Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Article information
Abstract
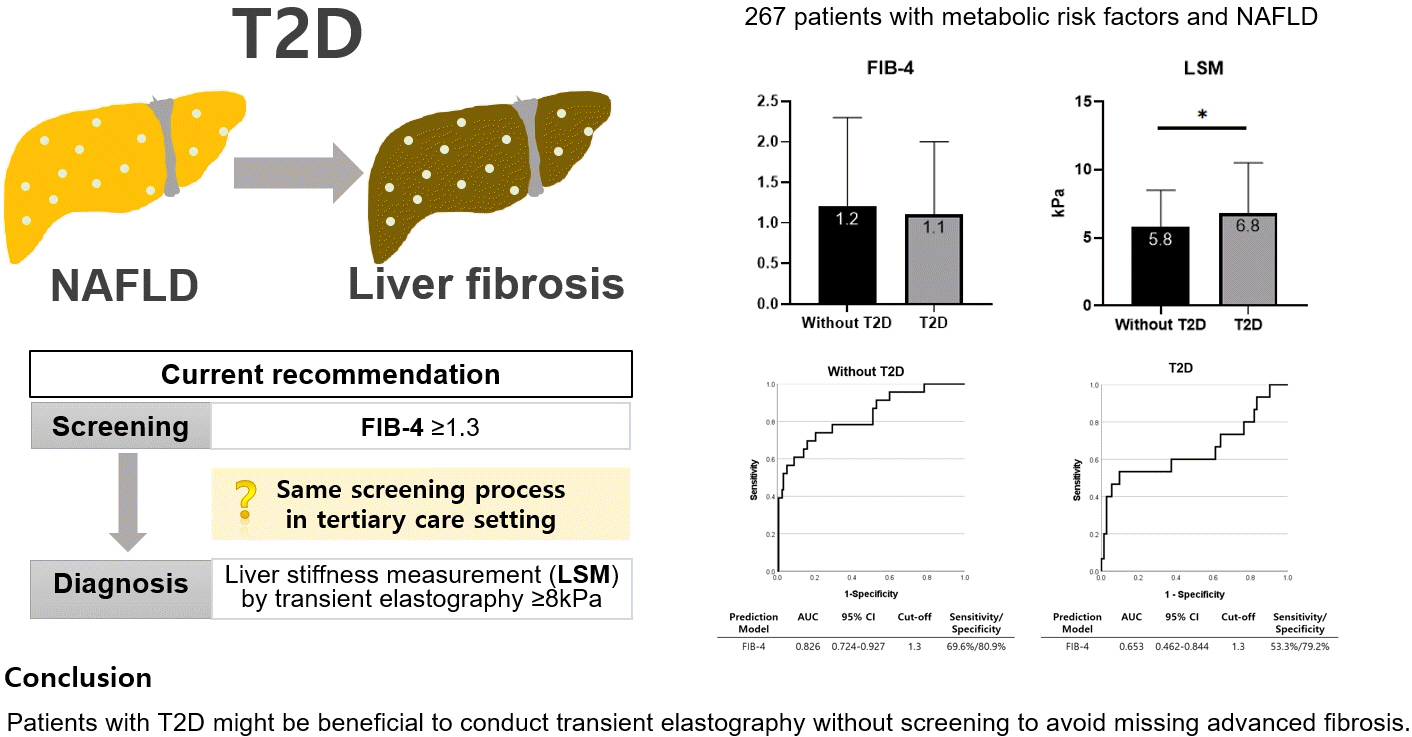
This cross-sectional study enrolled 267 patients with metabolic risk factors and established non-alcoholic fatty liver disease in the prospective cohort. The performance of fibrosis-4 (FIB-4) score (≥1.3) to diagnose advanced fibrosis using transient elastography (liver stiffness measurement [LSM] ≥8 kPa) was analyzed. Comparing patients with type 2 diabetes (T2D, n=87) and without (n=180), not FIB-4, but LSM was significantly higher in T2D (P=0.026). The prevalence of advanced fibrosis was 17.2% in T2D and 12.8% in non-T2D. FIB-4 exhibited higher proportion of false negatives in T2D patients (10.9%) than those without (5.2%). The diagnostic performance of FIB-4 was suboptimal in T2D (area under curve [AUC], 0.653; 95% confidence interval [CI], 0.462 to 0.844) compared to that in non-T2D (AUC, 0.826; 95% CI, 0.724 to 0.927). In conclusion, patients with T2D might be beneficial to conduct transient elastography without screening to avoid missing advanced fibrosis.
