Search
- Page Path
- HOME > Search
- Thyroid
- Phospholipase C-γ as a Potential Therapeutic Target for Graves’ Orbitopathy
- Tae Hoon Roh, Min Kyung Chae, Jae Sang Ko, Don O. Kikkawa, Sun Young Jang, Jin Sook Yoon
- Endocrinol Metab. 2023;38(6):739-749. Published online November 21, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1780
- 1,576 View
- 95 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
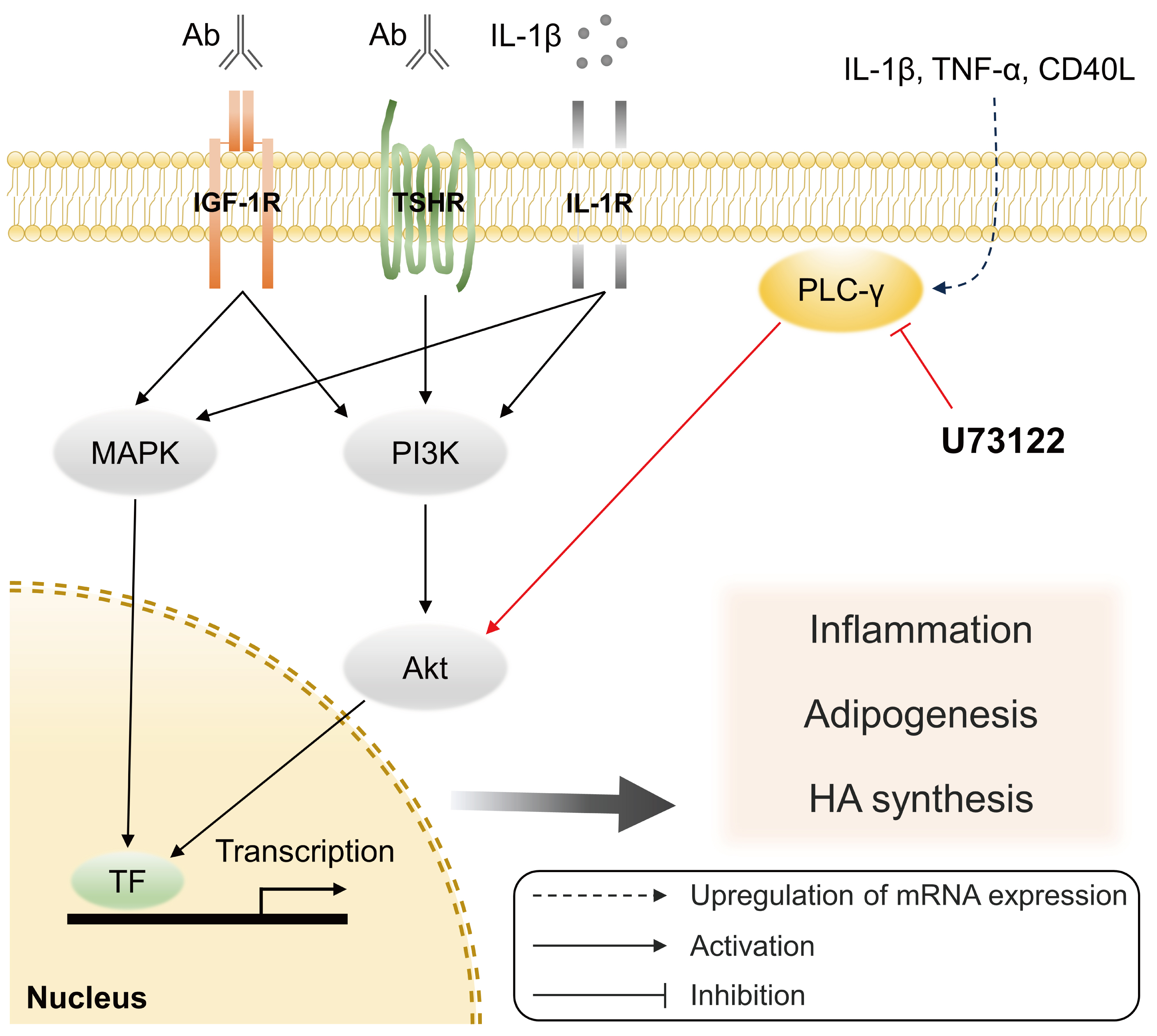
Phospholipase C-γ (PLC-γ) plays a crucial role in immune responses and is related to the pathogenesis of various inflammatory disorders. In this study, we investigated the role of PLC-γ and the therapeutic effect of the PLC-specific inhibitor U73122 using orbital fibroblasts from patients with Graves’ orbitopathy (GO).
