Articles
- Page Path
- HOME > Endocrinol Metab > Volume 31(4); 2016 > Article
-
Original ArticleClinical Study Obesity and Hyperglycemia in Korean Men with Klinefelter Syndrome: The Korean Endocrine Society Registry
-
Seung Jin Han1, Kyung-Soo Kim2, Wonjin Kim3, Jung Hee Kim4, Yong-ho Lee5, Ji Sun Nam6, Ji A Seo7, Bu Kyung Kim8, Jihyun Lee9, Jin Ook Chung10, Min-Hee Kim11, Tae-Seo Sohn11, Han Seok Choi12, Seong Bin Hong13, Yoon-Sok Chung1

-
Endocrinology and Metabolism 2016;31(4):598-603.
DOI: https://doi.org/10.3803/EnM.2016.31.4.598
Published online: December 20, 2016
1Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
2Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
3Department of Internal Medicine, CHA Gangnam Medical Center, CHA University, Seoul, Korea.
4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
6Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
7Division of Endocrinology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
8Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea.
9Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea.
10Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
11Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
12Division of Endocrinology and Metabolism, Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea.
13Department of Endocrinology, Inha University School of Medicine, Incheon, Korea.
- Corresponding author: Yoon-Sok Chung. Department of Endocrinology and Metabolism, Ajou University School of Medicine, 164 World cup-ro, Yeongtong-gu, Suwon 16499, Korea. Tel: +82-31-219-5127, Fax: +82-31-219-4497, yschung@ajou.ac.kr
Copyright © 2016 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- The aim of this study was to investigate the prevalence of obesity in Korean men with Klinefelter syndrome (KS) and the associated risk factors for obesity and hyperglycemia.
-
Methods
- Data were collected retrospectively from medical records from 11 university hospitals in Korea between 1994 and 2014. Subjects aged ≥18 years with newly diagnosed KS were enrolled. The following parameters were recorded at baseline before treatment: chief complaint, height, weight, fasting glucose level, lipid panel, blood pressure, testosterone, luteinizing hormone, follicle-stimulating hormone, karyotyping patterns, and history of hypertension, diabetes, and dyslipidemia.
-
Results
- Data were analyzed from 376 of 544 initially enrolled patients. The rate of the 47 XXY chromosomal pattern was 94.1%. The prevalence of obesity (body mass index ≥25 kg/m2) in Korean men with KS was 42.6%. The testosterone level was an independent risk factor for obesity and hyperglycemia.
-
Conclusion
- Obesity is common in Korean men with KS. Hypogonadism in patients with KS was associated with obesity and hyperglycemia.
- Klinefelter syndrome (KS) is the most frequent sex chromosome disorder in men, with a prevalence of 1:500 to 1:1,000 live births [1]. KS is caused by the presence of one or more additional X chromosomes. The 47 XXY karyotype is the most common classical chromosomal abnormality in subjects with KS, although both mosaic patterns and KS variants with supernumerary X or Y chromosomes exist [2]. The classical KS phenotype is a tall, slender man with narrow shoulders, long arms and legs, small testes, micropenis, gynecomastia, a lack of pubic hair, infertility, and mild-to-moderate cognitive deficits [3]. However, many patients do not present with the classical symptoms, and men with KS are associated with a broad spectrum of phenotypes, professions, incomes, and socioeconomic statuses [134]. KS in most men remains undetected, and only 25% of those predicted to have KS are diagnosed [5]. Although it is unknown why so many men with KS go their entire lives undiagnosed, it may be due to the lack of pronounced features, since the genotype does not necessarily imply the presence of any classical phenotypic features [67]. Recent studies reported that KS is associated with abdominal obesity and an increased risk of metabolic syndrome [89]. However, only limited data such as case reports describing obesity and metabolic disorders are available in Korean men with KS [10111213]. Therefore, the current study investigated the prevalence of obesity in Korean men with KS and the associated risk factors for obesity and hyperglycemia.