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes (T2D) have overlapping pathophysiological conditions, such as insulin resistance, and each disease exacerbates its prognosis [1]. At least one out of six T2D patients have advanced liver fibrosis [2], therefore, proper screening is essential. The fibrosis-4 (FIB-4) score have been proposed as screening tools for detecting liver fibrosis [3]. According to the European Association for the Study of the Liver, in the primary care settings, patients who have metabolic risk factors and FIB-4 levels are above 1.3, transient elastography (TE) is recommended for liver stiffness measurement (LSM) [4]. However, whether to undergo the same screening process in tertiary care settings is questionable. In this study, we aimed to explore the prevalence of advanced fibrosis among NAFLD patients who referred to tertiary care settings and analyze the diagnostic performance of FIB-4 for screening liver fibrosis in patients with T2D, and without.
METHODS
This study conducted a cross-sectional analysis on a cohort of 294 prospective patients who visited and consulted a hepatologist or endocrinologist at the Yeungnam University Hospital, Daegu, South Korea, between July 2020 and December 2021. The inclusion criteria were as follows: (1) patients with metabolic risk factors, including abdominal obesity, elevated triglyceride, reduced high-density lipoprotein cholesterol, elevated blood pressure, and elevated fasting glucose (impaired fasting glucose or T2D) [5]; and (2) patients with fatty liver diagnosed by ultrasound (increased echogenicity of the liver parenchyma relative to that of the cortex of the kidneys, unclear visualization of the intrahepatic vessels, and/or deep beam attenuation) or TE (FibroScan, Echosens, Paris, France; controlled attenuation parameter ≥248 dB/m). TE was performed in all participants. The exclusion criteria were as follows: (1) patients with chronic hepatitis B or C; (2) patients with significant alcohol consumption (>20 g/day in women and >30 g/day in men) [6]; and (3) patients with incomplete data to assess liver fibrosis using simple fibrosis scores or TE. A total of 267 patients were included in the final analysis (Supplemental Fig. S1). The study protocol adhered to the tenets of the Declaration of Helsinki and was reviewed and approved by the Institutional Review Board of Yeungnam University Hospital (approval no. YUMC 2020-06-020). The study was conducted after all patients provided written informed consent.
Anthropometric and biochemical measurements were taken by trained staff members after an 8-hour fast. The T2D was defined as fasting glucose value of ≥126 mg/dL and glycated hemoglobin (HbA1c) levels of ≥6.5%, or those who were previously diagnosed as T2D by an endocrinologist and currently on antidiabetic medication [7]. The simple fibrosis score, FIB-4, was calculated as per equation (1). To rule out advanced fibrosis, established cutoffs for FIB-4 score (1.3) were used [8]. LSM of ≥8 kPa assessed by TE was defined as having advanced fibrosis [4].
AST, aspartate aminotransferase; ALT, alanine aminotransferase.
Statistical analysis was performed using R 4.1.1 for Window (R development Core Team, Vienna, Austria). The clinical characteristics between patient with T2D and without were compared using independent sample t tests and chi-square tests. A receiver operating characteristic (ROC) curve was performed to analyze the area under curve (AUC) of FIB-4 ≥1.3 in predicting advanced fibrosis. AUC above 0.8 is considered as acceptable diagnostic performance in clinical practice. A P value less than 0.05 was considered statistically significant.
RESULTS
The characteristics of patients with T2D (n=87) and those without (n=180) are presented in Supplemental Table S1. The sex distribution, age, body mass index, waist circumference, drinking, smoking status, and liver enzymes did not differ between groups. In patients with T2D, compared to those without, the prevalence of dyslipidemia and proportions of patients taking statin was significantly higher, which might have resulted in significantly lower level of low-density lipoprotein cholesterol. In addition, the HbA1c, fasting glucose, and homeostasis model assessment of insulin resistance levels were significantly higher in patients with T2D compared to those without.
In TE, 38 patients (14.2%) had advanced fibrosis (LSM ≥8 kPa). Comparing patients with T2D and those without, the FIB-4 were not significantly different (Fig. 1A). However, the LSM was significantly higher in patients with T2D compared to those without (Fig. 1B). The advanced fibrosis accounted for 12.8% in patients without T2D and 17.2% in patients with T2D (Table 1). The false-negative rate for FIB-4 was 5.2% in patients without T2D and 10.9% in patients with T2D. The FIB-4 AUC for screening advanced fibrosis was 0.826 in patients without T2D (sensitivity 69.6%, specificity 80.9%) (Fig. 1C), and 0.653 in patients with T2D (sensitivity 53.3%, specificity 79.2%) (Fig. 1D).