Methods
The expression of phospholipase C gamma 1 (PLCG1) and phospholipase C gamma 2 (PLCG2) was evaluated using polymerase chain reaction in GO and normal orbital tissues/fibroblasts. The primary cultures of orbital fibroblasts were treated with non-toxic concentrations of U73122 with or without interleukin (IL)-1β to determine its therapeutic efficacy. The proinflammatory cytokine levels and activation of downstream signaling molecules were determined using Western blotting.
Results
PLCG1 and PLCG2 mRNA expression was significantly higher in GO orbital tissues than in controls (P<0.05). PLCG1 and PLCG2 mRNA expression was significantly increased (P<0.05) in IL-1β, tumor necrosis factor-α, and a cluster of differentiation 40 ligand-stimulated GO fibroblasts. U73122 significantly inhibited the IL-1β-induced expression of proinflammatory molecules, including IL-6, IL-8, monocyte chemoattractant protein-1, cyclooxygenase-2, and intercellular adhesion molecule-1 (ICAM-1), and phosphorylated protein kinase B (p-Akt) and p38 (p-p38) kinase in GO fibroblasts, whereas it inhibited IL-6, IL-8, and ICAM-1, and p-Akt and c-Jun N-terminal kinase (p-JNK) in normal fibroblasts (P<0.05).
Conclusion
PLC-γ-inhibiting U73122 suppressed the production of proinflammatory cytokines and the phosphorylation of Akt and p38 kinase in GO fibroblasts. This study indicates the implications of PLC-γ in GO pathogenesis and its potential as a therapeutic target for GO.

- Diabetes, Obesity and Metabolism
- Human Leukocyte Antigens and Biomarkers in Type 1 Diabetes Mellitus Induced by Immune-Checkpoint Inhibitors