INTRODUCTION
- Subjects
- Medical record data were collected retrospectively from 11 university hospitals in South Korea willing to participate from 1994 to 2014. Subjects aged ≥18 years with newly diagnosed KS were enrolled. The following parameters were examined at baseline before treatment: chief complaint, height, weight, fasting glucose level, lipid panel, blood pressure, total testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), sex chromosomal abnormalities, and histories of hypertension, diabetes, and dyslipidemia. Data from 376 of the 544 patients initially enrolled were analyzed. One hundred and sixty-eight patients were excluded due to an inaccurate diagnosis or missing data regarding body weight, height, or testosterone level. The study was approved by the Institutional Review Boards of Ajou University Hospital and each hospital, and it conformed to the ethical guidelines of the Declaration of Helsinki. Patient records and information were anonymized and de-identified before analysis.
- Definition
- KS was defined based on a karyotype consisting of X-chromosome polysomy and at least one Y chromosome, either as a single lineage or mosaicism. The definition of obesity was a body mass index (BMI) ≥25 kg/m2 [14]. Diabetes was defined as fasting plasma glucose (FPG) ≥126 mg/dL, glycated hemoglobin (HbA1c) ≥6.5%, or current treatment with oral antidiabetes drugs or insulin [15]. Prediabetes was defined as FPG between 100 and 125 mg/dL or an HbA1c of 5.7% to 6.4% and no diagnosis of diabetes [15]. Hyperglycemia was diagnosed if the patient had diabetes, used hypoglycemic agents, or had a FPG ≥100 mg/dL or an HbA1c level ≥5.7%. Hypertension was diagnosed according to a systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or the use of antihypertensive medications [16]. Dyslipidemia was defined as a serum total cholesterol level ≥240 mg/dL, triglyceride level ≥150 mg/dL, low serum high density lipoprotein cholesterol level (<40 mg/dL in men and <50 mg/dL in women), or the use of lipid-lowering agents [17].
- Statistical analysis
- All continuous variables were expressed as mean±standard deviation except age. Independent t tests were used to analyze continuous data. Age was shown as median and total range and nonparametric test was used to test for differences between groups. Categorical variables are expressed as numbers and percentages. Chi-square tests were implemented for categorical data, as appropriate. Pearson correlation analysis was used to describe correlations between variables, and logistic regression analysis was used to evaluate the factors associated with obesity or hyperglycemia. The data were analyzed using SPSS version 22.0 (IBM Co., Armonk, NY, USA). A two-sided P<0.05 was considered statistically significant.
METHODS
- The chief complaints of patients with KS at diagnosis are shown in Table 1. The most common complaints were (in order) infertility, small testicles, sexual dysfunction, and gynecomastia. Table 2 shows the karyotyping results in patients with KS. The proportions of nonmosaic, mosaic, and KS variants were 94.1%, 3.5%, and 2.5%, respectively. The mean patient age and BMI were 32.5±5.9 years and 24.7±3.9 kg/m2, respectively (Table 3). The prevalence of obesity in patients with KS was 42.6%. We found a trend towards an increase in the prevalence of obesity according to age, but there was no significant difference in a subgroup analysis (18 to 29 years [37.5%] vs. 30 to 39 years [43.1%] vs. 40 to 55 years [52.9%], P=0.122). The prevalences of hyperglycemia and dyslipidemia were 38.8% and 19.1%, respectively.
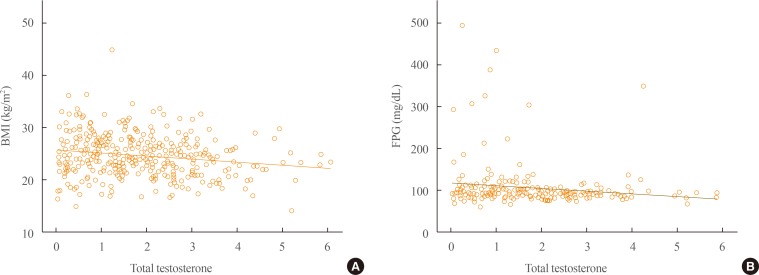
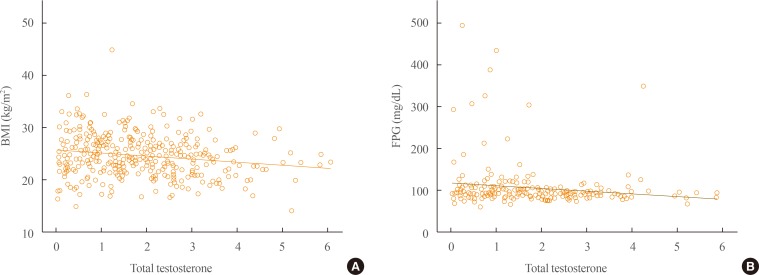
- Obese subjects with KS had a high incidence of hyperglycemia and low testosterone level and elevated LH and FSH levels compared with nonobese patients with KS. Testosterone levels were negatively correlated with BMI (r=−0.178, P=0.001) and FPG levels (r=−0.147, P=0.030) (Fig. 1). In a logistic regression model using obesity as the dichotomous variable, testosterone was the only independent risk factor after adjusting for age and karyotype (classical vs. nonclassical KS; odds ratio, 0.797; 95% confidence interval, 0.671 to 0.948; P=0.010). In a model using hyperglycemia as the dependent variable, testosterone level, BMI, and age were independent risk factors after exclusion of the karyotyping pattern.
