Previous issues
- Page Path
- HOME > BROWSE ARTICLES > Previous issues
Review Articles
- Calcium & Bone Metabolism
- Review and Update of the Risk Factors and Prevention of Antiresorptive-Related Osteonecrosis of the Jaw
- Ha Young Kim
- Endocrinol Metab. 2021;36(5):917-927. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1170
- 4,448 View
- 268 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
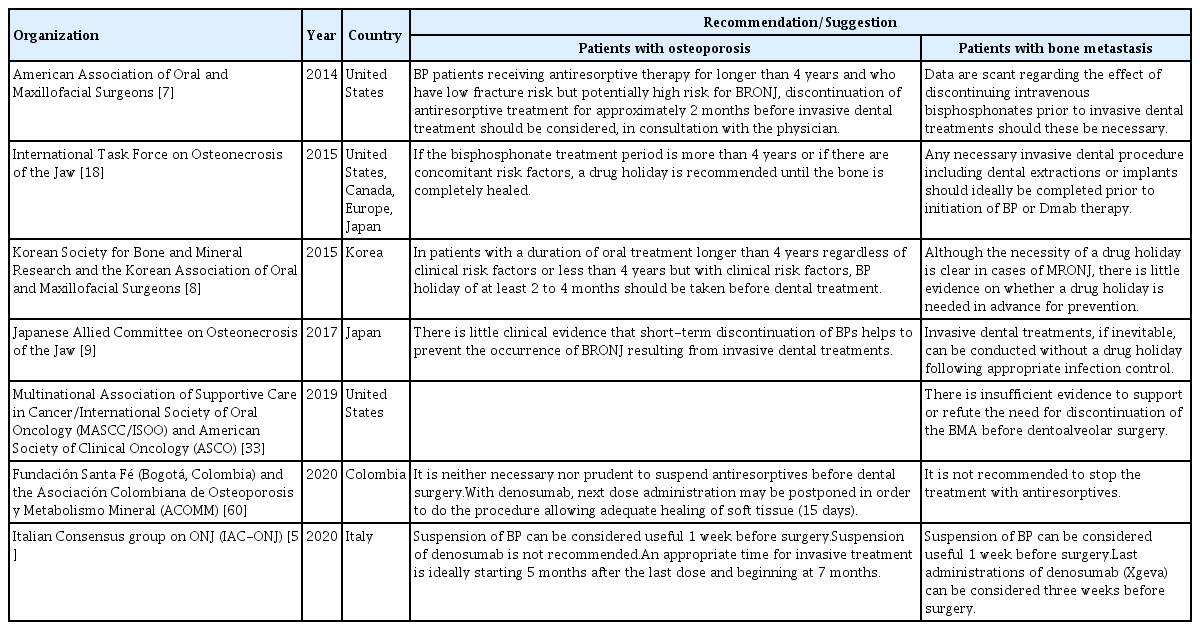
ePub - Antiresorptive-related osteonecrosis of the jaw (ARONJ) is a rare but serious adverse event of bisphosphonate or denosumab administration; it is associated with severe pain and a deteriorated quality of life. Since its first report in 2003, there have been many studies on its definition, epidemiology, pathophysiology, diagnosis, and treatment. Nevertheless, the epidemiology and mechanisms underlying this condition have not yet been fully delineated and several risk factors are known. Moreover, as there is no effective treatment currently available for osteonecrosis of the jaw, prevention is essential. Furthermore, close cooperation between prescribing physicians and dentists is important. The aim of this review was to provide up-to-date information regarding the risk factors and prevention of ARONJ from a physician’s perspective.
-
Citations
Citations to this article as recorded by- Risk factors for dental findings of the development of medication-related osteonecrosis of the jaw: Investigation of 3734 teeth in cancer patients receiving high dose antiresorptive agents
Mitsunobu Otsuru, Yoshinari Fujiki, Sakiko Soutome, Norio Nakamura, Taro Miyoshi, Tomofumi Naruse, Mizuho Ohnuma, Yuka Hotokezaka, Satoshi Rokutanda, Masahiro Umeda
Journal of Dental Sciences.2024; 19(1): 203. CrossRef - Editorial: Immunological processes in maxillofacial bone pathology
Matthias Tröltzsch
Frontiers in Immunology.2024;[Epub] CrossRef - Polysacharide of Agaricus blazei gel mitigates bone necrosis in model of the jaws related to bisphosphonate via Wnt signaling
Vanessa Costa de Sousa, Fátima Regina Nunes Sousa, Raquel Felipe Vasconcelos, Gisele Angelino Barreto, Conceição S. Martins, Nilson Romero Dias, Sislana Costa, Maria Jennifer Chaves Bernardino, George de Almeida Silva, Nadine Linhares, Delane Gondim, Mirn
Scientific Reports.2024;[Epub] CrossRef - When and how to stop denosumab therapy in a patient with osteoporosis
Eirena L. Goulden, Rachel K. Crowley
Clinical Endocrinology.2023; 98(5): 649. CrossRef - Clinical and Histopathological Aspects of MRONJ in Cancer Patients
George Adrian Ciobanu, Laurențiu Mogoantă, Adrian Camen, Mihaela Ionescu, Daniel Vlad, Ionela Elisabeta Staicu, Cristina Maria Munteanu, Mircea Ionuț Gheorghiță, Răzvan Mercuț, Elena Claudia Sin, Sanda Mihaela Popescu
Journal of Clinical Medicine.2023; 12(10): 3383. CrossRef - Bisphosphonates and osteonecrosis of the jaws: Clinical and forensic aspects
Diana Nogueira, Inês Morais Caldas, Ricardo Jorge Dinis-Oliveira
Archives of Oral Biology.2023; 155: 105792. CrossRef - Correlations between Immune Response and Etiopathogenic Factors of Medication-Related Osteonecrosis of the Jaw in Cancer Patients Treated with Zoledronic Acid
George Adrian Ciobanu, Laurențiu Mogoantă, Sanda Mihaela Popescu, Mihaela Ionescu, Cristina Maria Munteanu, Ionela Elisabeta Staicu, Răzvan Mercuț, Cristian Corneliu Georgescu, Monica Scrieciu, Daniel Vlad, Adrian Camen
International Journal of Molecular Sciences.2023; 24(18): 14345. CrossRef - Analysis of the Degree of Information of Dental Surgeons about Antiresorptive Drugs According to the Time Since Graduation in Dentistry
Flávia Godinho Costa Wanderley Rocha, Roberto Paulo Correia de Araújo
Pesquisa Brasileira em Odontopediatria e Clínica Integrada.2023;[Epub] CrossRef - Safety and Efficacy of Pamidronate in Neonatal Hypercalcemia Caused by Subcutaneous Fat Necrosis: A Case Report
Stefano Martinelli, Marco Pitea, Italo Francesco Gatelli, Tara Raouf, Graziano Barera, Ottavio Vitelli
Frontiers in Pediatrics.2022;[Epub] CrossRef - Zoledronic acid for osteoporosis and associated low-energy fractures
S. S. Rodionova, A. F. Kolondaev, A. N. Torgashin, I. A. Solomyannik
Meditsinskiy sovet = Medical Council.2022; (21): 163. CrossRef
- Risk factors for dental findings of the development of medication-related osteonecrosis of the jaw: Investigation of 3734 teeth in cancer patients receiving high dose antiresorptive agents

- Calcium & Bone Metabolism
- Applications of Machine Learning in Bone and Mineral Research
- Sung Hye Kong, Chan Soo Shin
- Endocrinol Metab. 2021;36(5):928-937. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1111

- 4,693 View
- 178 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - In this unprecedented era of the overwhelming volume of medical data, machine learning can be a promising tool that may shed light on an individualized approach and a better understanding of the disease in the field of osteoporosis research, similar to that in other research fields. This review aimed to provide an overview of the latest studies using machine learning to address issues, mainly focusing on osteoporosis and fractures. Machine learning models for diagnosing and classifying osteoporosis and detecting fractures from images have shown promising performance. Fracture risk prediction is another promising field of research, and studies are being conducted using various data sources. However, these approaches may be biased due to the nature of the techniques or the quality of the data. Therefore, more studies based on the proposed guidelines are needed to improve the technical feasibility and generalizability of artificial intelligence algorithms.
-
Citations
Citations to this article as recorded by- Predicting postoperative outcomes in lumbar spinal fusion: development of a machine learning model
Lukas Schönnagel, Thomas Caffard, Tu-Lan Vu-Han, Jiaqi Zhu, Isaac Nathoo, Kyle Finos, Gaston Camino-Willhuber, Soji Tani, Ali. E. Guven, Henryk Haffer, Maximilian Muellner, Artine Arzani, Erika Chiapparelli, Krizia Amoroso, Jennifer Shue, Roland Duculan,
The Spine Journal.2024; 24(2): 239. CrossRef - A CT-based Deep Learning Model for Predicting Subsequent Fracture Risk in Patients with Hip Fracture
Yisak Kim, Young-Gon Kim, Jung-Wee Park, Byung Woo Kim, Youmin Shin, Sung Hye Kong, Jung Hee Kim, Young-Kyun Lee, Sang Wan Kim, Chan Soo Shin
Radiology.2024;[Epub] CrossRef - Applying machine learning classification techniques for disease diagnosis from medical imaging data using Transformer based Attention Guided CNN (TAGCNN)
Saleh Alyahyan
Multimedia Tools and Applications.2024;[Epub] CrossRef - Development and validation of common data model-based fracture prediction model using machine learning algorithm
Sung Hye Kong, Sihyeon Kim, Yisak Kim, Jung Hee Kim, Kwangsoo Kim, Chan Soo Shin
Osteoporosis International.2023; 34(8): 1437. CrossRef - Machine learning algorithms for predicting the risk of fracture in patients with diabetes in China
Sijia Chu, Aijun Jiang, Lyuzhou Chen, Xi Zhang, Xiurong Shen, Wan Zhou, Shandong Ye, Chao Chen, Shilu Zhang, Li Zhang, Yang Chen, Ya Miao, Wei Wang
Heliyon.2023; 9(7): e18186. CrossRef - Leveraging Artificial Intelligence and Machine Learning in Regenerative Orthopedics: A Paradigm Shift in Patient Care
Madhan Jeyaraman, Harish V K Ratna, Naveen Jeyaraman, Aakaash Venkatesan, Swaminathan Ramasubramanian , Sankalp Yadav
Cureus.2023;[Epub] CrossRef - Quality use of artificial intelligence in medical imaging: What do radiologists need to know?
Stacy K Goergen, Helen ML Frazer, Sandeep Reddy
Journal of Medical Imaging and Radiation Oncology.2022; 66(2): 225. CrossRef
- Predicting postoperative outcomes in lumbar spinal fusion: development of a machine learning model