- Hidefumi Inaba, Yosuke Kaido, Saya Ito, Tomonao Hirobata, Gen Inoue, Takakazu Sugita, Yuki Yamamoto, Masatoshi Jinnin, Hiroaki Kimura, Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima, Takaaki Matsuoka
- Endocrinol Metab. 2022;37(1):84-95. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1282
- 4,216 View
- 159 Download
- 16 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 1 diabetes mellitus induced by immune-checkpoint inhibitors (ICI-T1DM) is a rare critical entity. However, the etiology of ICI-T1DM remains unclear.
Methods
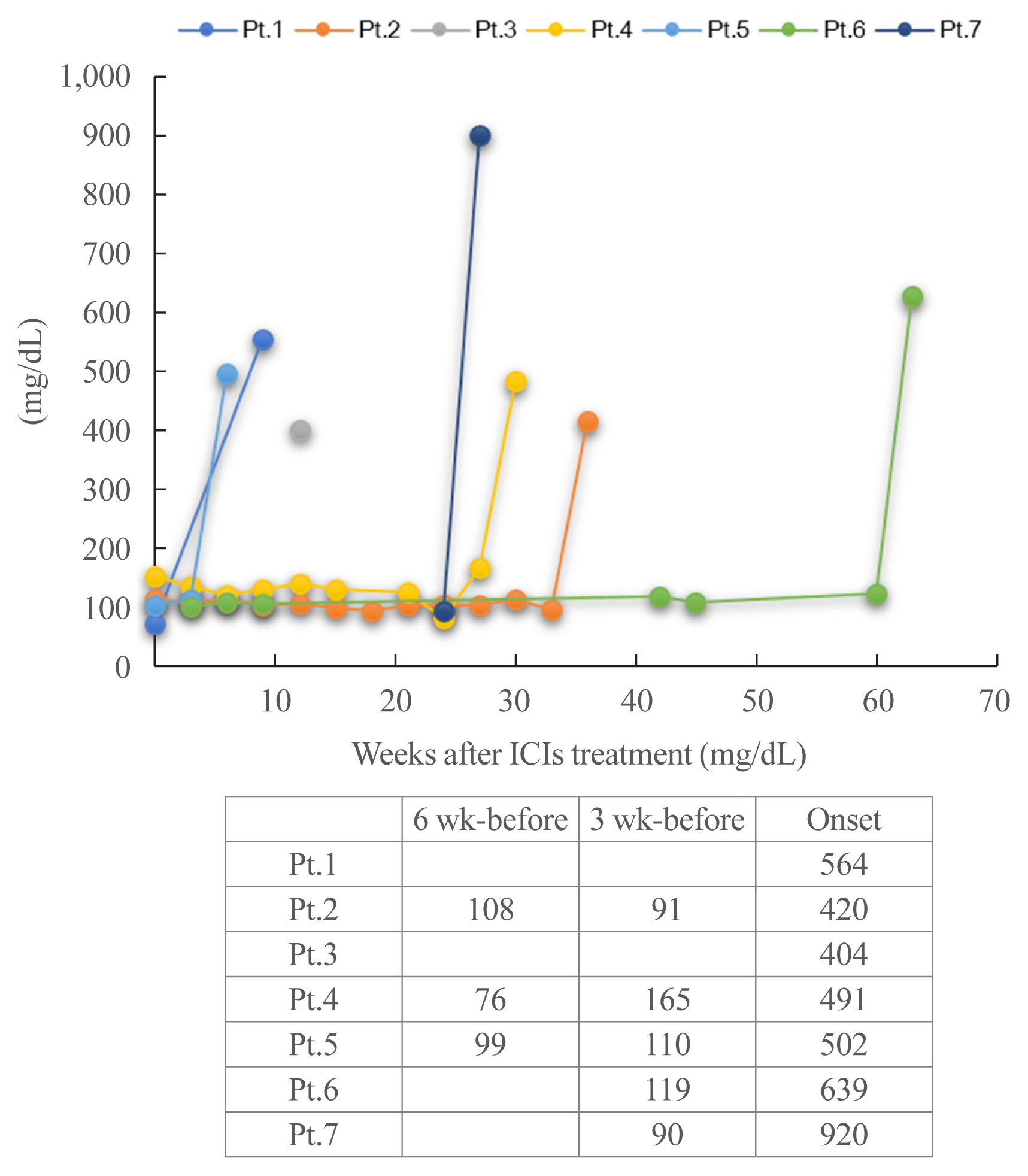
In order to elucidate risk factors for ICI-T1DM, we evaluated the clinical course and immunological status of patients with ICI-T1DM who had been diagnosed during 2016 to 2021.
Results
Seven of 871 (0.8%, six men and one woman) patients developed ICI-T1DM. We revealed that the allele frequencies of human leukocyte antigen (HLA)-DPA1*02:02 and DPB1*05:01 were significantly higher in the patients with ICI-T1DM In comparison to the controls who received ICI (11/14 vs. 10/26, P=0.022; 11/14 vs. 7/26, P=0.0027, respectively). HLA-DRB1*04:05, which has been found to be a T1DM susceptibility allele in Asians, was also observed as a high-risk allele for ICI-T1DM. The significance of the HLA-DPB1*05:01 and DRB1*04:05 alleles was confirmed by an analysis of four additional patients. The absolute/relative neutrophil count, neutrophils-lymphocyte ratio, and neutrophil-eosinophil ratio increased, and the absolute lymphocyte count and absolute/relative eosinophil count decreased at the onset as compared with 6 weeks before. In two patients, alterations in cytokines and chemokines were found at the onset.