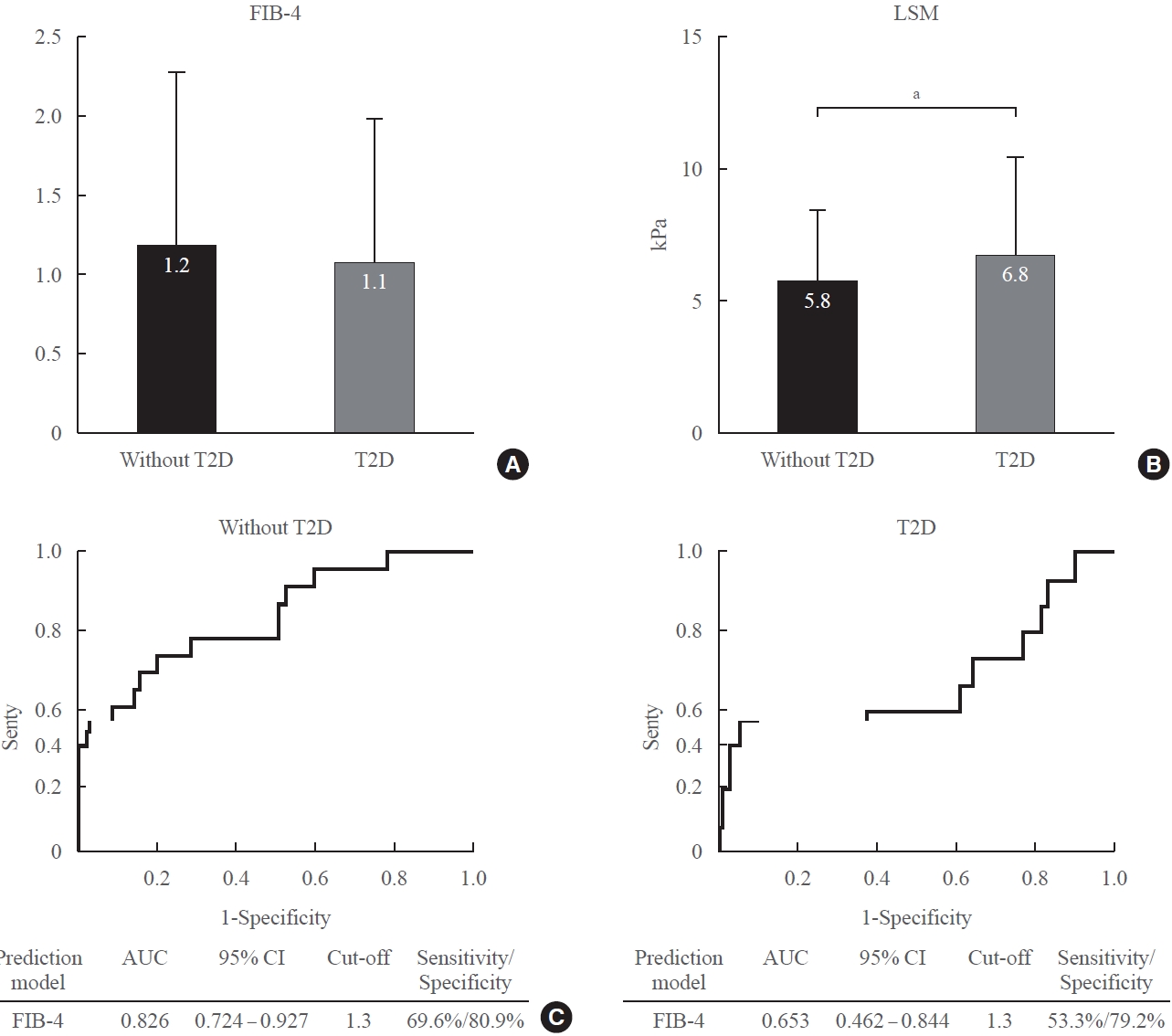
(A, B) Fibrosis-4 (FIB-4) score and transient elastography profiles. Box with annotation indicates mean. Bar indicates standard deviation. (C, D) FIB-4 performance for advanced fibrosis (liver stiffness measurement [LSM] ≥8 kPa) according to the diabetes status. Receiver operating characteristic curve analysis was performed. T2D, type 2 diabetes; AUC, area under curve; CI, confidence interval. aP<0.05.