- Thyroid
- T4+T3 Combination Therapy: An Unsolved Problem of Increasing Magnitude and Complexity
- Wilmar M. Wiersinga
- Endocrinol Metab. 2021;36(5):938-951. Published online September 30, 2021
- DOI: https://doi.org/10.3803/EnM.2021.501
- 8,879 View
- 333 Download
- 11 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
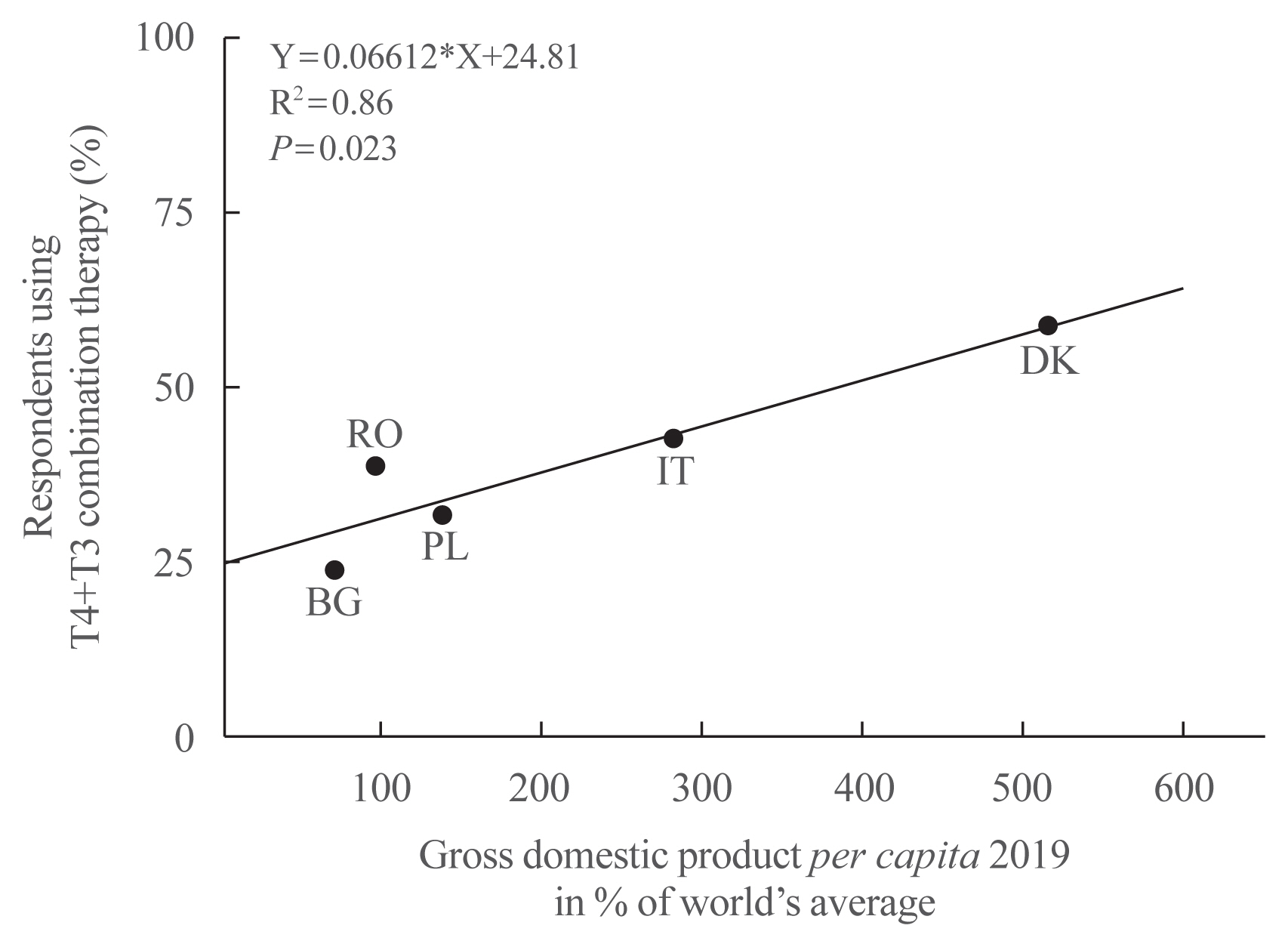
ePub - Thyroxine (T4)+triiodothyronine (T3) combination therapy can be considered in case of persistent symptoms despite normal serum thyroid stimulating hormone in levothyroxine (LT4)-treated hypothyroid patients. Combination therapy has gained popularity in the last two decades, especially in countries with a relatively high gross domestic product. The prevalence of persistent symptoms has also increased; most frequent are complaints about energy levels and fatigue (80% to 90%), weight management (70% to 75%), memory (60% to 80%), and mood (40% to 50%). Pathophysiological explanations for persistent problems are unrealistic patient expectations, comorbidities, somatic symptoms, related disorders (Diagnostic and Statistical Manual of Mental Disorders [DSM-5]), autoimmune neuroinflammation, and low tissue T3. There is fair circumstantial evidence for the latter cause (tissue and specifically brain T3 content is normalized by T4+T3, not by T4 alone), but the other causes are viewed as more relevant in current practice. This might be related to the ‘hype’ that has emerged surrounding T4+T3 therapy. Although more and better-designed trials are needed to validate the efficacy of T4+T3 combination, the management of persistent symptoms should also be directed towards alternative causes. Improving the doctor-patient relationship and including more and better information is crucial. For example, dissatisfaction with the outcomes of T4 treatment for subclinical hypothyroidism can be anticipated as recent trials have demonstrated that LT4 is hardly effective in improving symptoms associated with subclinical hypothyroidism.
-
Citations
Citations to this article as recorded by- Association of DIO2 and MCT10 Polymorphisms With Persistent Symptoms in LT4-Treated Patients in the UK Biobank
Christian Zinck Jensen, Jonas Lynggaard Isaksen, Gustav Ahlberg, Morten Salling Olesen, Birte Nygaard, Christina Ellervik, Jørgen Kim Kanters
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e613. CrossRef - Quality of life, daily functioning, and symptoms in hypothyroid patients on thyroid replacement therapy: A Dutch survey
Ellen Molewijk, Eric Fliers, Koen Dreijerink, Ad van Dooren, Rob Heerdink
Journal of Clinical & Translational Endocrinology.2024; 35: 100330. CrossRef - Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Use of Thyroid Hormones in Hypothyroid and Euthyroid Patients: A THESIS questionnaire survey of members of the Irish Endocrine Society
Mohamad Mustafa, Elsheikh Ali, Anne McGowan, Laura McCabe, Laszlo Hegedüs, Roberto Attanasio, Endre V. Nagy, Enrico Papini, Petros Perros, Carla Moran
Irish Journal of Medical Science (1971 -).2023; 192(5): 2179. CrossRef - Levothyroxine: Conventional and Novel Drug Delivery Formulations
Hanqing Liu, Wei Li, Wen Zhang, Shengrong Sun, Chuang Chen
Endocrine Reviews.2023; 44(3): 393. CrossRef - Re: “Exploring the Genetic Link Between Thyroid Dysfunction and Common Psychiatric Disorders: A Specific Hormonal or a General Autoimmune Comorbidity” by Soheili-Nezhad et al.
Christiaan F. Mooij, A.S. Paul van Trotsenburg
Thyroid®.2023; 33(8): 999. CrossRef - Circulating thyroid hormones and clinical parameters of heart failure in men
Iva Turić, Ivan Velat, Željko Bušić, Viktor Čulić
Scientific Reports.2023;[Epub] CrossRef - Evaluation of cortical and trabecular bone structure of the mandible in patients using L-Thyroxine
Melike Gulec, Melek Tassoker, Mediha Erturk
BMC Oral Health.2023;[Epub] CrossRef - The Impact of Hypothyroidism on Satisfaction with Care and Treatment and Everyday Living: Results from E-Mode Patient Self-Assessment of Thyroid Therapy, a Cross-Sectional, International Online Patient Survey
Petros Perros, Laszlo Hegedüs, Endre Vezekenyi Nagy, Enrico Papini, Harriet Alexandra Hay, Juan Abad-Madroñero, Amy Johanna Tallett, Megan Bilas, Peter Lakwijk, Alan J. Poots
Thyroid.2022;[Epub] CrossRef
- Association of DIO2 and MCT10 Polymorphisms With Persistent Symptoms in LT4-Treated Patients in the UK Biobank