RESULTS
- The present study revealed that the prevalence of obesity in Korean men with KS is 42.6%, and that testosterone level is an independent risk factor for obesity and hyperglycemia. Previous studies reported that even though patients with KS have abdominal adiposity, their BMI is often in the normal range due to decreased muscle mass and increased body fat [89]. Although we were unable to compare patients with KS with age-matched healthy controls, the prevalence of obesity, based on the criterion of a BMI ≥25 kg/m2, in Korean men with KS was higher than that in the general Korean male population. According to statistical data from Korea between 1998 and 2014, the prevalence of obesity in men aged ≥19 years was 25.1% to 37.7% [18]. Considering the mean age in the current study population was 32.5 years, the prevalence of obesity in KS seems rather higher than that of the general population. In Argentina, 62.5% of patients with KS had a BMI ≥25 kg/m2 [19].
- Testosterone levels were an independent risk factor for obesity and glucose intolerance in the current study. This result is consistent with previous studies, which showed that testosterone deficiency is a predictor of abdominal obesity and metabolic syndrome [8920]. Testosterone may play a central role in metabolic syndrome and type 2 diabetes by increasing skeletal muscle mass and decreasing abdominal obesity and free fatty acids; therefore, it improves insulin resistance in men with a normal karyotype [21]. However, testosterone treatment in patients with KS does not fully correct the unfavorable body composition, although it is unclear whether adequate levels of testosterone were administered in these studies [822]. Furthermore, increased body fat mass is already present before puberty in boys with KS, which suggests that both genetic abnormalities and testosterone deficiency influence body fat in patients with KS [22].
- Insulin resistance is the major pathogenesis of glucose intolerance in patients with KS [823]. Lee et al. [10] used euglycemic hyperinsulinemic clamps to demonstrate impaired peripheral insulin resistance as the mechanism underlying impaired glucose tolerance in Korean patients with KS. Recent both epidemiology and clinical studies showed clear evidence of a dramatically increased risk of diabetes and metabolic syndrome in KS worldwide [7]. In particular, In Korea, rapid economic development and a westernized lifestyle have resulted in increased rates of obesity [24]. Thus these factors can affect phenotype of KS.
- The median total testosterone level in the current study was in the lower-to-normal range, whereas LH and FSH levels were increased, consistent with previous studies [1891925]. This suggests that hypogonadism in KS is relative rather than absolute [4]. Among patients with KS, 45.1% to 56.5% have low total testosterone levels [1925].
- Less than 10% of the expected number of KS cases are diagnosed during childhood, and 15% to 20% of male KS cases are identified via investigations into the underlying cause of infertility [2627]. The current data are consistent with these previous results, since 73% of patients with KS complained of infertility at the first consultation. Therefore, most Korean men with KS are not diagnosed until adulthood.
- The current study has the strength of including a relatively large sample size. It is also the first report focusing on obesity in Korean patients with KS. Nevertheless, several limitations need to be considered. First, the retrospective design of the study did not allow any missing data to be collected. Relatively few physicians tend to measure metabolic parameters in patients with KS. Second, the present study was cross-sectional in nature, which prevents defining causal relationships. Third, the study was based on data from patients with KS from 11 university hospitals; therefore, the results need to be interpreted with caution before generalizing to the entire Korean population.
- In conclusion, the current study describes the prevalence of obesity in Korean patients with KS for the first time. Hypogonadism is a risk factor for obesity and hyperglycemia in patients with KS.