Conclusion
Novel high-risk HLA alleles and haplotypes were identified in ICI-T1DM, and peripheral blood factors may be utilized as biomarkers. -
Citations
Citations to this article as recorded by- Type 1 diabetes mellitus affected by potential toxicity from long-term use of nivolumab
Yuma Motomura, Shin Urai, Yushi Hirota, Naoki Takegawa, Hironori Bando, Masaaki Yamamoto, Hidenori Fukuoka, Masahiro Tsuda, Wataru Ogawa
Diabetology International.2024; 15(1): 130. CrossRef - Review – The impact of pharmacogenetics on the outcome of immune checkpoint inhibitors
Karlijn de Joode, Niels Heersche, Edwin A. Basak, Sander Bins, Astrid A.M. van der Veldt, Ron H.N. van Schaik, Ron H.J. Mathijssen
Cancer Treatment Reviews.2024; 122: 102662. CrossRef - Reaching the Diagnosis of Checkpoint Inhibitor-Induced Diabetes Mellitus in Different Clinical Scenarios: A Real-World Application of Updated Diagnostic Criteria
Anna Angelousi, Dimitrios C. Ziogas, Vasiliki Siampanopoulou, Chrysoula Mytareli, Amalia Anastasopoulou, George Lyrarakis, Helen Gogas
Diseases.2024; 12(2): 40. CrossRef - Non-Invasive Predictive Biomarkers for Immune-Related Adverse Events Due to Immune Checkpoint Inhibitors
Ben Ponvilawan, Abdul Wali Khan, Janakiraman Subramanian, Dhruv Bansal
Cancers.2024; 16(6): 1225. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - A single center case series of immune checkpoint inhibitor-induced type 1 diabetes mellitus, patterns of disease onset and long-term clinical outcome
John Marsiglio, Jordan P. McPherson, Magdalena Kovacsovics-Bankowski, Joanne Jeter, Christos Vaklavas, Umang Swami, Douglas Grossmann, Alyssa Erickson-Wayman, Heloisa P. Soares, Katie Kerrigan, Berit Gibson, Jennifer Anne Doherty, John Hyngstrom, Sheetal
Frontiers in Immunology.2023;[Epub] CrossRef - Predictive Biomarkers for Immune-Related Endocrinopathies following Immune Checkpoint Inhibitors Treatment
Almog Shalit, Panagiotis Sarantis, Evangelos Koustas, Eleni-Myrto Trifylli, Dimitris Matthaios, Michalis V. Karamouzis
Cancers.2023; 15(2): 375. CrossRef - Predictive Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Events
Iñigo Les, Mireia Martínez, Inés Pérez-Francisco, María Cabero, Lucía Teijeira, Virginia Arrazubi, Nuria Torrego, Ana Campillo-Calatayud, Iñaki Elejalde, Grazyna Kochan, David Escors
Cancers.2023; 15(5): 1629. CrossRef - Amino acid polymorphisms in human histocompatibility leukocyte antigen class II and proinsulin epitope have impacts on type 1 diabetes mellitus induced by immune-checkpoint inhibitors
Hidefumi Inaba, Shuhei Morita, Daisuke Kosugi, Yuki Asai, Yosuke Kaido, Saya Ito, Tomonao Hirobata, Gen Inoue, Yuki Yamamoto, Masatoshi Jinnin, Hiroaki Kimura, Masao Ota, Yuko Okudaira, Hiroyasu Nakatani, Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima, T
Frontiers in Immunology.2023;[Epub] CrossRef - Clinical characteristics and human leukocyte antigens in patients with immune checkpoint inhibitor-induced type 1 diabetes and pituitary dysfunction: a single center prospective study
Natsuko Hara, Hirotsugu Suwanai, Fumiyoshi Yakou, Keitaro Ishii, Hajime Iwasaki, Hironori Abe, Jumpei Shikuma, Hiroyuki Sakai, Takashi Miwa, Ryo Suzuki
Endocrine.2023; 81(3): 477. CrossRef - Autoimmunity in immune checkpoint inhibitor‐induced immune‐related adverse events: A focus on autoimmune skin toxicity and pneumonitis
Fiamma Berner, Lukas Flatz
Immunological Reviews.2023; 318(1): 37. CrossRef - Prediction-based prompt levothyroxine replacement to prevent a hypothyroid state after immune-related adverse events involving the thyroid gland
Ichiro Yamauchi, Takuro Hakata, Taku Sugawa, Daisuke Kosugi, Haruka Fujita, Kentaro Okamoto, Yohei Ueda, Toshihito Fujii, Daisuke Taura, Norio Harada, Nobuya Inagaki
Endocrine Journal.2023; 70(10): 987. CrossRef - Key Determinants of Immune-Mediated Adverse Reactions to Oncology Drugs
Yihan Zhou, Shan Ding
Cancers.2023; 15(23): 5622. CrossRef - Risk factors and predictors of immune-related adverse events: implications for patients with non-small cell lung cancer
Majd Issa, Joy Tang, Yizhen Guo, Chris Coss, Thomas A. Mace, Jason Bischof, Mitch Phelps, Carolyn J Presley, Dwight H Owen
Expert Review of Anticancer Therapy.2022; 22(8): 861. CrossRef - Risk Factors and Biomarkers for Immune-Related Adverse Events: A Practical Guide to Identifying High-Risk Patients and Rechallenging Immune Checkpoint Inhibitors
Adithya Chennamadhavuni, Laith Abushahin, Ning Jin, Carolyn J. Presley, Ashish Manne
Frontiers in Immunology.2022;[Epub] CrossRef - Flash Glucose Monitoring and Diabetes Mellitus Induced by Immune Checkpoint Inhibitors: An Approach to Clinical Practice
Pablo Rodríguez de Vera-Gómez, Ana Piñar-Gutiérrez, Raquel Guerrero-Vázquez, Virginia Bellido, Cristóbal Morales-Portillo, María Pilar Sancho-Márquez, Pablo Espejo-García, Noelia Gros-Herguido, Gema López-Gallardo, María Asunción Martínez-Brocca, Alfonso
Journal of Diabetes Research.2022; 2022: 1. CrossRef
- Type 1 diabetes mellitus affected by potential toxicity from long-term use of nivolumab

- Diabetes, Obesity and Metabolism
- Association of Protein Z with Prediabetes and Type 2 Diabetes
- Yun-Ui Bae, Ji Hong You, Nan Hee Cho, Leah Eunjung Kim, Hye Min Shim, Jae-Hyung Park, Ho Chan Cho
- Endocrinol Metab. 2021;36(3):637-646. Published online June 2, 2021
- DOI: https://doi.org/10.3803/EnM.2021.962

- 5,171 View
- 147 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) is a progressive metabolic disease. Early detection of prediabetes is important to reduce the risk of T2DM. Some cytokines are known to be associated with T2DM. Therefore, we aimed to identify cytokines as novel biomarkers of glucose dysmetabolism.
Methods
The first stage of the study included 43 subjects (13 subjects with newly diagnosed T2DM, 13 with prediabetes, and 16 with normoglycemia) for cytokine microarray analysis. Blood samples of the subjects were assessed for 310 cytokines to identify potential indicators of prediabetes. The second stage included 142 subjects (36 subjects with T2DM, 35 with prediabetes, and 71 with normoglycemia) to validate the potential cytokines associated with prediabetes.
Results
We identified 41 cytokines that differed by 1.5-fold or more in at least one out of the three comparisons (normoglycemia vs. prediabetes, normoglycemia vs. T2DM, and prediabetes vs. T2DM) among 310 cytokines. Finally, we selected protein Z (PROZ) and validated this finding to determine its association with prediabetes. Plasma PROZ levels were found to be decreased in patients with prediabetes (1,490.32±367.19 pg/mL) and T2DM (1,583.34±465.43 pg/mL) compared to those in subjects with normoglycemia (1,864.07±450.83 pg/mL) (P<0.001). There were significantly negative correlations between PROZ and fasting plasma glucose (P=0.001) and hemoglobin A1c (P=0.010).
Conclusion
PROZ levels were associated with prediabetes and T2DM. We suggest that PROZ may be a promising biomarker for the early detection of prediabetes. Further large-scale studies are needed to evaluate the relationship and mechanism between PROZ and prediabetes and T2DM. -
Citations
Citations to this article as recorded by- On the human health benefits of microalgal phytohormones: An explorative in silico analysis
Angelo Del Mondo, Annamaria Vinaccia, Luigi Pistelli, Christophe Brunet, Clementina Sansone
Computational and Structural Biotechnology Journal.2023; 21: 1092. CrossRef - Role of F-box WD Repeat Domain Containing 7 in Type 1 Diabetes
Sarah W. Mohammed, Zainab M. Qassam, Ekhlass M. Taha, Nameer M. Salih
Ibn AL-Haitham Journal For Pure and Applied Sciences.2023; 36(3): 167. CrossRef - Identification of Protein Z as a Potential Novel Biomarker for the Diagnosis of Prediabetes
Seung-Hoi Koo
Endocrinology and Metabolism.2021; 36(3): 572. CrossRef - Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
Ji Hong You, Yun-Ui Bae, Ho Chan Cho
Endocrinology and Metabolism.2021; 36(5): 1149. CrossRef - Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
Tiffany Pascreau, Maia Tchikviladze, Emilie Jolly, Sara Zia-Chahabi, Bertrand Lapergue, Marc Vasse
Endocrinology and Metabolism.2021; 36(5): 1147. CrossRef
- On the human health benefits of microalgal phytohormones: An explorative in silico analysis

- Clinical Study
- Cardiac Dysfunction in Association with Increased Inflammatory Markers in Primary Aldosteronism
- Jung Soo Lim, Sungha Park, Sung Il Park, Young Taik Oh, Eunhee Choi, Jang Young Kim, Yumie Rhee
- Endocrinol Metab. 2016;31(4):567-576. Published online November 3, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.567
- Correction in: Endocrinol Metab 2020;35(3):671
- 5,376 View
- 43 Download
- 15 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Oxidative stress in primary aldosteronism (PA) is thought to worsen aldosterone-induced damage by activating proinflammatory processes. Therefore, we investigated whether inflammatory markers associated with oxidative stress is increased with negative impacts on heart function as evaluated by echocardiography in patients with PA.
Methods Thirty-two subjects (mean age, 50.3±11.0 years; 14 males, 18 females) whose aldosterone-renin ratio was more than 30 among patients who visited Severance Hospital since 2010 were enrolled. Interleukin-1β (IL-1β), IL-6, IL-8, monocyte chemoattractant protein 1, tumor necrosis factor α (TNF-α), and matrix metalloproteinase 2 (MMP-2), and MMP-9 were measured. All patients underwent adrenal venous sampling with complete access to both adrenal veins.
Results Only MMP-2 level was significantly higher in the aldosterone-producing adenoma (APA) group than in the bilateral adrenal hyperplasia (BAH). Patients with APA had significantly higher left ventricular (LV) mass and A velocity, compared to those with BAH. IL-1β was positively correlated with left atrial volume index. Both TNF-α and MMP-2 also had positive linear correlation with A velocity. Furthermore, MMP-9 showed a positive correlation with LV mass, whereas it was negatively correlated with LV end-systolic diameter.
Conclusion These results suggest the possibility that some of inflammatory markers related to oxidative stress may be involved in developing diastolic dysfunction accompanied by LV hypertrophy in PA. Further investigations are needed to clarify the role of oxidative stress in the course of cardiac remodeling.
-
Citations
Citations to this article as recorded by- 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef - The role of the mineralocorticoid receptor in immune cells in cardiovascular disease
Charlotte D. C. C. van der Heijden, Marlies Bode, Niels P. Riksen, Ulrich O. Wenzel
British Journal of Pharmacology.2022; 179(13): 3135. CrossRef - Prevalence and clinical characteristics of primary aldosteronism in a tertiary-care center in Korea
Minjae Yoon, Namki Hong, Jaehyung Ha, Chan Joo Lee, Cheol Ryong Ku, Yumie Rhee, Sungha Park
Hypertension Research.2022; 45(9): 1418. CrossRef - Functional Characteristic and Significance of Aldosterone-Producing Cell Clusters in Primary Aldosteronism and Age-Related Hypertension
Fatin Athirah Pauzi, Elena Aisha Azizan
Frontiers in Endocrinology.2021;[Epub] CrossRef - Aldosterone-Regulating Receptors and Aldosterone-Driver Somatic Mutations
Jung Soo Lim, Samuel W. Plaska, Juilee Rege, William E. Rainey, Adina F. Turcu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Time-Dependent Risk of Atrial Fibrillation in Patients With Primary Aldosteronism After Medical or Surgical Treatment Initiation
Kyoung Jin Kim, Namki Hong, Min Heui Yu, Hokyou Lee, Seunghyun Lee, Jung Soo Lim, Yumie Rhee
Hypertension.2021; 77(6): 1964. CrossRef - Serum Matrix Metalloproteinases and Left Atrial Remodeling—The Hoorn Study
Pauline B. C. Linssen, Hans-Peter Brunner-La Rocca, Casper G. Schalkwijk, Joline W. J. Beulens, Petra J. M. Elders, Amber A. van der Heijden, Roderick C. Slieker, Coen D. A. Stehouwer, Ronald M. A. Henry
International Journal of Molecular Sciences.2020; 21(14): 4944. CrossRef - Endothelial Dysfunction in Primary Aldosteronism
Zheng-Wei Chen, Cheng-Hsuan Tsai, Chien-Ting Pan, Chia-Hung Chou, Che-Wei Liao, Chi-Sheng Hung, Vin-Cent Wu, Yen-Hung Lin
International Journal of Molecular Sciences.2019; 20(20): 5214. CrossRef - IL-6 trans-signalling contributes to aldosterone-induced cardiac fibrosis
Chia-Hung Chou, Chi-Sheng Hung, Che-Wei Liao, Lin-Hung Wei, Ching-Way Chen, Chia-Tung Shun, Wen-Fen Wen, Cho-Hua Wan, Xue-Ming Wu, Yi-Yao Chang, Vin-Cent Wu, Kwan-Dun Wu, Yen-Hung Lin