- Thyroid
- Deiodinases and the Three Types of Thyroid Hormone Deiodination Reactions
- Laura Sabatino, Cristina Vassalle, Cristina Del Seppia, Giorgio Iervasi
- Endocrinol Metab. 2021;36(5):952-964. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1198
- 6,834 View
- 265 Download
- 37 Web of Science
- 44 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
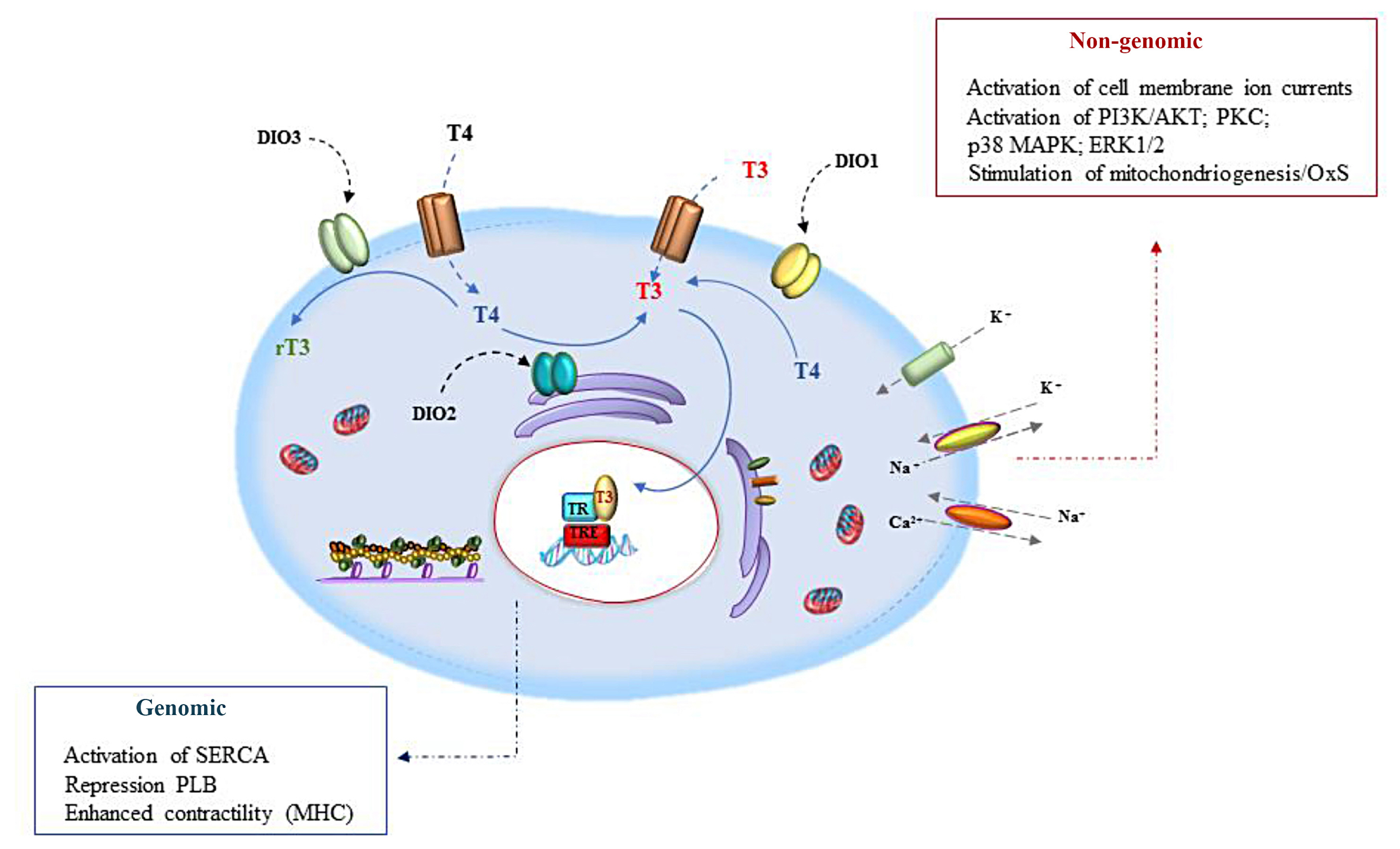
ePub - Thyroid hormone (TH) signaling is strictly regulated by iodothyronine deiodinase activity, which both preserves the circulating levels of the biologically active triiodothyronine (T3) and regulates TH homeostasis at the local level, in a cell- and time-dependent manner. Three deiodinases have been identified—namely iodothyronine deiodinase 1 (DIO1), DIO2, and DIO3—that differ in their catalytic properties and tissue distribution. The deiodinases represent a dynamic system that changes in the different stages of life according to their functions and roles in various cell types and tissues. Deiodinase activity at the tissue level permits cell-targeted fine regulation of TH homeostasis, mediating the activation (DIO1 and DIO2) and inactivation (DIO3) of THs. Deiodinase homeostasis is the driving force that leads T3-target cells towards customized TH signaling, which takes into account both the hormonal circulating levels and the tissue-specific response. This review analyzes the complex role of deiodinases in physiological and pathological contexts, exploring new challenges and opportunities deriving from a deeper knowledge of the dynamics underlying their roles and functions.
-
Citations
Citations to this article as recorded by- Noncatalytic Reductive Deiodination of Thyroid Hormones. Electrochemistry and Quantum Chemical Calculations
Piotr P. Romańczyk, Stefan S. Kurek
ChemElectroChem.2024;[Epub] CrossRef - Comparison of in vitro thyroxine (T4) metabolism between Wistar rat and human hepatocyte cultures
Audrey Baze, Lucille Wiss, Liliia Horbal, Klaus Biemel, Laure Asselin, Lysiane Richert
Toxicology in Vitro.2024; 96: 105763. CrossRef - Thyroxine Levels Predict the Development of Brain Failure in Patients With Cirrhosis in Indian Population
Anand V. Kulkarni, Moiz Vora, Ramyasri Ramagundam, Mithun Sharma, D. Nageshwar Reddy, P.N. Rao, S. Iyengar, D. Gujjarlapudi, A. Gupta, M. Alla, S. Venishetty, R. Gupta
Gastro Hep Advances.2024; 3(1): 55. CrossRef - Embryonic thermal manipulation reduces hatch time, increases hatchability, thermotolerance, and liver metabolism in broiler embryos
Sadid Al Amaz, Md Ahosanul Haque Shahid, Ajay Chaudhary, Rajesh Jha, Birendra Mishra
Poultry Science.2024; 103(4): 103527. CrossRef - Factors and Mechanisms of Thyroid Hormone Activity in the Brain: Possible Role in Recovery and Protection
Laura Sabatino, Dominga Lapi, Cristina Del Seppia
Biomolecules.2024; 14(2): 198. CrossRef - Association between per- and polyfluoroalkyl substances exposure and thyroid function biomarkers among females attending a fertility clinic
Yu Zhang, Vicente Mustieles, T.I.M. Korevaar, Leah Martin, Yang Sun, Zainab Bibi, Nicole Torres, Ayanna Coburn-Sanderson, Olivia First, Irene Souter, John C. Petrozza, Maarten A.C. Broeren, Julianne C. Botelho, Antonia M. Calafat, Yi-Xin Wang, Carmen Mess
Environmental Pollution.2024; 346: 123513. CrossRef - Correlation between a low serum free triiodothyronine level and mortality of severe pulmonary tuberculosis patients
Yan Yang, Xiaoqing Huang
BMC Infectious Diseases.2024;[Epub] CrossRef - Investigating open access new approach methods (NAM) to assess biological points of departure: A case study with 4 neurotoxic pesticides
Marilyn H. Silva
Current Research in Toxicology.2024; 6: 100156. CrossRef - A regulatory element associated to NAFLD in the promoter of DIO1 controls LDL-C, HDL-C and triglycerides in hepatic cells
Casimiro Castillejo-López, José Ramón Bárcenas-Walls, Marco Cavalli, Anders Larsson, Claes Wadelius
Lipids in Health and Disease.2024;[Epub] CrossRef - Thyroid dysfunction and Alzheimer's disease, a vicious circle
Zhaoqing Li, Jia Liu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Male-transmitted transgenerational effects of the herbicide linuron on DNA methylation profiles in Xenopus tropicalis brain and testis
Mauricio Roza, Andreas N.M. Eriksson, Sofie Svanholm, Cecilia Berg, Oskar Karlsson
Science of The Total Environment.2024; 923: 170949. CrossRef - Selenoprotein Gene mRNA Expression Evaluation During Renal Ischemia–Reperfusion Injury in Rats and Ebselen Intervention Effects
Yikun Wu, Hua Shi, Yuangao Xu, Rao Wen, Maodi Gong, Guangyi Hong, Shuxiong Xu
Biological Trace Element Research.2023; 201(4): 1792. CrossRef - Acute exposure to microcystins affects hypothalamic-pituitary axes of male rats
Ting Shi, Lin-Lin Xu, Liang Chen, Jun He, Ye-Ke Wang, Feng Chen, Yang Chen, John P. Giesy, Yu-Ting Wang, Qian-Hui Wu, Wen-Li Xu, Jun Chen, Ping Xie
Environmental Pollution.2023; 318: 120843. CrossRef - Thyroid hormone Beta receptor agonists for treatment of kidney disease: A promising agent?
Sidar Copur, Furkan Yavuz, Mehmet Kanbay
European Journal of Clinical Investigation.2023;[Epub] CrossRef - The ratio of free triiodothyronine to free thyroxine is regulated differently in patients with type 2 diabetes mellitus treated and not treated with sodium glucose cotransporter 2 inhibitors
Shuichi Okada, Atsushi Isoda, Hiroto Hoshi, Junichi Okada, Kazuya Okada, Eijiro Yamada, Tsugumichi Saito, Takuya Watanabe, Koji Kikkawa, Kihachi Ohshima
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102704. CrossRef - WITHDRAWN: The effect of deiodinase type-3 gene on the therapeutic response to levothyroxine in a sample of Iraqi hypothyroidism patients
Alaa Hashim Mohmmed, Suzanne Jubair, Ban Hoshi
Human Gene.2023; : 201142. CrossRef - Subclinical hypothyroidism, outcomes and management guidelines: a narrative review and update of recent literature
Bogumila Urgatz, Salman Razvi
Current Medical Research and Opinion.2023; 39(3): 351. CrossRef - DIO1 Gene Polymorphism Is Associated with Thyroid Profiles and Reproductive Performance in Dairy Cows
Olga V. Kostyunina, Olga S. Mityashova, Nikolay V. Bardukov, Olga V. Aleynikova, Irina Y. Lebedeva
Agriculture.2023; 13(2): 398. CrossRef - Embryonic thermal manipulation leads growth inhibition and reduced hepatic insulin-like growth factor1 expression due to promoter DNA hypermethylation in broilers
Wei Cong, Wanwan Han, Jie Liu, Ruqian Zhao, Lei Wu
Poultry Science.2023; 102(4): 102562. CrossRef - Drug Repurposing Patent Applications October–December 2022
Hermann A.M. Mucke
ASSAY and Drug Development Technologies.2023; 21(2): 80. CrossRef - Insights on the Association between Thyroid Diseases and Colorectal Cancer
Federica Gagliardi, Enke Baldini, Eleonora Lori, Silvia Cardarelli, Daniele Pironi, Augusto Lauro, Domenico Tripodi, Piergaspare Palumbo, Eleonora D’Armiento, Giuseppe Cavallaro, Andrea Polistena, Valerio D’Orazi, Simone Sibio, Poupak Fallahi, Alessandro
Journal of Clinical Medicine.2023; 12(6): 2234. CrossRef - Combining In Vitro and In Silico New Approach Methods to Investigate Type 3 Iodothyronine Deiodinase Chemical Inhibition Across Species
Sally A. Mayasich, Michael R. Goldsmith, Kali Z. Mattingly, Carlie A. LaLone
Environmental Toxicology and Chemistry.2023; 42(5): 1032. CrossRef - Thyrotoxic Cardiomyopathy: State of the Art
Juan Eduardo Quiroz-Aldave, María del Carmen Durand-Vásquez, Carlos Jhonatan Lobato-Jeri, Juan-Manuel Muñoz-Moreno, Diana Carolina Deutz Gómez Condori, Sofía Pilar Ildefonso-Najarro, Felipe Contreras-Yametti, Francisca Zavaleta-Gutiérrez, Luis Concepción-
European Endocrinology.2023; 19(1): 78. CrossRef - Bisphenol A-Induced Endocrine Dysfunction and its Associated Metabolic Disorders
Meenu Maniradhan, Latchoumycandane Calivarathan
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(4): 515. CrossRef - Dose- and Time-Dependent Effects of Radiofrequency Electromagnetic Field on Adipose Tissue: Implications of Thermoregulation and Mitochondrial Signaling
Jennifer Maalouf, Amandine Pelletier, Aurélie Corona, Jérôme Gay-Quéheillard, Véronique Bach, René de Seze, Brahim Selmaoui
International Journal of Molecular Sciences.2023; 24(13): 10628. CrossRef - Critically ill patients: Histopathological evidence of thyroid dysfunction
Dipti Saha, Saurabh Chattopadhyay, Sayak Sovan Dutta, Anup Kumar Roy
Journal of Critical Care.2023; 78: 154384. CrossRef - Primary Hypothyroidism and Alzheimer’s Disease: A Tale of Two
Faisal Holil AlAnazi, Hayder M. Al-kuraishy, Athanasios Alexiou, Marios Papadakis, Mohamed H. Mazhar Ashour, Saud A. Alnaaim, Omnya Elhussieny, Hebatallah M. Saad, Gaber El-Saber Batiha
Cellular and Molecular Neurobiology.2023; 43(7): 3405. CrossRef - Genetically predicted thyroid function and risk of colorectal cancer: a bidirectional Mendelian randomization study
Qiang Du, Zhaoyang Zheng, Yong Wang, Lie Yang, Zongguang Zhou
Journal of Cancer Research and Clinical Oncology.2023; 149(15): 14015. CrossRef - SARS-CoV-2 infection and thyroid dysfunction in children
K. V. Kozak, H. A. Pavlyshyn, I. Y. Avramenko, O. M. Dyvonyak, O. O. Shevchuk, K. T. Hlushko
The Ukrainian Biochemical Journal.2023; 95(3): 12. CrossRef - Nongenomic roles of thyroid hormones and their derivatives in adult brain: are these compounds putative neurotransmitters?
Joseph V. Martin, Pradip K. Sarkar
Frontiers in Endocrinology.2023;[Epub] CrossRef - Drug Repurposing Patent Applications April–June 2023
Hermann A.M. Mucke
ASSAY and Drug Development Technologies.2023; 21(6): 288. CrossRef - Deiodinase Types 1 and 3 and Proinflammatory Cytokine Values May Discriminate Depressive Disorder Patients from Healthy Controls
Elżbieta Małujło-Balcerska, Tadeusz Pietras
Journal of Clinical Medicine.2023; 12(19): 6163. CrossRef - Thyroid Dysfunction Induced by Fungicide Famoxadone Exposure Contributes to Nonalcoholic Fatty Liver Disease in Male Mice: In Vivo, In Vitro, and In Silico Studies
Shouchun Xiao, Jingna Cui, Aisong Chen, Haonan Hou, Jianing Yao, Yue Cao, Yaofeng Fang, Xueke Liu, Zhiqiang Zhou, Donghui Liu, Peng Wang
Environmental Science & Technology.2023; 57(40): 14881. CrossRef -
In-silico
studies of
Brassica oleracea
active compounds and their role in thyroid peroxidase activity
Haritha Kalath, Abel John Koshy, Bhavya Banjan, Sowmya Soman, Gururaja Hosadevasthana, Rajesh Raju, Niyas Rehman, Amjesh Revikumar
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Advances and Perspectives of Selenocompounds as Dietary Supplements to Ameliorate Obesity Biomarkers: From Field to Market
Frineth de la Luz Limón Aguilera, Sayra N. Serrano Sandoval, Mauricio Graciano-Palacios, Janet A. Gutiérrez-Uribe, Anayansi Escalante-Aburto
Food Reviews International.2023; : 1. CrossRef - Understanding the Roles of Selenium on Thyroid Hormone-Induced Thermogenesis in Adipose Tissue
Yasmin Anissa R. Ruswandi, Ronny Lesmana, Aziiz Mardanarian Rosdianto, Julia Windi Gunadi, Hanna Goenawan, Felix Zulhendri
Biological Trace Element Research.2023;[Epub] CrossRef - Deiodinase Type 3 Polymorphism (rs1190716) Affects Therapeutic Response to Levothyroxine
Alaa Hashim MOHMMED, Ban HOSHI, Suzanne JUBAIR
Turkish Journal of Pharmaceutical Sciences.2023; 20(5): 335. CrossRef - Polycystic Ovary Syndrome and Oxidative Stress—From Bench to Bedside
Natalia Zeber-Lubecka, Michał Ciebiera, Ewa E. Hennig
International Journal of Molecular Sciences.2023; 24(18): 14126. CrossRef - Thyroid hormone action and liver disease, a complex interplay
Luigi Marino, Adam Kim, Bin Ni, Francesco S. Celi
Hepatology.2023;[Epub] CrossRef - Arsenic-Induced Thyroid Hormonal Alterations and Their Putative Influence on Ovarian Follicles in Balb/c Mice
Nandheeswari K, Jayapradha P, Sree Vaishnavi Nalla, Itishree Dubey, Sapana Kushwaha
Biological Trace Element Research.2023;[Epub] CrossRef - Thyroid Dysfunction and COVID-19: The Emerging Role of Selenium in This Intermingled Relationship
Francesca Gorini, Laura Sabatino, Alessio Coi, Giorgio Iervasi, Cristina Vassalle
International Journal of Environmental Research and Public Health.2022; 19(11): 6912. CrossRef - Associations of bisphenol exposure with thyroid hormones in pregnant women: a prospective birth cohort study in China
Huishen Huang, Jun Liang, Peng Tang, Chuanxiang Yu, Haoran Fan, Qian Liao, Jinghua Long, Dongxiang Pan, Xiaoyun Zeng, Shun Liu, Dongping Huang, Xiaoqiang Qiu
Environmental Science and Pollution Research.2022; 29(58): 87170. CrossRef - Selenium in Bodily Homeostasis: Hypothalamus, Hormones, and Highways of Communication
Pamela Toh, Jessica L. Nicholson, Alyssa M. Vetter, Marla J. Berry, Daniel J. Torres
International Journal of Molecular Sciences.2022; 23(23): 15445. CrossRef - Does clinical hypothyroidism occur in obesity? here is what the lab rats may be telling us about hope on the horizon
Orien L Tulp, Frantz Sainvil, Andrew Scrianka, Rolando Branly, Aftab R Awan, George P Einstein
International Journal of Family & Community Medicine.2022; 6(6): 338. CrossRef
- Noncatalytic Reductive Deiodination of Thyroid Hormones. Electrochemistry and Quantum Chemical Calculations