DISCUSSION
-
Acknowledgements
- This study was funded by a research grant from the Korean Endocrine Society.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
Article information
- 1. Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E. Klinefelter's syndrome. Lancet 2004;364:273–283. ArticlePubMed
- 2. Visootsak J, Aylstock M, Graham JM Jr. Klinefelter syndrome and its variants: an update and review for the primary pediatrician. Clin Pediatr (Phila) 2001;40:639–651. ArticlePubMed
- 3. Smyth CM, Bremner WJ. Klinefelter syndrome. Arch Intern Med 1998;158:1309–1314. ArticlePubMed
- 4. Gravholt CH, Jensen AS, Host C, Bojesen A. Body composition, metabolic syndrome and type 2 diabetes in Klinefelter syndrome. Acta Paediatr 2011;100:871–877. ArticlePubMed
- 5. Bojesen A, Juul S, Birkebaek NH, Gravholt CH. Morbidity in Klinefelter syndrome: a Danish register study based on hospital discharge diagnoses. J Clin Endocrinol Metab 2006;91:1254–1260. ArticlePubMed
- 6. Bird RJ, Hurren BJ. Anatomical and clinical aspects of Klinefelter's syndrome. Clin Anat 2016;29:606–619. ArticlePubMed
- 7. Groth KA, Skakkebaek A, Host C, Gravholt CH, Bojesen A. Clinical review: Klinefelter syndrome: a clinical update. J Clin Endocrinol Metab 2013;98:20–30. ArticlePubMed
- 8. Bojesen A, Kristensen K, Birkebaek NH, Fedder J, Mosekilde L, Bennett P, et al. The metabolic syndrome is frequent in Klinefelter's syndrome and is associated with abdominal obesity and hypogonadism. Diabetes Care 2006;29:1591–1598. ArticlePubMed
- 9. Ishikawa T, Yamaguchi K, Kondo Y, Takenaka A, Fujisawa M. Metabolic syndrome in men with Klinefelter's syndrome. Urology 2008;71:1109–1113. ArticlePubMed
- 10. Lee KW, Cha CK, Uhm C, Kwon OY, Lee SK, Chung YS, et al. Impaired glucose tolerance associated with klinefalter syndrome. J Korean Soc Endocrinol 1998;13:495–500.
- 11. Yoon JY, Hong SM, Park YS, Kim DS, Choi WH, Kim TW, et al. A case of diabetes mellitus associated with Klinefelter's syndrome. Korean J Med 2010;79:701–704.
- 12. Kim Y, Kim WJ, Huh JH, Lee S, Kim D, Hong JW, et al. A 47,X,+t(X;X)(p22.3;p22.3)del(X)(p11.23q11.2),Y Klinefelter variant with morbid obesity. Yonsei Med J 2013;54:538–540. ArticlePubMedPMC
- 13. Lim SH, Bae WH, Kim SJ, Lee YH, Jun IP, Kim SH, et al. Diabetes mellitus in association with Klinefelter syndrome. J Korean Soc Endocrinol 1994;9:46–49.
- 14. WHO West Pacific Region. The Asia-Pacific perspective: redefining obesity and its treatment; Balmain: Health Communications Australia; 2000.
- 15. American Diabetes Association. Standards of medical care in diabetes: 2010. Diabetes Care 2010;33(Suppl 1):S11–S61. ArticlePubMedPMC
- 16. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 2007;75:72–80. ArticlePubMed
- 17. Roh E, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, et al. Prevalence and management of dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010. Diabetes Metab J 2013;37:433–449. ArticlePubMedPMC
- 18. Statistics Korea. Prevalence of obesity [Internet]; Daejeon: Statistics Korea; 2016. cited 2016 Nov 8. Available from:http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=2705.