DISCUSSION
We assessed the diagnostic performance of simple fibrosis marker between patients with T2D and those without. In this cross-sectional study in a tertiary care setting, the prevalence of advanced fibrosis was 14.2%, which was higher than that in general population (2.7% to 6.5%) [9,10], and the diagnostic accuracy of FIB-4 was discrepant with TE results especially in T2D patients.
This discrepancy might be attributed to clinical characteristics of patients with T2D or limitation of fibrosis score formula. As has been noted in earlier reports, the diagnostic performance of simple fibrosis scores was suboptimal in T2D patients [11,12] which might be due to alteration of liver enzymes. A significant proportion of patients with T2D revealed to have advanced liver fibrosis despite of normal transaminase levels [13], and simple fibrosis scores were less accurate predicting cirrhosis or hepatocellular carcinoma [14]. Although liver fibrosis has already progressed for a long time with T2D, biomarkers can be affected by therapeutic factors such as lifestyle modifications, weight loss, and glucose-lowering agents [15]. Thiazolidinedione (TZD), dipeptidyl peptidase-4 inhibitors, glucagon-like peptide-1 receptor agonist (GLP1-RA), and sodium-glucose cotransporter-2 inhibitors (SGLT2i) have shown favorable results, especially improvement of transaminases levels, in patients with both NAFLD and T2D [16,17]. In our study, approximately 6%, 8%, and 40% of patients with T2D were administered TZD, GLP1-RA, and SGLT2i, respectively (Supplemental Table S2). Therefore, simple fibrosis markers using transaminase can be affected by these factors, and cause failure of screening advanced fibrosis. This result was consistent in recent large retrospective cohort study which included over 1,000 patients with biopsy-proven NAFLD [18]. They suggested a new diagnostic algorithm for patients with T2D when suspected advanced fibrosis. We agreed with the suggested algorithm—TE is prioritized and used in patients with T2D not to miss advanced fibrosis, especially when they were prescribed glucose-lowering agents known to be beneficial effects on NAFLD.
Our study has several limitations. First, the sample size was relatively small to represent T2D. Second, the liver fibrosis was not confirmed by liver biopsy. However, the applicability of TE as a surrogate for liver fibrosis has been validated [19], and histological assessment might also mislead the diagnosis due to the uneven distribution of fibrosis [20]. Lastly, as we used the LSM ≥8 kPa as an outcome, we could not assess the diagnostic performance of two-step approaches (FIB-4 followed by TE) for liver fibrosis. Despite these limitations, the strength of this study is that we differentially analyzed the diagnostic performance of simple fibrosis score for screening advanced fibrosis according to the diabetes statuses using well controlled prospective cohort, which was less explored.
Taken together, in patient with T2D, simple fibrosis scores could fail to screen liver fibrosis, and these factors may even conceal the progression of NAFLD. Therefore, it would be better to perform TE first without FIB-4 screening to avoid missing advanced fibrosis, especially in patients with T2D.
Supplementary material
Patient selection flowchart. FIB-4, fibrosis-4; LSM, liver stiffness measurement. aAbdominal obesity, elevated triglyceride, reduced high-density lipoprotein cholesterol, elevated blood pressure, and elevated fasting glucose (impaired fasting glucose or type 2 diabetes); bDiagnosed with ultrasound (increased echogenicity of the liver parenchyma relative to that of the cortex of the kidneys, unclear visualization of the intrahepatic vessels, and/or deep beam attenuation) or transient elastography (TE) (FibroScan; controlled attenuation parameter ≥248 dB/m). TE was performed in all participants; cLiver biopsy was performed if the patented serum tests (cutoffs to use: enhanced liver fibrosis 9.8; FibroMeter 0.45, Fibrotest 0.48) were discordant with LSM.
Baseline Characteristics
Glucose-Lowering Agents Prescribed in Patients with Type 2 Diabetes
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: J.S.M., J.G.P. Acquisition, analysis, or interpretation of data: S.M.C., M.K.K., J.S.M., J.G.P. Drafting the work or revising: S.M.C., J.S.M., J.G.P. Final approval of the manuscript: S.M.C., M.K.K., J.S.M., J.G.P.