- Adrenal Gland
- Adrenal Venous Sampling for Subtype Diagnosis of Primary Hyperaldosteronism
- Mitsuhide Naruse, Akiyo Tanabe, Koichi Yamamoto, Hiromi Rakugi, Mitsuhiro Kometani, Takashi Yoneda, Hiroki Kobayashi, Masanori Abe, Youichi Ohno, Nobuya Inagaki, Shoichiro Izawa, Masakatsu Sone
- Endocrinol Metab. 2021;36(5):965-973. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1192
- 5,002 View
- 226 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
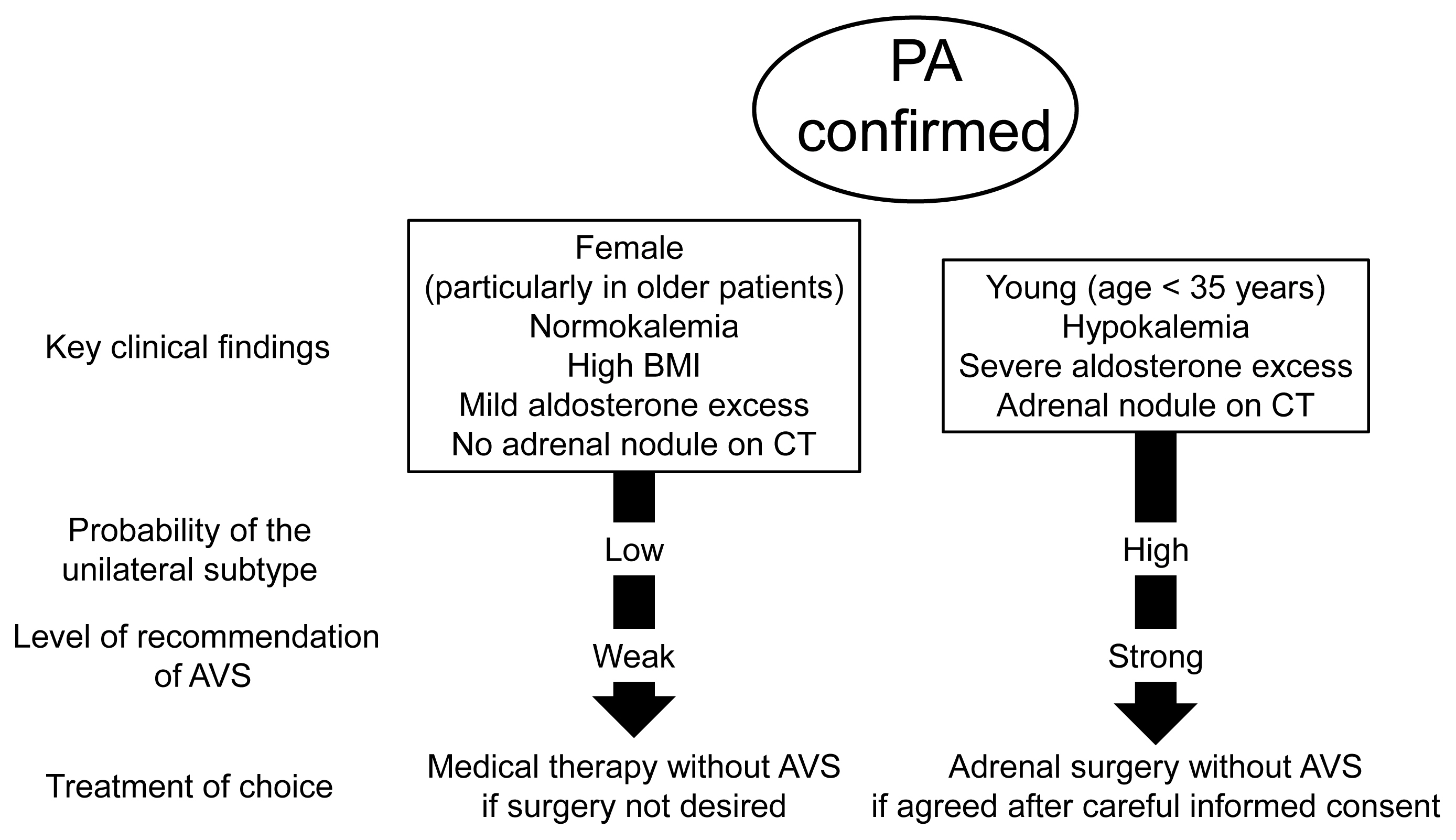
ePub - Adrenal venous sampling (AVS) is the key procedure for lateralization of primary hyperaldosteronism (PA) before surgery. Identification of the adrenal veins using computed tomography (CT) and intraoperative cortisol assay facilitates the success of catheterization. Although administration of adrenocorticotropic hormone (ACTH) has benefits such as improving the success rate, some unilateral cases could be falsely diagnosed as bilateral. Selectivity index of 5 with ACTH stimulation to assess the selectivity of catheterization and lateralization index (LI) >4 with ACTH stimulation for unilateral diagnosis is used in many centers. Co-secretion of cortisol from the tumor potentially affects the lateralization by the LI. Patients aged <35 years with hypokalemia, marked aldosterone excess, and unilateral adrenal nodule on CT have a higher probability of unilateral disease. Patients with normokalemia, mild aldosterone excess, and no adrenal tumor on CT have a higher probability of bilateral disease. Although no methods have 100% specificity for subtype diagnosis that would allow bypassing AVS, prediction of the subtype should be considered when recommending AVS to patients. Methodological standardization and strict indication improve diagnostic quality of AVS. Development of non-invasive imaging and biochemical markers will drive a paradigm shift in the clinical practice of PA.
-
Citations
Citations to this article as recorded by- A controlled trial of percutaneous adrenal arterial embolization for hypertension in patients with idiopathic hyperaldosteronism
Yaqiong Zhou, Xinquan Wang, Jixin Hou, Jindong Wan, Yi Yang, Sen Liu, Tao Luo, Qiting Liu, Qiang Xue, Peijian Wang
Hypertension Research.2024; 47(2): 311. CrossRef - Screening and diagnosis of primary aldosteronism. Consensus document of all the Spanish Societies involved in the management of primary aldosteronism
Marta Araujo-Castro, Jorge Gabriel Ruiz-Sánchez, Paola Parra Ramírez, Patricia Martín Rojas-Marcos, Almudena Aguilera-Saborido, Jorge Francisco Gómez Cerezo, Nieves López Lazareno, María Eugenia Torregrosa Quesada, Jorge Gorrin Ramos, Josep Oriola, Esteba
Endocrine.2024;[Epub] CrossRef - Diagnostic accuracy of using multiple cytokines to predict aldosterone-producing adenoma
Fei Qin, Hong Wen, Xiaoge Zhong, Yajin Pan, Xiaomei Lai, Tingting Yang, Jing Huang, Jie Yu, Jianling Li
Scientific Reports.2023;[Epub] CrossRef - A clinical assessment of portable point-of-care testing for quick cortisol assay during adrenal vein sampling
Ko Aiga, Mitsuhiro Kometani, Shigehiro Karashima, Seigo Konishi, Takuya Higashitani, Daisuke Aono, Xurong Mai, Mikiya Usukura, Takahiro Asano, Ayako Wakayama, Yuko Noda, Wataru Koda, Tetsuya Minami, Satoshi Kobayashi, Toshinori Murayama, Takashi Yoneda
Scientific Reports.2023;[Epub] CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef - Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes
Chang Ho Ahn, You-Bin Lee, Jae Hyeon Kim, Young Lyun Oh, Jung Hee Kim, Kyeong Cheon Jung
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef - The Entity of Connshing Syndrome: Primary Aldosteronism with Autonomous Cortisol Secretion
Mara Carsote
Diagnostics.2022; 12(11): 2772. CrossRef
- A controlled trial of percutaneous adrenal arterial embolization for hypertension in patients with idiopathic hyperaldosteronism