- 19. Pacenza N, Pasqualini T, Gottlieb S, Knoblovits P, Costanzo PR, Stewart Usher J, et al. Clinical presentation of Klinefelter's syndrome: differences according to age. Int J Endocrinol 2012;2012:324835ArticlePubMedPMCPDF
- 20. van den Bergh JP, Hermus AR, Spruyt AI, Sweep CG, Corstens FH, Smals AG. Bone mineral density and quantitative ultrasound parameters in patients with Klinefelter's syndrome after long-term testosterone substitution. Osteoporos Int 2001;12:55–62. ArticlePubMedPDF
- 21. Marin P, Holmang S, Jonsson L, Sjostrom L, Kvist H, Holm G, et al. The effects of testosterone treatment on body composition and metabolism in middle-aged obese men. Int J Obes Relat Metab Disord 1992;16:991–997. PubMed
- 22. Aksglaede L, Molgaard C, Skakkebaek NE, Juul A. Normal bone mineral content but unfavourable muscle/fat ratio in Klinefelter syndrome. Arch Dis Child 2008;93:30–34. ArticlePubMed
- 23. Pei D, Sheu WH, Jeng CY, Liao WK, Fuh MM. Insulin resistance in patients with Klinefelter's syndrome and idiopathic gonadotropin deficiency. J Formos Med Assoc 1998;97:534–540. PubMed
- 24. Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, et al. Prevalence, awareness, and management of obesity in Korea: data from the Korea National Health and Nutrition Examination Survey (1998-2011). Diabetes Metab J 2014;38:35–43. ArticlePubMedPMC
- 25. Abdel-Razic MM, Abdel-Hamid IA, Elsobky E, El-Dahtory F. Further evidence of the clinical, hormonal, and genetic heterogeneity of Klinefelter syndrome: a study of 216 infertile Egyptian patients. J Androl 2012;33:441–448. ArticlePubMed
- 26. Bojesen A, Juul S, Gravholt CH. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocrinol Metab 2003;88:622–626. ArticlePubMed
- 27. Abramsky L, Chapple J. 47,XXY (Klinefelter syndrome) and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling. Prenat Diagn 1997;17:363–368. ArticlePubMed
References
Correlation among serum testosterone, body mass index (BMI), and fasting plasma glucose (FPG). (A) The association between testosterone and BMI. (B) The association between testosterone and FPG.
Chief Complaint at Diagnosis
Karyotyping of Patients with Klinefelter Syndrome
| Karyotype | Number of patients (%) |
|---|---|
| 47 XXY | 354 (94.1) |
| 46 XY/47 XXY | 13 (3.5) |
| 46 XY/47 XXY/48 XXXY | 3 (0.8) |
| 48 XXXY | 2 |
| 48 XXYY | 1 |
| 46 XY/46 XX/47 XXY | 1 |
| 47 XX, inv (Y) | 1 |
| 47 XXY/48 XXXY | 1 |
Comparison of Characteristics in Obese versus Nonobese Patients with Klinefelter Syndrome
Values are expressed as median (range), mean±SD, or number (%). Diabetes was defined as fasting plasma glucose (FPG) ≥126 mg/dL, glycated hemoglobin (HbA1c) ≥6.5%, or current treatment with oral antidiabetes drugs or insulin. Prediabetes was defined as FPG between 100 and 125 mg/dL or an HbA1c of 5.7% to 6.4% and no diagnosis of diabetes. Hyperglycemia was diagnosed if the patient had diabetes, used hypoglycemic agents, or had a FPG ≥100 mg/dL or an HbA1c level ≥5.7%. Hypertension was diagnosed according to a systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or the use of antihypertensive medications. Dyslipidemia was defined as a serum total cholesterol level ≥240 mg/dL, triglyceride level ≥150 mg/dL, low serum high density lipoprotein cholesterol level (<40 mg/dL in men and <50 mg/dL in women), or the use of lipid-lowering agents. BMI, body mass index; LH, luteinizing hormone; FSH, follicle-stimulating hormone.
an=219; bn=223.