Cardiovascular Research.2018; 114(5): 690. CrossRef - European Heart Rhythm Association (EHRA) position paper on arrhythmia management and device therapies in endocrine disorders, endorsed by Asia Pacific Heart Rhythm Society (APHRS) and Latin American Heart Rhythm Society (LAHRS)
Bulent Gorenek, Giuseppe Boriani, Gheorge-Andrei Dan, Laurent Fauchier, Guilherme Fenelon, He Huang, Gulmira Kudaiberdieva, Gregory Y H Lip, Rajiv Mahajan, Tatjana Potpara, Juan David Ramirez, Marc A Vos, Francisco Marin, Carina Blomstrom-Lundqvist, Aldo
EP Europace.2018; 20(6): 895. CrossRef - Effects of Altered Calcium Metabolism on Cardiac Parameters in Primary Aldosteronism
Jung Soo Lim, Namki Hong, Sungha Park, Sung Il Park, Young Taik Oh, Min Heui Yu, Pil Yong Lim, Yumie Rhee
Endocrinology and Metabolism.2018; 33(4): 485. CrossRef - The mineralocorticoid receptor as a modulator of innate immunity and atherosclerosis
Charlotte D C C van der Heijden, Jaap Deinum, Leo A B Joosten, Mihai G Netea, Niels P Riksen
Cardiovascular Research.2018; 114(7): 944. CrossRef
- 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism

- The Changes of Cytokines and Bone Turnover Markers after Bone Marrow Transplantation.
- Won Young Lee, Moo Il Kang, Ki Won Oh, Hye Soo Kim, Seong Dae Mun, Je Ho Han, Hyun Shik Son, Sung Koo Kang, Wan Sik Shin, Woo Sung Min, Choon Choo Kim
- J Korean Endocr Soc. 2000;15(1):85-96. Published online January 1, 2001
- 982 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Loss of bone mass is usually detected after BMT. The causes of bone loss are related with gonadal dysfunction and immunosuppressants. Cytokines, especially IL-6, play an important role in the pathogenesis of postmenopausal osteoporosis. However, the pathogenetic role of cytokines in post-BMT bone loss is unknown and data on the changes of cytokines in accordance with bone turnover markers are scarce. The aim of this study is to assess the relationship of bone turnover markers and cytokines of peripheral blood and bone marrow before and after allogeneic BMT. METHODS: This prospective study included two analyses. The first was a study of 46 BMT recipients, examining the relationship between bone turnover markers and cytokines of serum which were measured before and 1, 2, 3, 4 week and 3 months after BMT. The second was a study of 14 BMT patients, measuring bone marrow plasma cytokines such as IL-6 and TNF-alpha at post-BMT 3 week and bone turnover marker at the same time to assess the relationship between two parameters. RESULTS: Serum ICTP, bone resorption marker, increased progressively until 4 weeks (peak) after BMT and then decreased thereafter. Serum osteocalcin, bone formation marker, decreased progressively until 3 weeks after BMT and then increased thereafter. There was positive correlation between serum ICTP and bone marrow IL-6 levels at the post-BMT 3 week with a statistical significance, but the correlation between bone turnover markers and bone marrow TNF-alpha or peripheral blood cytokines was not found. CONCLUSION: Our data suggest that the progressive increase of bone resorption after BMT is related with the increase of bone marrow IL-6, which is a potent stimulator of bone resorption in vivo.


 KES
KES

 First
First Prev
Prev