Editorial
- Thyroid
- Comparison of Thyroid Imaging Reporting and Data Systems in Malignancy Risk Stratification of Indeterminate Thyroid Nodules
- Bo Hyun Kim
- Endocrinol Metab. 2021;36(5):974-976. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1287
- 2,788 View
- 102 Download

Original Articles
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2021;36(5):977-987. Published online October 14, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1046
- 3,998 View
- 175 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
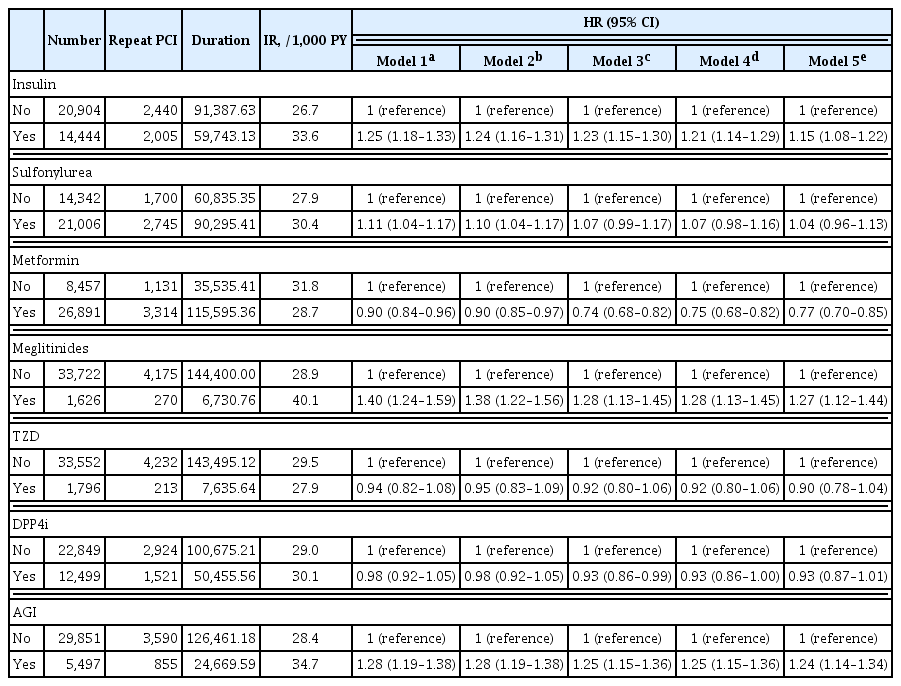
ePub - Background
Patients with diabetes have a higher risk of requiring repeated percutaneous coronary intervention (PCI) than non-diabetic patients. We aimed to evaluate and compare the effects of anti-diabetic drugs on the secondary prevention of myocardial infarction among type 2 diabetes mellitus patients.
Methods
We analyzed the general health check-up dataset and claims data of the Korean National Health Insurance Service of 199,714 participants (age ≥30 years) who underwent PCIs between 2010 and 2013. Those who underwent additional PCI within 1 year of their first PCI (n=3,325) and those who died within 1 year (n=1,312) were excluded. Patients were classified according to their prescription records for glucose-lowering agents. The primary endpoint was the incidence rate of coronary revascularization.
Results
A total of 35,348 patients were included in the study. Metformin significantly decreased the risk of requiring repeat PCI in all patients (adjusted hazard ratio [aHR], 0.77). In obese patients with body mass index (BMI) ≥25 kg/m2, patients treated with thiazolidinedione (TZD) exhibited a decreased risk of requiring repeat revascularization than those who were not treated with TZD (aHR, 0.77; 95% confidence interval, 0.63 to 0.95). Patients treated with metformin showed a decreased risk of requiring revascularization regardless of their BMI. Insulin, meglitinide, and alpha-glucosidase inhibitor were associated with increased risk of repeated PCI.
Conclusion
The risk of requiring repeat revascularization was lower in diabetic patients treated with metformin and in obese patients treated with TZD. These results suggest that physicians should choose appropriate glucose-lowering agents for the secondary prevention of coronary artery disease. -
Citations
Citations to this article as recorded by- Application of systemic inflammation indices and lipid metabolism-related factors in coronary artery disease
Zhuoyan Zhao, Huan Lian, Yixiang Liu, Lixian Sun, Ying Zhang
Coronary Artery Disease.2023; 34(5): 306. CrossRef - Effect of metformin on adverse outcomes in T2DM patients: Systemic review and meta-analysis of observational studies
Zhicheng Xu, Haidong Zhang, Chenghui Wu, Yuxiang Zheng, Jingzhou Jiang
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Establishment of a Predictive Model for Poor Prognosis of Incomplete Revascularization in Patients with Coronary Heart Disease and Multivessel Disease
Huan Lian, Zhuoyan Zhao, Kelin Ma, Zhenjiang Ding, Lixian Sun, Ying Zhang
Clinical and Applied Thrombosis/Hemostasis.2022; 28: 107602962211392. CrossRef
- Application of systemic inflammation indices and lipid metabolism-related factors in coronary artery disease