Figure & Data
References
Citations

- A dual-center study of predictive factors for sperm retrieval through microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in men with non-mosaic Klinefelter syndrome
Jong Hyeun Baeck, Tae Jin Kim, Tae Heon Kim, Seung-Ryeol Lee, Dong Soo Park, Hwang Kwon, Ji Eun Shin, Dong Hyeon Lee, Young Dong Yu
Investigative and Clinical Urology.2023; 64(1): 41. CrossRef - Cardiorespiratory fitness in adolescents and young adults with Klinefelter syndrome – a pilot study
Julia Spiekermann, Kathrin Sinningen, Beatrice Hanusch, Michaela Kleber, Michael M. Schündeln, Cordula Kiewert, Heide Siggelkow, Jakob Höppner, Corinna Grasemann
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metabolic Profile in a Cohort of Young Sicilian Patients with Klinefelter’s Syndrome: The Role of Irisin
Stefano Radellini, Valentina Guarnotta, Vincenzo Sciabica, Giuseppe Pizzolanti, Carla Giordano, Vito Angelo Giagulli
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Metabolic and Nutritional Aspects in Paediatric Patients with Klinefelter Syndrome: A Narrative Review
Chiara Mameli, Giulia Fiore, Arianna Sangiorgio, Marta Agostinelli, Giulia Zichichi, Gianvincenzo Zuccotti, Elvira Verduci
Nutrients.2022; 14(10): 2107. CrossRef - Klinefelter syndrome in an adolescent with severe obesity, insulin resistance, and hyperlipidemia, successfully treated with testosterone replacement therapy
Shota Fukuhara, Jun Mori, Hisakazu Nakajima
Clinical Pediatric Endocrinology.2021; 30(3): 127. CrossRef - Glucose metabolic disorder in Klinefelter syndrome: a retrospective analysis in a single Chinese hospital and literature review
Shixuan Liu, Tao Yuan, Shuoning Song, Shi Chen, Linjie Wang, Yong Fu, Yingyue Dong, Yan Tang, Weigang Zhao
BMC Endocrine Disorders.2021;[Epub] CrossRef - What Every Internist-Endocrinologist Should Know about Rare Genetic Syndromes in Order to Prevent Needless Diagnostics, Missed Diagnoses and Medical Complications: Five Years of ‘Internal Medicine for Rare Genetic Syndromes’
Anna G. W. Rosenberg, Minke R. A. Pater, Karlijn Pellikaan, Kirsten Davidse, Anja A. Kattentidt-Mouravieva, Rogier Kersseboom, Anja G. Bos-Roubos, Agnies van Eeghen, José M. C. Veen, Jiske J. van der Meulen, Nina van Aalst-van Wieringen, Franciska M. E. H
Journal of Clinical Medicine.2021; 10(22): 5457. CrossRef - Klinefelter Syndrome and Diabetes
Mark J. O’Connor, Emma A. Snyder, Frances J. Hayes
Current Diabetes Reports.2019;[Epub] CrossRef - Endocrine aspects of Klinefelter syndrome
Adriana Herrera Lizarazo, Michelle McLoughlin, Maria G. Vogiatzi
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(1): 60. CrossRef - Sex differences in metabolism and cardiometabolic disorders
Karthickeyan Chella Krishnan, Margarete Mehrabian, Aldons J. Lusis
Current Opinion in Lipidology.2018; 29(5): 404. CrossRef - Klinefelter Syndrome: Integrating Genetics, Neuropsychology, and Endocrinology
Claus H Gravholt, Simon Chang, Mikkel Wallentin, Jens Fedder, Philip Moore, Anne Skakkebæk
Endocrine Reviews.2018; 39(4): 389. CrossRef - Sex differences in obesity, lipid metabolism, and inflammation—A role for the sex chromosomes?
Temeka Zore, Maria Palafox, Karen Reue
Molecular Metabolism.2018; 15: 35. CrossRef - Klinefelter syndrome, insulin resistance, metabolic syndrome, and diabetes: review of literature and clinical perspectives
Andrea Salzano, Roberta D’Assante, Liam M. Heaney, Federica Monaco, Giuseppe Rengo, Pietro Valente, Daniela Pasquali, Eduardo Bossone, Daniele Gianfrilli, Andrea Lenzi, Antonio Cittadini, Alberto M. Marra, Raffaele Napoli
Endocrine.2018; 61(2): 194. CrossRef - Síndrome de Klinefelter y riesgo cardiovascular
A. Yamaguchi, P. Knoblovits
Hipertensión y Riesgo Vascular.2018; 35(4): 195. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Sex differences in obesity: X chromosome dosage as a risk factor for increased food intake, adiposity and co-morbidities
Karen Reue
Physiology & Behavior.2017; 176: 174. CrossRef - Klinefelter Syndrome with Morbid Obesity Before Bariatric Surgery: A Case Report
Parisa Janmohammadi, Gholamreza Mohammadi-Farsani, Hana Arghavani, Mahmoud Arshad, Tayebeh Mokhber
Journal of Minimally Invasive Surgical Sciences.2017;[Epub] CrossRef - Klinefelter Syndrome and Metabolic Disorder
Ji Cheol Bae
Endocrinology and Metabolism.2016; 31(4): 535. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite