.W. Ma, Wing Yee So, Andrea O.Y. Luk
Diabetes Care.2022; 45(10): 2207. CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - From Hong Kong Diabetes Register to JADE Program to RAMP-DM for Data-Driven Actions
Juliana C.N. Chan, Lee-Ling Lim, Andrea O.Y. Luk, Risa Ozaki, Alice P.S. Kong, Ronald C.W. Ma, Wing-Yee So, Su-Vui Lo
Diabetes Care.2019; 42(11): 2022. CrossRef - Cholesterol levels and development of cardiovascular disease in Koreans with type 2 diabetes mellitus and without pre-existing cardiovascular disease
Mee Kyoung Kim, Kyungdo Han, Han Na Joung, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Effects of Variability in Blood Pressure, Glucose, and Cholesterol Concentrations, and Body Mass Index on End-Stage Renal Disease in the General Population of Korea
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Journal of Clinical Medicine.2019; 8(5): 755. CrossRef - Efficacy and safety of fixed‐dose combination therapy with gemigliptin (50 mg) and rosuvastatin compared with monotherapy in patients with type 2 diabetes and dyslipidaemia (BALANCE): A multicentre, randomized, double‐blind, controlled, phase 3 trial
Ji Cheol Bae, Kyung Wan Min, Yong Hyun Kim, Kyoung‐Ah Kim, Eun‐Gyoung Hong, Cheol‐Young Park, Song Han, Bong‐Soo Cha
Diabetes, Obesity and Metabolism.2019; 21(1): 103. CrossRef - Statin Use is Associated with Decreased Hepatocellular Carcinoma Recurrence in Liver Transplant Patients
Yongin Cho, Myoung Soo Kim, Chung Mo Nam, Eun Seok Kang
Scientific Reports.2019;[Epub] CrossRef
- Impact of Body Composition and Anemia on Accuracy of a Real-Time Continuous Glucose Monitor in Diabetes Patients on Continuous Ambulatory Peritoneal Dialysis

- Clinical Study
- Factors Associated with Postoperative Diabetes Insipidus after Pituitary Surgery
- Antonio L. Faltado, Anna Angelica Macalalad-Josue, Ralph Jason S. Li, John Paul M. Quisumbing, Marc Gregory Y. Yu, Cecilia A. Jimeno
- Endocrinol Metab. 2017;32(4):426-433. Published online November 21, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.4.426
- 5,526 View
- 92 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Determining risk factors for diabetes insipidus (DI) after pituitary surgery is important in improving patient care. Our objective is to determine the factors associated with DI after pituitary surgery.
Methods We reviewed records of patients who underwent pituitary surgery from 2011 to 2015 at Philippine General Hospital. Patients with preoperative DI were excluded. Multiple logistic regression analysis was performed and a predictive model was generated. The discrimination abilities of the predictive model and individual variables were assessed using the receiving operator characteristic curve.
Results A total of 230 patients were included. The rate of postoperative DI was 27.8%. Percent change in serum Na (odds ratio [OR], 1.39; 95% confidence interval [CI], 1.15 to 1.69); preoperative serum Na (OR, 1.19; 95% CI, 1.02 to 1.40); and performance of craniotomy (OR, 5.48; 95% CI, 1.60 to 18.80) remained significantly associated with an increased incidence of postoperative DI, while percent change in urine specific gravity (USG) (OR, 0.53; 95% CI, 0.33 to 0.87) and meningioma on histopathology (OR, 0.05; 95% CI, 0.04 to 0.70) were significantly associated with a decreased incidence. The predictive model generated has good diagnostic accuracy in predicting postoperative DI with an area under curve of 0.83.
Conclusion Greater percent change in serum Na, preoperative serum Na, and performance of craniotomy significantly increased the likelihood of postoperative DI while percent change in USG and meningioma on histopathology were significantly associated with a decreased incidence. The predictive model can be used to generate a scoring system in estimating the risk of postoperative DI.
-
Citations
Citations to this article as recorded by- Importance of Intraoperative Factors in Postoperative Arginine Vasopressin Deficiency After Pituitary Adenoma Surgery
Nasim Alidaei, Guive Sharifi, Zahra Davoudi
Endocrine Practice.2024; 30(3): 253. CrossRef - Incidence of post-operative diabetes insipidus and associated factors after pituitary surgery in two teaching hospitals, in Addis Ababa, Ethiopia: A prospective observational study
Abera Chanie, Abat Sahlu
Interdisciplinary Neurosurgery.2024; 37: 101978. CrossRef - Pituitary Adenoma in the Philippines: A Scoping Review on the Treatment Gaps, Challenges, and Current State of Care
Mykha Marie B. Tabuzo, Mary Angeline Luz U. Hernandez, Annabell E. Chua, Patricia D. Maningat, Harold Henrison C. Chiu, Roland Dominic G. Jamora
Medical Sciences.2024; 12(1): 16. CrossRef - Correlation of Pituitary Descent and Diabetes Insipidus After Transsphenoidal Pituitary Macroadenoma Resection
Josh Ma, Peter Gooderham, Ryojo Akagami, Serge Makarenko
Neurosurgery.2023; 92(6): 1269. CrossRef - Risk Factors Related to Transient Diabetes Insipidus Development Following Transsphenoidal Pituitary Adenoma Resection: A Multicentric Study
Marcos Ezequiel Yasuda, Daniela Renedo, Soledad Sosa, Karina Danilowicz, Rodolfo Recalde, Roberto Zaninovich, Santiago Gonzalez Abbati, Andrés Cervio, Sebastian Giovannini, Juan Villalonga, Liezel Ulloque-Caamaño, Kesava Reddy, Mariano Socolovsky, Alvaro
World Neurosurgery.2023; 175: e636. CrossRef - Change in cephalocaudal tumor cavity diameter after transsphenoidal surgery is a predictor of diabetes insipidus in pituitary adenoma
Kunzhe Lin, Kaichun Fan, Shuwen Mu, Shousen Wang
European Journal of Medical Research.2022;[Epub] CrossRef - Change in the pituitary stalk deviation angle after transsphenoidal surgery can predict the development of diabetes insipidus for pituitary adenomas
Liang Xue, Jianwu Wu, Jie Chen, Yongkai Yang
Endocrine Connections.2022;[Epub] CrossRef - Disorders of Salt and Water Balance After Pituitary Surgery
Emily K Brooks, Warrick J Inder
The Journal of Clinical Endocrinology & Metabolism.2022; 108(1): 198. CrossRef - Postoperative diabetes insipidus: how to define and grade this complication?
Friso de Vries, Daniel J. Lobatto, Marco J. T. Verstegen, Wouter R. van Furth, Alberto M. Pereira, Nienke R. Biermasz
Pituitary.2021; 24(2): 284. CrossRef - Diaphragma sellae sinking can predict the onset of hyponatremia after transsphenoidal surgery for pituitary adenomas
Kunzhe Lin, Jun Li, Lingling Lu, Shangming Zhang, Shuwen Mu, Zhijie Pei, Cheng Wang, Jingying Lin, Liang Xue, Liangfeng Wei, Lin Zhao, Shousen Wang
Journal of Endocrinological Investigation.2021; 44(11): 2511. CrossRef - Adrenocorticotropic hormone-secreting pituitary macroadenoma: A pictorial case report and review
Ujjwala Murkute
Indian Journal of Continuing Nursing Education.2021; 22(2): 137. CrossRef - Sodium Perturbations After Pituitary Surgery
Kevin C.J. Yuen, Adnan Ajmal, Ricardo Correa, Andrew S. Little
Neurosurgery Clinics of North America.2019; 30(4): 515. CrossRef
- Importance of Intraoperative Factors in Postoperative Arginine Vasopressin Deficiency After Pituitary Adenoma Surgery

- Effects of Incretin-Based Therapies on Diabetic Microvascular Complications
- Yu Mi Kang, Chang Hee Jung
- Endocrinol Metab. 2017;32(3):316-325. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.316
- 4,612 View
- 55 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The morbidity and mortality associated with diabetic complications impose a huge socioeconomic burden worldwide. Therefore, the ultimate goal of managing diabetes mellitus (DM) is to lower the risk of macrovascular complications and highly morbid microvascular complications such as diabetic nephropathy (DN) and diabetic retinopathy (DR). Potential benefits of incretin-based therapies such as glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and dipeptidyl peptidase-4 (DPP-4) inhibitors on the diabetic macrovascular complications have been recently suggested, owing to their pleiotropic effects on multiple organ systems. However, studies primarily investigating the role of these therapies in diabetic microvascular complications are rare. Nevertheless, preclinical and limited clinical data suggest the potential protective effect of incretin-based agents against DN and DR via their anti-inflammatory, antioxidative, and antiapoptotic properties. Evidence also suggests that these incretin-dependent and independent beneficial effects are not necessarily associated with the glucose-lowering properties of GLP-1 RAs and DPP-4 inhibitors. Hence, in this review, we revisit the preclinical and clinical evidence of incretin-based therapy for DR and DN, the two most common, morbid complications in individuals with DM. In addition, the review discusses a few recent studies raising concerns of aggravating DR with the use of incretin-based therapies.
-
Citations
Citations to this article as recorded by- Efficacy and Safety of the Utilization of Dipeptidyl Peptidase IV Inhibitors in Diabetic Patients with Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical Trials
Moeber Mahzari, Muhannad Alqirnas, Moustafa Alhamadh, Faisal Alrasheed, Abdulrahman Alhabeeb, Wedad Al Madani, Hussain Aldera
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1425. CrossRef - Anti-Inflammatory Effects of GLP-1R Activation in the Retina
Alessandra Puddu, Davide Maggi
International Journal of Molecular Sciences.2022; 23(20): 12428. CrossRef - Diabetes and Its Complications: Therapies Available, Anticipated and Aspired
Anu Grover, Komal Sharma, Suresh Gautam, Srishti Gautam, Monica Gulati, Sachin Kumar Singh
Current Diabetes Reviews.2021; 17(4): 397. CrossRef - SGLT2 Inhibitors, GLP-1 Agonists, and DPP-4 Inhibitors in Diabetes and Microvascular Complications: A Review
Christopher El Mouhayyar, Ruba Riachy, Abir Bou Khalil, Asaad Eid, Sami Azar
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Novel therapeutic agents for the treatment of diabetic kidney disease
Rachel E. Hartman, P.S.S. Rao, Mariann D. Churchwell, Susan J. Lewis
Expert Opinion on Investigational Drugs.2020; 29(11): 1277. CrossRef - Nationwide Trends in Pancreatitis and Pancreatic Cancer Risk Among Patients With Newly Diagnosed Type 2 Diabetes Receiving Dipeptidyl Peptidase 4 Inhibitors
Minyoung Lee, Jiyu Sun, Minkyung Han, Yongin Cho, Ji-Yeon Lee, Chung Mo Nam, Eun Seok Kang
Diabetes Care.2019; 42(11): 2057. CrossRef - Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2019; 34(1): 80. CrossRef - Serum adipocytokines are associated with microalbuminuria in patients with type 1 diabetes and incipient chronic complications
Tomislav Bulum, Marijana Vučić Lovrenčić, Martina Tomić, Sandra Vučković-Rebrina, Vinko Roso, Branko Kolarić, Vladimir Vuksan, Lea Duvnjak
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 496. CrossRef - Protective Effects of Incretin Against Age-Related Diseases
Di Zhang, Mingzhu Ma, Yueze Liu
Current Drug Delivery.2019; 16(9): 793. CrossRef - The role of dipeptidylpeptidase-4 inhibitors in management of cardiovascular disease in diabetes; focus on linagliptin
Annayya R. Aroor, Camila Manrique-Acevedo, Vincent G. DeMarco
Cardiovascular Diabetology.2018;[Epub] CrossRef
- Efficacy and Safety of the Utilization of Dipeptidyl Peptidase IV Inhibitors in Diabetic Patients with Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical Trials

- Vascular Cell Adhesion Molecule 1, Intercellular Adhesion Molecule 1, and Cluster of Differentiation 146 Levels in Patients with Type 2 Diabetes with Complications
- F. Sinem Hocaoglu-Emre, Devrim Saribal, Guven Yenmis, Guvenc Guvenen
- Endocrinol Metab. 2017;32(1):99-105. Published online March 20, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.99
- 3,954 View
- 74 Download
- 19 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Type 2 diabetes mellitus (T2DM) is a multisystemic, chronic disease accompanied by microvascular complications involving various complicated mechanisms. Intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), and cluster of differentiation-146 (CD146) are mainly expressed by endothelial cells, and facilitate the adhesion and transmigration of immune cells, leading to inflammation. In the present study, we evaluated the levels of soluble adhesion molecules in patients with microvascular complications of T2DM.
Methods Serum and whole blood samples were collected from 58 T2DM patients with microvascular complications and 20 age-matched healthy subjects. Levels of soluble ICAM-1 (sICAM-1) and soluble VCAM-1 (sVCAM-1) were assessed using enzyme-linked immunosorbent assay, while flow cytometry was used to determine CD146 levels.
Results Serum sICAM-1 levels were lower in T2DM patients with microvascular complications than in healthy controls (
P <0.05). No significant differences were found in sVCAM-1 and CD146 levels between the study and the control group. Although patients were subdivided into groups according to the type of microvascular complications that they experienced, cell adhesion molecule levels were not correlated with the complication type.Conclusion In the study group, most of the patients were on insulin therapy (76%), and 95% of them were receiving angiotensin-converting enzyme (ACE)-inhibitor agents. Insulin and ACE-inhibitors have been shown to decrease soluble adhesion molecule levels via various mechanisms, so we suggest that the decreased or unchanged levels of soluble forms of cellular adhesion molecules in our study group may have resulted from insulin and ACE-inhibitor therapy, as well as tissue-localized inflammation in patients with T2DM.
-
Citations
Citations to this article as recorded by- Immunity status and expression of molecular markers (ICAM-1, CD5, CD25, CD95) on lymphocytes of patients with recurrent anterior uveitis complicated by macular edema
Natalia I. Khramenko, Natalia V. Konovalova, Volodymyr Ya. Usov, Liudmyla M. Velychko, Olexandra V. Bogdanova
Graefe's Archive for Clinical and Experimental Ophthalmology.2023; 261(5): 1423. CrossRef - The association of cell adhesion molecules and selectins (VCAM-1, ICAM-1, E-selectin, L-selectin, and P-selectin) with microvascular complications in patients with type 2 diabetes: A follow-up study
Khalid Siddiqui, Teena P. George, Muhammad Mujammami, Arthur Isnani, Assim A. Alfadda
Frontiers in Endocrinology.2023;[Epub] CrossRef - Vascular cell adhesion molecule‑1 levels in patients with coronary artery disease with type 2 diabetes mellitus
S.A. Serik, N.R. Mavrycheva
Medicni perspektivi.2023; 28(1): 82. CrossRef - Diabetic Endothelial Cell Glycogen Synthase Kinase 3β Activation Induces VCAM1 Ectodomain Shedding
Masuma Akter Brishti, Somasundaram Raghavan, Kennedy Lamar, Udai P. Singh, Daniel M. Collier, M. Dennis Leo
International Journal of Molecular Sciences.2023; 24(18): 14105. CrossRef - Evaluation of cell adhesion molecules (LFA-1 and L-selectin) in ankylosing spondylitis patients after treatment with β-D-mannuronic acid (M2000)
MohammadJavad Fattahi, BerndH A. Rehm, Hidenori Matsuo, Salvatore Cuzzocrea, Fahimeh Jafarnezhad-Ansariha, Hossein Ahmadi, Farzaneh Tofighi-Zavareh, Mona Oraei, Zahra Aghazadeh, Abbas Mirshafiey
Indian Journal of Medical Research.2023; 157(5): 453. CrossRef - Coenzyme Q10 administration has no effect on sICAM-1 and metabolic parameters of pediatrics with type 1 diabetes mellitus
Heba Serag, Lamia El Wakeel, Amira Adly
International Journal for Vitamin and Nutrition Research.2021; 91(3-4): 315. CrossRef - Diabetes induced renal complications by leukocyte activation of nuclear factor κ-B and its regulated genes expression
Noura M. Darwish, Yousif M. Elnahas, Fatmah S. AlQahtany
Saudi Journal of Biological Sciences.2021; 28(1): 541. CrossRef - Effect of French maritime pine bark extract supplementation on metabolic status and serum vascular cell adhesion molecule-1 levels in patients with type 2 diabetes and microalbuminuria
Elham Navval-Esfahlan, Maryam Rafraf, Somayyeh Asghari, Hossein Imani, Mohammad Asghari-Jafarabadi, Sanaz Karimi-Avval
Complementary Therapies in Medicine.2021; 58: 102689. CrossRef - Dysregulation of Leukocyte Trafficking in Type 2 Diabetes: Mechanisms and Potential Therapeutic Avenues
Laleh Pezhman, Abd Tahrani, Myriam Chimen
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Regulatory effects of IL-1β in the interaction of GBM and tumor-associated monocyte through VCAM-1 and ICAM-1
Ching-Kai Shen, Bor-Ren Huang, Wei-Lan Yeh, Chao-Wei Chen, Yu-Shu Liu, Sheng-Wei Lai, Wen-Pei Tseng, Dah-Yuu Lu, Cheng-Fang Tsai
European Journal of Pharmacology.2021; 905: 174216. CrossRef - Serum netrin and VCAM-1 as biomarker for Egyptian patients with type IΙ diabetes mellitus
Maher M. Fadel, Faten R. Abdel Ghaffar, Shimaa K. Zwain, Hany M. Ibrahim, Eman AE. badr
Biochemistry and Biophysics Reports.2021; 27: 101045. CrossRef - Circulating Biomarkers of Inflammation and Endothelial Activation in Diabetic Retinopathy
Federica Storti, Jennifer Pulley, Pascal Kuner, Markus Abt, Ulrich F. O. Luhmann
Translational Vision Science & Technology.2021; 10(12): 8. CrossRef - Estimation of Vascular Cell Adhesion Molecule 1 (VCAM-1) Levels In Type 1 Diabetic Mellitus Patients
Ousamha Akram Saterr, Abeer J. Hassan, Qahtan Adnan Rasheed
Bionatura.2021; 6(4): 2292. CrossRef - IL-18, VCAM-1 and P-selectin as early biomarkers in normoalbuminuric Type 2 diabetes patients
Khalid Al-Rubeaan, Shaik S Nawaz, Amira M Youssef, Mohammed Al Ghonaim, Khalid Siddiqui
Biomarkers in Medicine.2019; 13(6): 467. CrossRef - miR-146a mediates thymosin β4 induced neurovascular remodeling of diabetic peripheral neuropathy in type-II diabetic mice
Lei Wang, Michael Chopp, XueRong Lu, Alexandra Szalad, LongFei Jia, Xian Shuang Liu, Kuan-Han Wu, Mei Lu, Zheng Gang Zhang
Brain Research.2019; 1707: 198. CrossRef
- Immunity status and expression of molecular markers (ICAM-1, CD5, CD25, CD95) on lymphocytes of patients with recurrent anterior uveitis complicated by macular edema

- Clinical Study
- Comparison of Age of Onset and Frequency of Diabetic Complications in the Very Elderly Patients with Type 2 Diabetes
- Bong-Ki Lee, Sang-Wook Kim, Daehee Choi, Eun-Hee Cho
- Endocrinol Metab. 2016;31(3):416-423. Published online August 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.416
- 3,298 View
- 44 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The prevalence of type 2 diabetes in elderly people has increased dramatically in the last few decades. This study was designed to clarify the clinical characteristics of type 2 diabetes in patients aged ≥80 years according to age of onset.
Methods We reviewed the medical records of 289 patients aged ≥80 years with type 2 diabetes at the outpatient diabetes clinics of Kangwon National University Hospital from September 2010 to June 2014. We divided the patients into middle-age-onset diabetes (onset before 65 years of age) and elderly-onset diabetes (onset at 65+ years of age).
Results There were 141 male and 148 female patients. The patients had a mean age of 83.2±2.9 years and the mean duration of diabetes was 14.3±10.4 years. One hundred and ninety-nine patients had elderly-onset diabetes. The patients with elderly-onset diabetes had a significantly lower frequency of diabetic retinopathy and nephropathy, lower serum creatinine levels, lower glycated hemoglobin (HbA1c) levels, and similar coronary revascularization and cerebral infarction rates compared to those with middle-age-onset diabetes. There was no frequency difference in coronary revascularization and cerebral infarction and HbA1c levels between three subgroups (<5, 5 to 15, and ≥15 years) of diabetes duration in elderly onset diabetes. However, both in the elderly onset diabetes and middle-age-onset diabetes, the cumulative incidence of retinopathy was increasing rapidly according to the duration of diabetes.
Conclusion We report that individuals with elderly-onset diabetes have a lower frequency of diabetic retinopathy and nephropathy and similar cardiovascular complications compared to those with middle-age-onset diabetes.
-
Citations
Citations to this article as recorded by- Rescue of High Glucose Impairment of Cultured Human Osteoblasts Using Cinacalcet and Parathyroid Hormone
V. A. Shahen, A. Schindeler, M. S. Rybchyn, C. M. Girgis, B. Mulholland, R. S. Mason, I. Levinger, T. C. Brennan-Speranza
Calcified Tissue International.2023; 112(4): 452. CrossRef - Factors Related to the Occurrence and Number of Chronic Diabetic Complications in Patients with Type 2 Diabetes Mellitus: Utilizing The National Health Insurance Service-National Health Screening Cohort in Korea, 2002~2015
Haejung Lee, Misoon Lee, Gaeun Park, Ah Reum Khang
Journal of Korean Gerontological Nursing.2022; 24(1): 22. CrossRef - Prevalence of and Risk Factors for Diabetic Retinopathy and Diabetic Macular Edema in Patients with Early- and Late-Onset Diabetes Mellitus
Yu Wang, Zhong Lin, Gang Zhai, Xiao Xia Ding, Liang Wen, Dong Li, Bo Zou, Ke Mi Feng, Yuan Bo Liang, Cong Xie
Ophthalmic Research.2022; 65(3): 293. CrossRef - Associations of Age at Diagnosis and Duration of Diabetes With Morbidity and Mortality Among Older Adults
Christine T. Cigolle, Caroline S. Blaum, Chen Lyu, Jinkyung Ha, Mohammed Kabeto, Judy Zhong
JAMA Network Open.2022; 5(9): e2232766. CrossRef - Chart review of diagnostic methods, baseline characteristics and symptoms for European patients with pancreatic cancer
Alfredo Carrato, Davide Melisi, Gerald Prager, Christoph B Westphalen, Anabel Ferreras, Nathalie D’Esquermes, Julien Taieb, Teresa M Mercadé
Future Oncology.2021; 17(15): 1843. CrossRef - Distinction of cardiometabolic profiles among people ≥75 years with type 2 diabetes: a latent profile analysis
Antoine CHRISTIAENS, Michel P. HERMANS, Benoit BOLAND, Séverine HENRARD
BMC Endocrine Disorders.2019;[Epub] CrossRef - Validity of diagnostic codes and estimation of prevalence of diabetic foot ulcers using a large electronic medical record database
Avivit Cahn, Talya Altaras, Tal Agami, Ori Liran, Colette E. Touaty, Michel Drahy, Rena Pollack, Itamar Raz, Gabriel Chodick, Inbar Zucker
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Response: Comparison of Age of Onset and Frequency of Diabetic Complications in the Very Elderly Patients with Type 2 Diabetes (Endocrinol Metab2016;31:416-23, Bong-Ki Lee et al.)
Eun-Hee Cho
Endocrinology and Metabolism.2017; 32(1): 142. CrossRef - Letter: Comparison of Age of Onset and Frequency of Diabetic Complications in the Very Elderly Patients with Type 2 Diabetes (Endocrinol Metab2016;31:416-23, Bong-Ki Lee et al.)
Mee Kyoung Kim
Endocrinology and Metabolism.2017; 32(1): 140. CrossRef
- Rescue of High Glucose Impairment of Cultured Human Osteoblasts Using Cinacalcet and Parathyroid Hormone

- Obesity and Metabolism
- Clinical Implications of Glucose Variability: Chronic Complications of Diabetes
- Hye Seung Jung
- Endocrinol Metab. 2015;30(2):167-174. Published online June 30, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.2.167
- 5,816 View
- 96 Download
- 66 Web of Science
- 69 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucose variability has been identified as a potential risk factor for diabetic complications; oxidative stress is widely regarded as the mechanism by which glycemic variability induces diabetic complications. However, there remains no generally accepted gold standard for assessing glucose variability. Representative indices for measuring intraday variability include calculation of the standard deviation along with the mean amplitude of glycemic excursions (MAGE). MAGE is used to measure major intraday excursions and is easily measured using continuous glucose monitoring systems. Despite a lack of randomized controlled trials, recent clinical data suggest that long-term glycemic variability, as determined by variability in hemoglobin A1c, may contribute to the development of microvascular complications. Intraday glycemic variability is also suggested to accelerate coronary artery disease in high-risk patients.
-
Citations
Citations to this article as recorded by- Glycemic variability is associated with sural nerve conduction velocity in outpatients with type 2 diabetes: Usefulness of a new point‐of‐care device for nerve conduction studies
Machiko Morita, Kentaro Sada, Shuji Hidaka, Miki Ogawa, Hirotaka Shibata
Journal of Diabetes Investigation.2024;[Epub] CrossRef - A randomized trial on the effect of transcutaneous electrical nerve stimulator on glycemic control in patients with type 2 diabetes
Jin-Ying Lu, Horng-Yih Ou, Chung-Ze Wu, Chwen-Yi Yang, Ju-Ying Jiang, Chieh-Hsiang Lu, Yi-Der Jiang, Tien-Jyun Chang, Yi-Cheng Chang, Meng-Lun Hsieh, Wan-Chen Wu, Hung-Yuan Li, Ye-Fong Du, Ching-Han Lin, Hao-Chang Hung, Kai-Jen Tien, Nai-Cheng Yeh, Shang-
Scientific Reports.2023;[Epub] CrossRef - Association between initial in-hospital heart rate and glycemic control in patients with acute ischemic stroke and diabetes mellitus
Ya-Wen Kuo, Jiann-Der Lee, Chuan-Pin Lee, Yen-Chu Huang, Meng Lee
BMC Endocrine Disorders.2023;[Epub] CrossRef - Practical Application of Continuous Glucose Monitoring in Clinical Practice: Case Studies
Jeff Unger, Denise R. Franco
Diabetes Technology & Therapeutics.2023; 25(S3): S-21. CrossRef - Comparison of Glycemia Risk Index with Time in Range for Assessing Glycemic Quality
Ji Yoon Kim, Jee Hee Yoo, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2023; 25(12): 883. CrossRef - Personalized diabetes monitoring platform leveraging IoMT and AI for non-invasive estimation
Durga Padmavilochanan, Rahul Krishnan Pathinarupothi, K.A. Unnikrishna Menon, Harish Kumar, Ramesh Guntha, Maneesha V. Ramesh, P. Venkat Rangan
Smart Health.2023; 30: 100428. CrossRef - Acute effects of drinks containing blackcurrant and citrus (poly)phenols and dietary fibre on postprandial glycaemia, gut hormones, cognitive function and appetite in healthy adults: two randomised controlled trials
Ana M. Pinto, Mark R. Hobden, Katherine D. Brown, Jonathan Farrimond, Darren Targett, Christopher P. Corpe, Peter R. Ellis, Yvanna Todorova, Klaudia Socha, Shatha Bahsoon, Claudia Haworth, Morgane Marcel, Xirui Nie, Wendy L. Hall
Food & Function.2023; 14(22): 10163. CrossRef - Metabolomics in diabetes mellitus: clinical insight
Shereen M. Aleidi, Hiba Al Fahmawi, Afshan Masood, Anas Abdel Rahman
Expert Review of Proteomics.2023; 20(12): 451. CrossRef - Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
Diabetes & Metabolism Journal.2022; 46(1): 81. CrossRef - Glycemic Variability and Diabetes Mellitus
Han Na Jang, Hye Seung Jung
The Journal of Korean Diabetes.2022; 23(1): 12. CrossRef - Comparison of the Impact of Insulin Degludec U100 and Insulin Glargine U300 on Glycemic Variability and Oxidative Stress in Insulin-Naive Patients With Type 2 Diabetes Mellitus: Pilot Study for a Randomized Trial
Pavle Vrebalov Cindro, Mladen Krnić, Darko Modun, Jonatan Vuković, Tina Tičinović Kurir, Goran Kardum, Doris Rušić, Ana Šešelja Perišin, Josipa Bukić
JMIR Formative Research.2022; 6(7): e35655. CrossRef - Endothelial Dysfunction and Platelet Hyperactivation in Diabetic
Complications Induced by Glycemic Variability
Ye Huang, Long Yue, Jiahuang Qiu, Ming Gao, Sijin Liu, Jingshang Wang
Hormone and Metabolic Research.2022; 54(07): 419. CrossRef - Therapeutic potential of paeoniflorin in atherosclerosis: A cellular action and mechanism-based perspective
Wei Yu, Iqra Ilyas, Xuerui Hu, Suowen Xu, Hui Yu
Frontiers in Immunology.2022;[Epub] CrossRef - Effect of Dapagliflozin as an Add-on Therapy to Insulin on the Glycemic Variability in Subjects with Type 2 Diabetes Mellitus (DIVE): A Multicenter, Placebo-Controlled, Double-Blind, Randomized Study
Seung-Hwan Lee, Kyung-Wan Min, Byung-Wan Lee, In-Kyung Jeong, Soon-Jib Yoo, Hyuk-Sang Kwon, Yoon-Hee Choi, Kun-Ho Yoon
Diabetes & Metabolism Journal.2021; 45(3): 339. CrossRef - Association of time in range, as assessed by continuous glucose monitoring, with painful diabetic polyneuropathy
Junpeng Yang, Xueli Yang, Dongni Zhao, Xiaobing Wang, Wei Wei, Huijuan Yuan
Journal of Diabetes Investigation.2021; 12(5): 828. CrossRef - The Association Between Continuous Glucose Monitoring-Derived Metrics and Cardiovascular Autonomic Neuropathy in Outpatients with Type 2 Diabetes
Min Young Kim, Gyuri Kim, Ji Yun Park, Min Sun Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2021; 23(6): 434. CrossRef - Current concepts and clinical importance of glycemic variability
Ramya Ravi, V Balasubramaniam, Gowthamarajan Kuppusamy, Sivasankaran Ponnusankar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(2): 627. CrossRef - Glycemic deviation index: a novel method of integrating glycemic numerical value and variability
Yizhou Zou, Wanli Wang, Dongmei Zheng, Xu Hou
BMC Endocrine Disorders.2021;[Epub] CrossRef - Relationship between short and long-term glycemic variability and oxidative stress in type 1 diabetes mellitus under daily life insulin treatment
Tatiana Valente, Fernando Valente, Maria Beatriz Bastos Lucchesi, Giovana Rita Punaro, Margaret Gori Mouro, Monica Andrade Lima Gabbay, Elisa Mieko Suemitsu Higa, Sergio Atala Dib
Archives of Endocrinology and Metabolism.2021;[Epub] CrossRef - Evidence of Early Diabetic Nephropathy in Pediatric Type 1 Diabetes
Leena Mamilly, Lucy D. Mastrandrea, Claudia Mosquera Vasquez, Brett Klamer, Mahmoud Kallash, Ahmad Aldughiem
Frontiers in Endocrinology.2021;[Epub] CrossRef - Glucose Variability and Risk of Hepatocellular Carcinoma in Patients with Diabetes: A Nationwide Population-Based Study
Jeong-Ju Yoo, Eun Ju Cho, Kyungdo Han, Soo Seong Heo, Bo-Yeon Kim, Dong Wook Shin, Su Jong Yu
Cancer Epidemiology, Biomarkers & Prevention.2021; 30(5): 974. CrossRef - Effect of glucose concentration and culture substrate on HUVECs viability in in vitro cultures: A literature review and own results
Anna Ciechanowska, Ilona Gora, Stanislawa Sabalinska, Piotr Foltynski, Piotr Ladyzynski
Biocybernetics and Biomedical Engineering.2021; 41(4): 1390. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(3): 368. CrossRef - Immunosuppressive PLGA TGF-β1 Microparticles Induce Polyclonal and Antigen-Specific Regulatory T Cells for Local Immunomodulation of Allogeneic Islet Transplants
Ying Li, Anthony W. Frei, Irayme M. Labrada, Yanan Rong, Jia-Pu Liang, Magdalena M. Samojlik, Chuqiao Sun, Steven Barash, Benjamin G. Keselowsky, Allison L. Bayer, Cherie L. Stabler
Frontiers in Immunology.2021;[Epub] CrossRef - Retrospective study of glycemic variability, BMI, and blood pressure in diabetes patients in the Digital Twin Precision Treatment Program
Paramesh Shamanna, Mala Dharmalingam, Rakesh Sahay, Jahangir Mohammed, Maluk Mohamed, Terrence Poon, Nathan Kleinman, Mohamed Thajudeen
Scientific Reports.2021;[Epub] CrossRef - Dulaglutide improves muscle function by attenuating inflammation through OPA-1-TLR-9 signaling in aged mice
Phyu Phyu Khin, Yeonhee Hong, MyeongHoon Yeon, Dae Ho Lee, Jong Han Lee, Hee-Sook Jun
Aging.2021; 13(18): 21962. CrossRef - Glycemic Variability, Oxidative Stress, and Impact on Complications Related to Type 2 Diabetes Mellitus
Tatiana Valente, Alberto K. Arbex
Current Diabetes Reviews.2021;[Epub] CrossRef - The impact of structured self-monitoring of blood glucose on glycaemic variability in non-insulin treated type 2 diabetes: The SMBG study, a 12-month randomised controlled trial
David M. Williams, Sharon N. Parsons, Gareth J. Dunseath, Jeffrey W. Stephens, Stephen D. Luzio, David R. Owens
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(2): 101. CrossRef - Model‐based data analysis of individual human postprandial plasma bile acid responses indicates a major role for the gallbladder and intestine
Emma C. E. Meessen, Fianne L. P. Sips, Hannah M. Eggink, Martijn Koehorst, Johannes A. Romijn, Albert K. Groen, Natal A. W. Riel, Maarten R. Soeters
Physiological Reports.2020;[Epub] CrossRef - How tightly controlled do fluctuations in blood glucose levels need to be to reduce the risk of developing complications in people with Type 1 diabetes?
R. Livingstone, J. G. Boyle, J. R. Petrie
Diabetic Medicine.2020; 37(4): 513. CrossRef - Simple Linear Support Vector Machine Classifier Can Distinguish Impaired Glucose Tolerance Versus Type 2 Diabetes Using a Reduced Set of CGM-Based Glycemic Variability Indices
Enrico Longato, Giada Acciaroli, Andrea Facchinetti, Alberto Maran, Giovanni Sparacino
Journal of Diabetes Science and Technology.2020; 14(2): 297. CrossRef - Vascular Complication in Adolescents With Diabetes Mellitus
Lara E. Graves, Kim C. Donaghue
Frontiers in Endocrinology.2020;[Epub] CrossRef - The Association Between Glycemic Variability and Macronutrients in Young Children with T1D
Alexandra D Monzon, Laura B Smith, Scott W Powers, Lawrence M Dolan, Susana R Patton
Journal of Pediatric Psychology.2020; 45(7): 749. CrossRef - Effect of sancai powder on glacemic variability of type 1 diabetes in China
Weiwei Yu, Dongqi Zhou, Li Zhang, Chen Rumeng, Peishuai Zhang, Lisha Sun, Ziping Gao
Medicine.2020; 99(34): e20772. CrossRef - Glycemic variability in newly diagnosed diabetic cats treated with the glucagon‐like peptide‐1 analogue exenatide extended release
Anna L. Krämer, Angelina Riederer, Federico Fracassi, Felicitas S. Boretti, Nadja S. Sieber‐Ruckstuhl, Thomas A. Lutz, Barbara Contiero, Eric Zini, Claudia E. Reusch
Journal of Veterinary Internal Medicine.2020; 34(6): 2287. CrossRef - The Association Between Glycemic Variability and Myocardial Infarction: A Review and Meta-Analysis of Prospective Studies and Randomized Trials
Zinab Alatawi, Hyder Mirghani
Cureus.2020;[Epub] CrossRef - Epigenetic regulation by polyphenols in diabetes and related complications
Hammad Ullah, Anna De Filippis, Cristina Santarcangelo, Maria Daglia
Mediterranean Journal of Nutrition and Metabolism.2020; 13(4): 289. CrossRef - A Protective Role of Paeoniflorin in Fluctuant Hyperglycemia-Induced Vascular Endothelial Injuries through Antioxidative and Anti-Inflammatory Effects and Reduction of PKCβ1
Jing-Shang Wang, Ye Huang, Shuping Zhang, Hui-Jun Yin, Lei Zhang, Yan-Hong Zhang, Ye-Wen Song, Dan-Dan Li
Oxidative Medicine and Cellular Longevity.2019; 2019: 1. CrossRef - The mechanisms of glycemic variability accelerate diabetic central neuropathy and diabetic peripheral neuropathy in diabetic rats
Junpeng Yang, Zhigang Zhao, Huijuan Yuan, Xiangxiang Ma, Yakun Li, Huimeng Wang, Xiaojun Ma, Guijun Qin
Biochemical and Biophysical Research Communications.2019; 510(1): 35. CrossRef - Glucose Variability and Coronary Artery Disease
Jinggang Xia, Chunlin Yin
Heart, Lung and Circulation.2019; 28(4): 553. CrossRef - Phase 1 Study of the Pharmacology of BTI320 Before High‐Glycemic Meals
David R. Luke, Karen Ka Yan Lee, Carl W. Rausch, Camille Cheng
Clinical Pharmacology in Drug Development.2019; 8(3): 395. CrossRef - Information Technology for Supporting Self-Control in the Formation of a Rational Lifestyle for Diabetics Patients
S. KIFORENKO, T. HONTAR, V. ORLENKO, K. IVASKIVA, T. OBELETS
Kibernetika i vyčislitelʹnaâ tehnika.2019; 2019(3(197)): 80. CrossRef - Impact of Carbohydrate on Glucose Variability in Patients with Type 1 Diabetes Assessed Through Professional Continuous Glucose Monitoring: A Retrospective Study
Yi-Hsuan Lin, Yu-Yao Huang, Hsin-Yun Chen, Sheng-Hwu Hsieh, Jui-Hung Sun, Szu-Tah Chen, Chia-Hung Lin
Diabetes Therapy.2019; 10(6): 2289. CrossRef - Tracking the Sugar Rush: Incorporating Continuous Glucose Monitoring Into Multisite Early Clinical Research With Type 2 Diabetes Subjects
Sabina Paglialunga, Bruce H. Morimoto, Amparo de la Peña, Caroline Fortier
Clinical Pharmacology in Drug Development.2018; 7(7): 676. CrossRef - Higher Total Insulin Dose Has Positive Effect on Corneal Nerve Fibers in DM1 Patients
Gabriela Mahelková, Marie Ceská Burdová, Šárka Malá, Lucie Hoskovcová, Dagmar Dotrelová, Katerina Štechová
Investigative Opthalmology & Visual Science.2018; 59(10): 3800. CrossRef - Relationship between Thyroid Function and Kidney Function in Patients with Type 2 Diabetes
Ying Zhang, Yang Wang, Xiao Jun Tao, Qian Li, Feng Fei Li, Kok Onn Lee, Dong Mei Li, Jian Hua Ma
International Journal of Endocrinology.2018; 2018: 1. CrossRef - The correlation between glucose fluctuation from self-monitored blood glucose and the major adverse cardiac events in diabetic patients with acute coronary syndrome during a 6-month follow-up by WeChat application
Jinggang Xia, Shaodong Hu, Ji Xu, Hengjian Hao, Chunlin Yin, Dong Xu
Clinical Chemistry and Laboratory Medicine (CCLM).2018; 56(12): 2119. CrossRef - Glycemic Variability Percentage: A Novel Method for Assessing Glycemic Variability from Continuous Glucose Monitor Data
Thomas A. Peyser, Andrew K. Balo, Bruce A. Buckingham, Irl B. Hirsch, Arturo Garcia
Diabetes Technology & Therapeutics.2018; 20(1): 6. CrossRef - Efficacy and safety of Panax ginseng berry extract on glycemic control: A 12-wk randomized, double-blind, and placebo-controlled clinical trial
Han Seok Choi, Sunmi Kim, Min Jung Kim, Myung-Sunny Kim, Juewon Kim, Chan-Woong Park, Daebang Seo, Song Seok Shin, Sang Woo Oh
Journal of Ginseng Research.2018; 42(1): 90. CrossRef - Resistance to Data Loss of Glycemic Variability Measurements in Long-Term Continuous Glucose Monitoring
Przemysław Kucharski, Konrad Pagacz, Agnieszka Szadkowska, Wojciech Młynarski, Andrzej Romanowski, Wojciech Fendler
Diabetes Technology & Therapeutics.2018; 20(12): 833. CrossRef - Investigation of glucose fluctuations by approaches of multi-scale analysis
Yunyun Lai, Zhengbo Zhang, Peiyao Li, Xiaoli Liu, YiXin Liu, Yi Xin, Weijun Gu
Medical & Biological Engineering & Computing.2018; 56(3): 505. CrossRef - Shared Responsibility for Type 1 Diabetes Care Is Associated With Glycemic Variability and Risk of Glycemic Excursions in Youth
Arwen M Marker, Amy E Noser, Mark A Clements, Susana R Patton
Journal of Pediatric Psychology.2018; 43(1): 61. CrossRef - Self Blood Glucose Monitoring Underestimates Hyperglycemia And Hypoglycemia As Compared To Continuous Glucose Monitoring In Type 1 And Type 2 Diabetes
Devna Mangrola, Christine Cox, Arianne S. Furman, Sridevi Krishnan, Sidika E. Karakas
Endocrine Practice.2018; 24(1): 47. CrossRef - Risk factors for the development of micro-vascular complications of type 2 diabetes in a single-centre cohort of patients
Marsida Teliti, Giulia Cogni, Lucia Sacchi, Arianna Dagliati, Simone Marini, Valentina Tibollo, Pasquale De Cata, Riccardo Bellazzi, Luca Chiovato
Diabetes and Vascular Disease Research.2018; 15(5): 424. CrossRef - Glucotypes reveal new patterns of glucose dysregulation
Heather Hall, Dalia Perelman, Alessandra Breschi, Patricia Limcaoco, Ryan Kellogg, Tracey McLaughlin, Michael Snyder, Jason Locasale
PLOS Biology.2018; 16(7): e2005143. CrossRef - Glucose Outcomes with the In-Home Use of a Hybrid Closed-Loop Insulin Delivery System in Adolescents and Adults with Type 1 Diabetes
Satish K. Garg, Stuart A. Weinzimer, William V. Tamborlane, Bruce A. Buckingham, Bruce W. Bode, Timothy S. Bailey, Ronald L. Brazg, Jacob Ilany, Robert H. Slover, Stacey M. Anderson, Richard M. Bergenstal, Benyamin Grosman, Anirban Roy, Toni L. Cordero, J
Diabetes Technology & Therapeutics.2017; 19(3): 155. CrossRef - Vildagliptin reduces plasma stromal cell‐derived factor‐1α in patients with type 2 diabetes compared with glimepiride
Kyeong Seon Park, SooHeon Kwak, Young Min Cho, Kyong Soo Park, Hak C Jang, Seong Yeon Kim, Hye Seung Jung
Journal of Diabetes Investigation.2017; 8(2): 218. CrossRef - Role of the PKCβII/JNK signaling pathway in acute glucose fluctuation-induced apoptosis of rat vascular endothelial cells
Na Wu, Haitao Shen, Yanjun Wang, Bing He, Yongyan Zhang, Yu Bai, Runyu Du, Qiang Du, Ping Han
Acta Diabetologica.2017; 54(8): 727. CrossRef - Association between glycemic variability and major adverse cardiovascular and cerebrovascular events (MACCE) in patients with acute coronary syndrome during 30-day follow-up
Jinggang Xia, Ji Xu, Boyu Li, Zhi Liu, Hengjian Hao, Chunlin Yin, Dong Xu
Clinica Chimica Acta.2017; 466: 162. CrossRef - How Can We Realize the Clinical Benefits of Continuous Glucose Monitoring?
Ramzi A. Ajjan
Diabetes Technology & Therapeutics.2017; 19(S2): S-27. CrossRef - The efficacy and safety of adding either vildagliptin or glimepiride to ongoing metformin therapy in patients with type 2 diabetes mellitus
Gyuri Kim, Sewon Oh, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee
Expert Opinion on Pharmacotherapy.2017; 18(12): 1179. CrossRef - Association Between Coronary Artery Calcification and the Hemoglobin Glycation Index: The Kangbuk Samsung Health Study
Eun-Jung Rhee, Jung-Hwan Cho, Hyemi Kwon, Se Eun Park, Cheol-Young Park, Ki-Won Oh, Sung-Woo Park, Won-Young Lee
The Journal of Clinical Endocrinology & Metabolism.2017; 102(12): 4634. CrossRef - Glucose variability for cardiovascular risk factors in type 2 diabetes: a meta-analysis
Shuang Liang, Hang Yin, Chunxiang Wei, Linjun Xie, Hua He, Xiaoquan Liu
Journal of Diabetes & Metabolic Disorders.2017;[Epub] CrossRef - Could angiotensin-(1–7) be connected with improvement of microvascular function in diabetic patients? Angiotensin-(1–7) iontophoresis may provide the answer
Aleksandar Kibel
Medical Hypotheses.2016; 93: 16. CrossRef - Efficacy and Safety of PDM011011 Capsules as Compared to Metformin in Subjects with Type-2 Diabetes Mellitus: An Open-Label, Randomized, Active-Controlled, Multicentric, Phase III Study
Ashish C. Suthar, Vikas G. Pai, Yogesh Kadam, Aniruddha Tongaonkar, Shailaja Kale, Atul B. Deshpande, Sharat Kolke, Snehal Tanna, Shrikant V. Deshpande, Purvi Chawla, Debjit Biswas, Somesh Sharma
Journal of Diabetes Mellitus.2016; 06(01): 38. CrossRef - 1,5-Anhydro-D-Glucitol Could Reflect Hypoglycemia Risk in Patients with Type 2 Diabetes Receiving Insulin Therapy
Min Kyeong Kim, Hye Seung Jung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Endocrinology and Metabolism.2016; 31(2): 284. CrossRef - The impact of glycemic variability on diabetic peripheral neuropathy
Heung Yong Jin, Kyung Ae Lee, Tae Sun Park
Endocrine.2016; 53(3): 643. CrossRef - Serum bilirubin levels are positively associated with glycemic variability in women with type 2 diabetes
Lee Kyung Kim, Eun Roh, Min Joo Kim, Min Kyeong Kim, Kyeong Seon Park, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Hye Seung Jung
Journal of Diabetes Investigation.2016; 7(6): 874. CrossRef - Wider Perioperative Glycemic Fluctuations Increase Risk of Postoperative Acute Kidney Injury
Ming Ann Sim, Weiling Liu, Roderica R.G. Ng, Lian Kah Ti, Sophia T.H. Chew
Medicine.2015; 94(44): e1953. CrossRef
- Glycemic variability is associated with sural nerve conduction velocity in outpatients with type 2 diabetes: Usefulness of a new point‐of‐care device for nerve conduction studies


 KES
KES

 First
First Prev
Prev