- Diabetes, Obesity and Metabolism
- How Can We Adopt the Glucose Tolerance Test to Facilitate Predicting Pregnancy Outcome in Gestational Diabetes Mellitus?
- Kyeong Jin Kim, Nam Hoon Kim, Jimi Choi, Sin Gon Kim, Kyung Ju Lee
- Endocrinol Metab. 2021;36(5):988-996. Published online October 15, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1107

- 4,159 View
- 112 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated how 100-g oral glucose tolerance test (OGTT) results can be used to predict adverse pregnancy outcomes in gestational diabetes mellitus (GDM) patients.
Methods
We analyzed 1,059 pregnant women who completed the 100-g OGTT between 24 and 28 weeks of gestation. We compared the risk of adverse pregnancy outcomes according to OGTT patterns by latent profile analysis (LPA), numbers to meet the OGTT criteria, and area under the curve (AUC) of the OGTT graph. Adverse pregnancy outcomes were defined as a composite of preterm birth, macrosomia, large for gestational age, low APGAR score at 1 minute, and pregnancy-induced hypertension.
Results
Overall, 257 participants were diagnosed with GDM, with a median age of 34 years. An LPA led to three different clusters of OGTT patterns; however, there were no significant associations between the clusters and adverse pregnancy outcomes after adjusting for confounders. Notwithstanding, the risk of adverse pregnancy outcome increased with an increase in number to meet the OGTT criteria (P for trend=0.011); odds ratios in a full adjustment model were 1.27 (95% confidence interval [CI], 0.72 to 2.23), 2.16 (95% CI, 1.21 to 3.85), and 2.32 (95% CI, 0.66 to 8.15) in those meeting the 2, 3, and 4 criteria, respectively. The AUCs of the OGTT curves also distinguished the patients at risk of adverse pregnancy outcomes; the larger the AUC, the higher the risk (P for trend=0.007).
Conclusion
The total number of abnormal values and calculated AUCs for the 100-g OGTT may facilitate tailored management of patients with GDM by predicting adverse pregnancy outcomes. -
Citations
Citations to this article as recorded by- Risk factors combine in a complex manner in assessment for macrosomia
Yi-Wen Wang, Yan Chen, Yong-Jun Zhang
BMC Public Health.2023;[Epub] CrossRef - Association of the Severity of Hypertensive Disorders in Pregnancy with Birthweight, Childhood Obesity, and Blood Pressure at Age 7
Yan Chen, Yiwen Wang, Yanjun Li, Guodong Ding, Yongjun Zhang
Nutrients.2023; 15(14): 3104. CrossRef
- Risk factors combine in a complex manner in assessment for macrosomia

- Diabetes, Obesity and Metabolism
- Role of TRPV4 Channel in Human White Adipocytes Metabolic Activity
- Julio C. Sánchez, Aníbal Valencia-Vásquez, Andrés M. García
- Endocrinol Metab. 2021;36(5):997-1006. Published online October 14, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1167
- 3,614 View
- 122 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
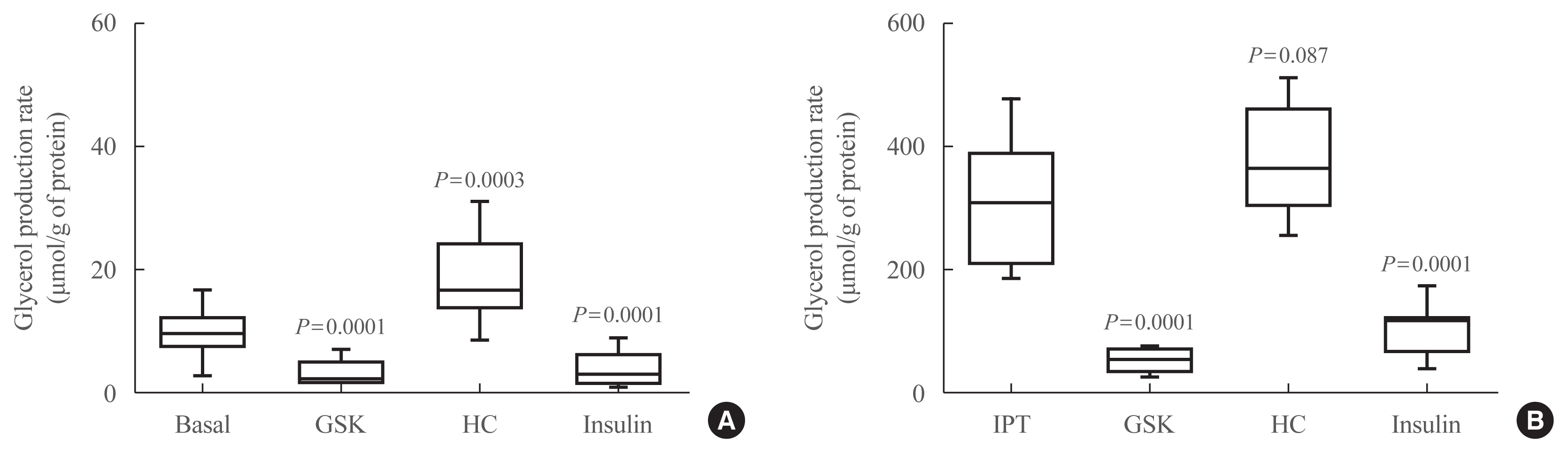
ePub - Background
Intracellular calcium (Ca2+) homeostasis plays an essential role in adipocyte metabolism and its alteration is associated with obesity and related disorders. Transient receptor potential vanilloid 4 (TRPV4) channels are an important Ca2+ pathway in adipocytes and their activity is regulated by metabolic mediators such as insulin. In this study, we evaluated the role of TRPV4 channels in metabolic activity and adipokine secretion in human white adipocytes.
Methods
Human white adipocytes were freshly cultured and the effects of the activation and inhibition of TRPV4 channels on lipolysis, glucose uptake, lactate production, and leptin and adiponectin secretion were evaluated.
Results
Under basal and isoproterenol-stimulated conditions, TRPV4 activation by GSK1016709A decreased lipolysis whereas HC067047, an antagonist, increased lipolysis. The activation of TRPV4 resulted in increased glucose uptake and lactate production under both basal conditions and insulin-stimulated conditions; in contrast HC067047 decreased both parameters. Leptin production was increased, and adiponectin production was diminished by TRPV4 activation and its inhibition had the opposite effect.
Conclusion
Our results suggested that TRPV4 channels are metabolic mediators involved in proadipogenic processes and glucose metabolism in adipocyte biology. TRPV4 channels could be a potential pharmacological target to treat metabolic disorders. -
Citations
Citations to this article as recorded by- Obesity, bone marrow adiposity, and leukemia: Time to act
Vijay Kumar, John H. Stewart
Obesity Reviews.2024;[Epub] CrossRef - TRP channels associated with macrophages as targets for the treatment of obese asthma
Wenzhao Zhu, Dinxi Bai, Wenting Ji, Jing Gao
Lipids in Health and Disease.2024;[Epub] CrossRef - Multidisciplinary Advances Address the Challenges in Developing Drugs against Transient Receptor Potential Channels to Treat Metabolic Disorders
Yibing Wang
ChemMedChem.2023;[Epub] CrossRef - Ion channels regulate energy homeostasis and the progression of metabolic disorders: Novel mechanisms and pharmacology of their modulators
Wenyi Wu, Jianan Zheng, Ru Wang, Yibing Wang
Biochemical Pharmacology.2023; 218: 115863. CrossRef - Potential lipolytic regulators derived from natural products as effective approaches to treat obesity
Xi-Ding Yang, Xing-Cheng Ge, Si-Yi Jiang, Yong-Yu Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Adipokines: Deciphering the cardiovascular signature of adipose tissue
Joseph C. Galley, Shubhnita Singh, Wanessa M.C. Awata, Juliano V. Alves, Thiago Bruder-Nascimento
Biochemical Pharmacology.2022; 206: 115324. CrossRef
- Obesity, bone marrow adiposity, and leukemia: Time to act

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Frequency of Exposure to Impaired Fasting Glucose and Risk of Mortality and Cardiovascular Outcomes
- Seung-Hwan Lee, Kyungdo Han, Hyuk-Sang Kwon, Mee Kyoung Kim
- Endocrinol Metab. 2021;36(5):1007-1015. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1218
- 3,810 View
- 126 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
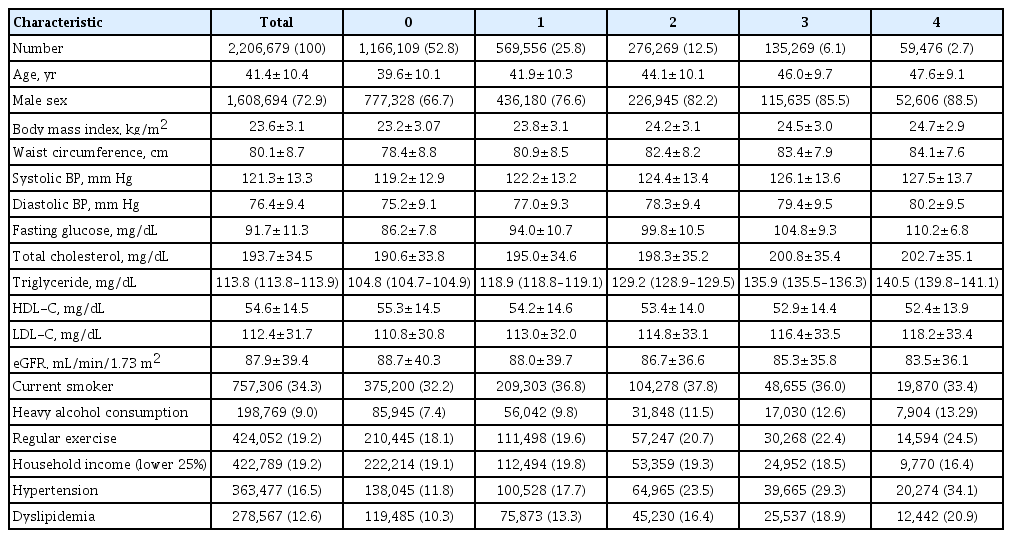
ePub - Background
Metabolic abnormalities, such as impaired fasting glucose (IFG), are dynamic phenomena; however, it is unclear whether the timing of IFG exposure and cumulative exposure to IFG are related to cardiovascular disease (CVD) and mortality risk.
Methods
Data were extracted from a nationwide population-based cohort in South Korea for adults (n=2,206,679) who were free of diabetes and had 4 years of consecutive health examination data. Fasting blood glucose levels of 100 to 125 mg/dL were defined as IFG, and the number of IFG diagnoses for each adult in the 4-year period was tabulated as the IFG exposure score (range, 0 to 4). Adults with persistent IFG for the 4-year period received a score of 4.
Results
The median follow-up was 8.2 years. There were 24,820 deaths, 13,502 cases of stroke, and 13,057 cases of myocardial infarction (MI). IFG exposure scores of 1, 2, 3, and 4 were associated with all-cause mortality (multivariable-adjusted hazard ratio [aHR], 1.11; 95% confidence interval [CI], 1.08 to 1.15; aHR, 1.16; 95% CI, 1.12 to 1.20; aHR, 1.20; 95% CI, 1.15 to 1.25; aHR, 1.18; 95% CI, 1.11 to 1.25, respectively) compared with an IFG exposure score of 0. Adjusting for hypertension and dyslipidemia attenuated the slightly increased risk of MI or stroke associated with high IFG exposure scores, but significant associations for allcause mortality remained.
Conclusion
The intensity of IFG exposure was associated with an elevated risk of all-cause mortality, independent of cardiovascular risk factors. The association between IFG exposure and CVD risk was largely mediated by the coexistence of dyslipidemia and hypertension. -
Citations
Citations to this article as recorded by- A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Construction and Validation of a Model for Predicting Impaired Fasting Glucose Based on More Than 4000 General Population
Cuicui Wang, Xu Zhang, Chenwei Li, Na Li, Xueni Jia, Hui Zhao
International Journal of General Medicine.2023; Volume 16: 1415. CrossRef - Factors Affecting High Body Weight Variability
Kyungdo Han, Mee Kyoung Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 163. CrossRef - Exposure to perfluoroalkyl and polyfluoroalkyl substances and risk of stroke in adults: a meta-analysis
Min Cheol Chang, Seung Min Chung, Sang Gyu Kwak
Reviews on Environmental Health.2023;[Epub] CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - A Longitudinal Retrospective Observational Study on Obesity Indicators and the Risk of Impaired Fasting Glucose in Pre- and Postmenopausal Women
Myung Ji Nam, Hyunjin Kim, Yeon Joo Choi, Kyung-Hwan Cho, Seon Mee Kim, Yong-Kyun Roh, Kyungdo Han, Jin-Hyung Jung, Yong-Gyu Park, Joo-Hyun Park, Do-Hoon Kim
Journal of Clinical Medicine.2022; 11(10): 2795. CrossRef - Current Trends of Big Data Research Using the Korean National Health Information Database
Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
Diabetes & Metabolism Journal.2022; 46(4): 552. CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef - Additive interaction of diabetes mellitus and chronic kidney disease in cancer patient mortality risk
Seohyun Kim, Gyuri Kim, Jae Hyeon Kim
Scientific Reports.2022;[Epub] CrossRef
- A nationwide cohort study on diabetes severity and risk of Parkinson disease

- Diabetes, Obesity and Metabolism
- Changes in Insulin Resistance Index and the Risk of Liver Fibrosis in Patients with Nonalcoholic Fatty Liver Disease without Diabetes: Kangbuk Samsung Health Study
- Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2021;36(5):1016-1028. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1110
- 4,129 View
- 128 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
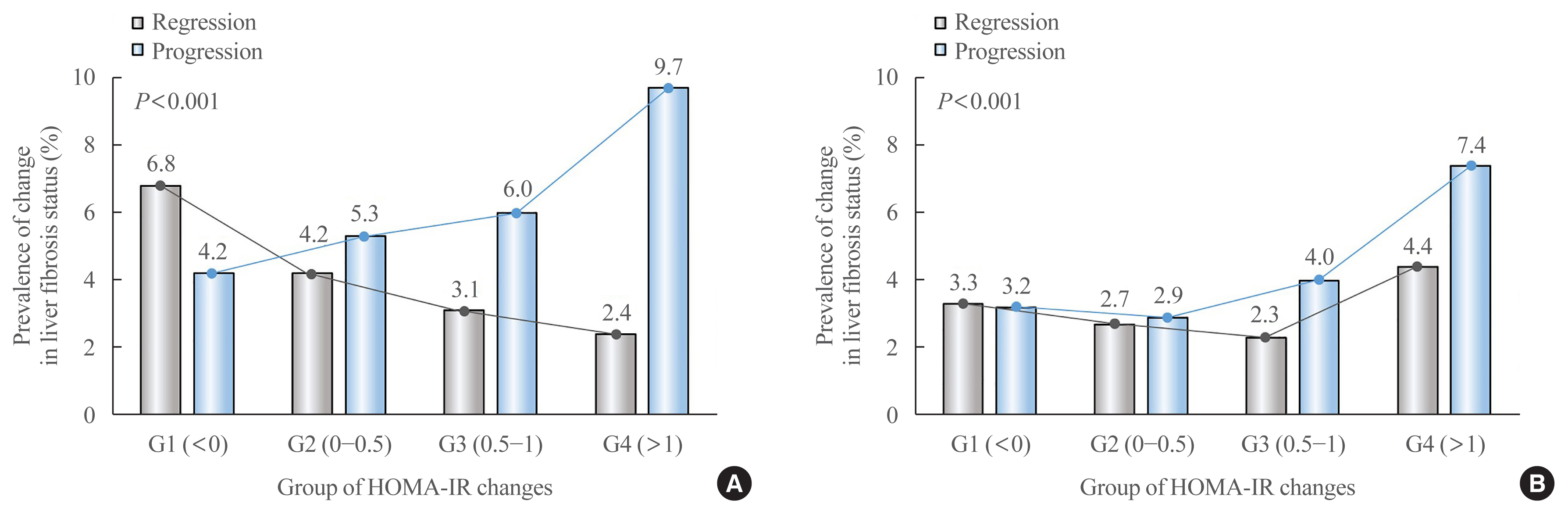
ePub - Background
Fibrosis is the most important prognostic factor for nonalcoholic fatty liver disease (NAFLD). Insulin resistance plays a key role of fibrosis progression. We evaluated the association between changes in homeostasis model assessment of insulin resistance (HOMA-IR) values and changes in fibrosis status in NAFLD.
Methods
We analyzed the data of 15,728 participants with NAFLD (86% men, mean age 40.5 years) who had no diabetes at baseline and visited our centers for health check-ups both in 2012 and 2016. The participants were classified into four groups according to the degree of change in HOMA-IR values from baseline to the end of follow-up: G1 (<0), G2 (0–0.50), G3 (0.51–1.00), and G4 (>1.00). NAFLD was assessed by ultrasonography, and fibrosis status was evaluated by the NAFLD fibrosis score (NFS) and the aspartate aminotransferase to platelet ratio index (APRI).
Results
After the 4-year follow-up, the multivariable-adjusted odds ratio (OR) for progression of fibrosis probability increased with increasing HOMA-IR values (OR, 2.25; 95% confidence interval [CI], 1.87 to 2.71 for NFS; and OR, 2.55; 95% CI, 2.05 to 3.18 for APRI, G4). This tendency remained consistent throughout the subgroup analyses, except in those for female sex and a body mass index <25 kg/m2. The OR for regression of fibrosis probability decreased with increasing HOMA-IR values (OR, 0.33; 95% CI, 0.25 to 0.43 for NFS, G4).
Conclusion
Changes in HOMA-IR values were associated with changes in fibrosis status in patients with NAFLD without diabetes, which underscores the role of insulin resistance in liver fibrosis. -
Citations
Citations to this article as recorded by- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis
Mohammad E. Khamseh, Mojtaba Malek, Soodeh Jahangiri, Sohrab Nobarani, Azita Hekmatdoost, Marieh Salavatizadeh, Samira Soltanieh, Haleh Chehrehgosha, Hoda Taheri, Zeinab Montazeri, Fereshteh Attaran, Faramarz Ismail-Beigi, Fariba Alaei-Shahmiri
Digestive Diseases and Sciences.2024; 69(4): 1430. CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - Factors Associated with Liver Fibrosis in Chinese Patients with Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease
Yu Luo, Cuiyu Wang, Tian Zhang, Xiaoyu He, Jianan Hao, Andong Shen, Hang Zhao, Shuchun Chen, Luping Ren
International Journal of General Medicine.2023; Volume 16: 293. CrossRef - Impact of COVID-19 Lockdown on Non-Alcoholic Fatty Liver Disease and Insulin Resistance in Adults: A before and after Pandemic Lockdown Longitudinal Study
Ángel Arturo López-González, Bárbara Altisench Jané, Luis Masmiquel Comas, Sebastiana Arroyo Bote, Hilda María González San Miguel, José Ignacio Ramírez Manent
Nutrients.2022; 14(14): 2795. CrossRef - Metabolic Score for Insulin Resistance Is Inversely Related to Incident Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease
Jun-Hyuk Lee, Yu-Jin Kwon, Kyongmin Park, Hye Sun Lee, Hoon-Ki Park, Jee Hye Han, Sang Bong Ahn
Nutrients.2022; 14(15): 3039. CrossRef - Machine learning models including insulin resistance indexes for predicting liver stiffness in United States population: Data from NHANES
Kexing Han, Kexuan Tan, Jiapei Shen, Yuting Gu, Zilong Wang, Jiayu He, Luyang Kang, Weijie Sun, Long Gao, Yufeng Gao
Frontiers in Public Health.2022;[Epub] CrossRef - The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
Dae-Jeong Koo, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(4): 132. CrossRef
- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Cardiovascular Outcomes of Obesity According to Menopausal Status: A Nationwide Population-Based Study
- Bo Kyung Koo, Sang-Hyun Park, Kyungdo Han, Min Kyong Moon
- Endocrinol Metab. 2021;36(5):1029-1041. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1197

- 3,662 View
- 117 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We estimated the effect of obesity on the incidence of cardiovascular disease (CVD) and mortality in women according to menopausal status.
Methods
Women aged 40 to 69 years under routine health check-ups provided by the National Health Insurance Service in 2009 were followed up till 2018 (n=2,208,559).
Results
In premenopausal women, a significant increment of mortality rate was found in underweight and obesity class II (hazard ratio [HR], 1.48; 95% confidence interval [CI], 1.31 to 1.67; and HR, 1.25; 95% CI, 1.12 to 1.39) compared to normal body mass index (BMI); overweight and obesity class I did not affect mortality rate. In postmenopausal women, obesity as well as overweight status reduced the risk of mortality compared to normal BMI (HR, 0.86; 95% CI, 0.83 to 0.88; and HR, 0.84; 95% CI, 0.82 to 0.86). By contrast, there was a linear association between CVD and BMI above the normal range irrespective of menopausal status, which was attenuated in diabetic women.
Conclusion
The current study replicated the J-shaped relationship between BMI and mortality, being more prominent in the postmenopausal group. The risk of CVD was linearly increased as BMI was increased above the normal range irrespective of menopausal status. -
Citations
Citations to this article as recorded by- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension
Geetha Kandasamy, Thangamani Subramani, Gigi Sam, Mona Almanasef, Tahani Almeleebia, Eman Shorog, Asma M. Alshahrani, Amjad Hmlan, Atheer Y. Al Suhaym, Kousalya Prabahar, Vinoth Prabhu Veeramani, Palanisamy Amirthalingam
Frontiers in Cardiovascular Medicine.2024;[Epub] CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 45. CrossRef - The effect of menopause on cardiovascular risk factors according to body mass index in middle-aged Korean women
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Aysha Almas
PLOS ONE.2023; 18(3): e0283393. CrossRef - Low‐quality muscle mass rather than normal‐quality muscle mass determines fibrosis progression in biopsy‐proven NAFLD
Yun Kyu Lee, Bo Kyung Koo, Sae Kyung Joo, Dong Hyeon Lee, Heejoon Jang, Jee Won Chai, Myoung Seok Lee, Si Won Jang, Young Ho So, Jeong Hwan Park, Mee Soo Chang, Won Kim
Alimentary Pharmacology & Therapeutics.2023; 58(3): 322. CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Non-pharmacologic treatment for obesity
Bo Kyung Koo
Journal of the Korean Medical Association.2022; 65(7): 400. CrossRef
- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension

- Diabetes, Obesity and Metabolism
- Prognostic Value of Triglyceride and Glucose Index for Incident Type 2 Diabetes beyond Metabolic Health and Obesity
- Hwi Seung Kim, Jiwoo Lee, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Hong-Kyu Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
- Endocrinol Metab. 2021;36(5):1042-1054. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1184
- 5,255 View
- 132 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
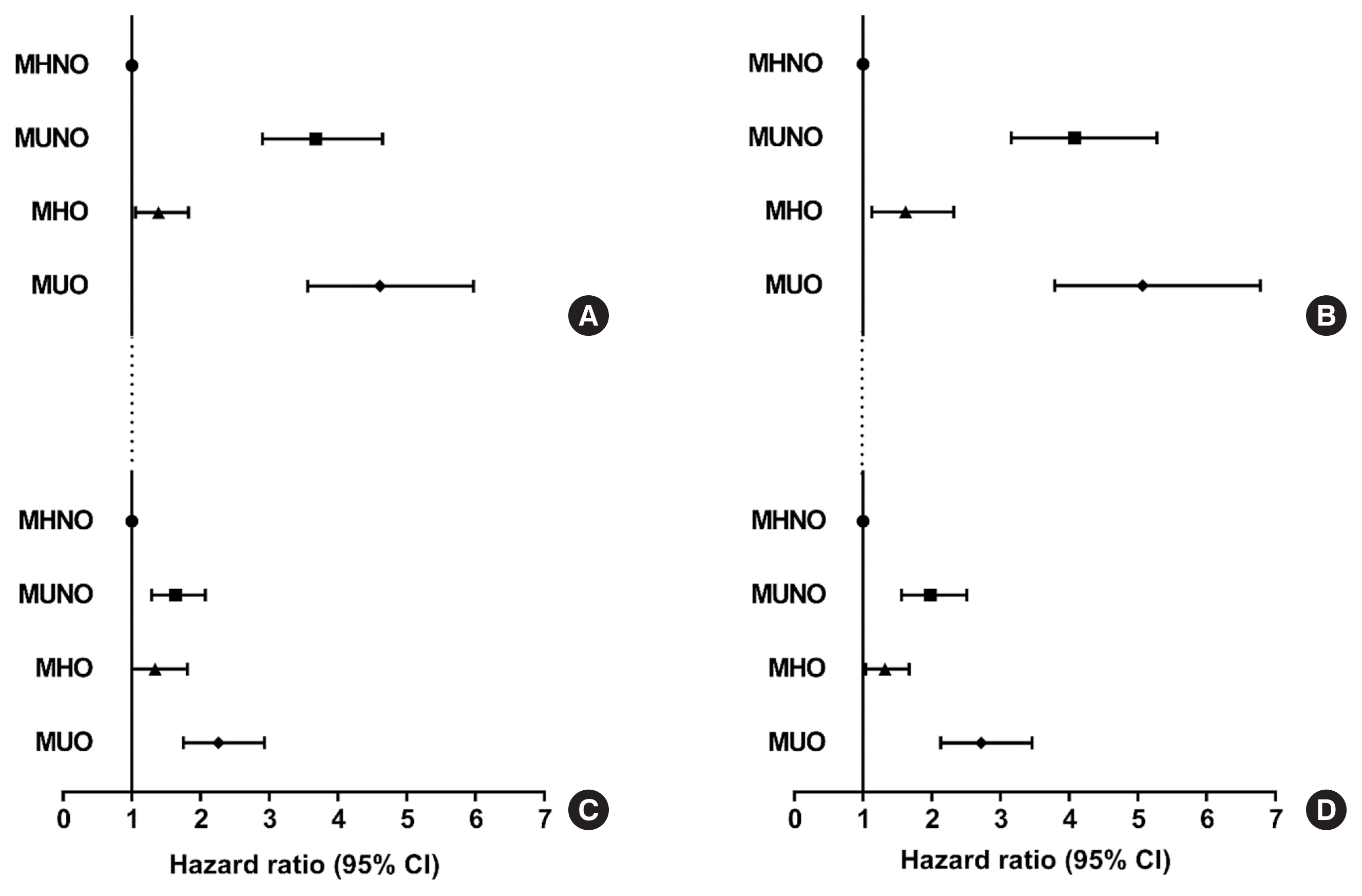
Metabolically healthy obese (MHO) phenotype is metabolically heterogeneous in terms of type 2 diabetes (T2D). Previously, the triglyceride and glucose (TyG) index has been considered for identifying metabolic health and future risk of T2D. This study aimed to evaluate the risk of incident T2D according to obesity status and metabolic health, categorized by four different criteria and the TyG index.
Methods
The study included 39,418 Koreans without T2D at baseline. The risk of T2D was evaluated based on four different definitions of metabolic health and obesity status and according to the baseline TyG index within each metabolic health and obesity group.
Results
During the median follow-up at 38.1 months, 726 individuals developed T2D. Compared with the metabolically healthy non-obese (MHNO) group with low TyG index, the MHO group with high TyG index showed increased risk of T2D in all four definitions of metabolic health with multivariate-adjusted hazard ratios of 2.57 (95% confidence interval [CI], 1.76 to 3.75), 3.72 (95% CI, 2.15 to 6.43), 4.13 (95% CI, 2.67 to 6.38), and 3.05 (95% CI, 2.24 to 4.15), when defined by Adult Treatment Panel III, Wildman, Karelis, and homeostasis model assessment (HOMA) criteria, respectively.
Conclusion
MHO subjects with high TyG index were at an increased risk of developing T2D compared with MHNO subjects, regardless of the definition of metabolic health. TyG index may serve as an additional factor for predicting the individual risk of incident T2D in MHO subjects.

- Diabetes, Obesity and Metabolism
- Musclin Is Related to Insulin Resistance and Body Composition, but Not to Body Mass Index or Cardiorespiratory Capacity in Adults
- Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis Valbuena, Andrés F. Milán, María C. Trillos-Almanza, Sergio Granados, Miguel Peña, Mauricio Estrada-Castrillón, Juan C. Aristizábal, Raúl Narvez-Sanchez, Jaime Gallo-Villegas, Juan C. Calderón
- Endocrinol Metab. 2021;36(5):1055-1068. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1104
- 5,037 View
- 137 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
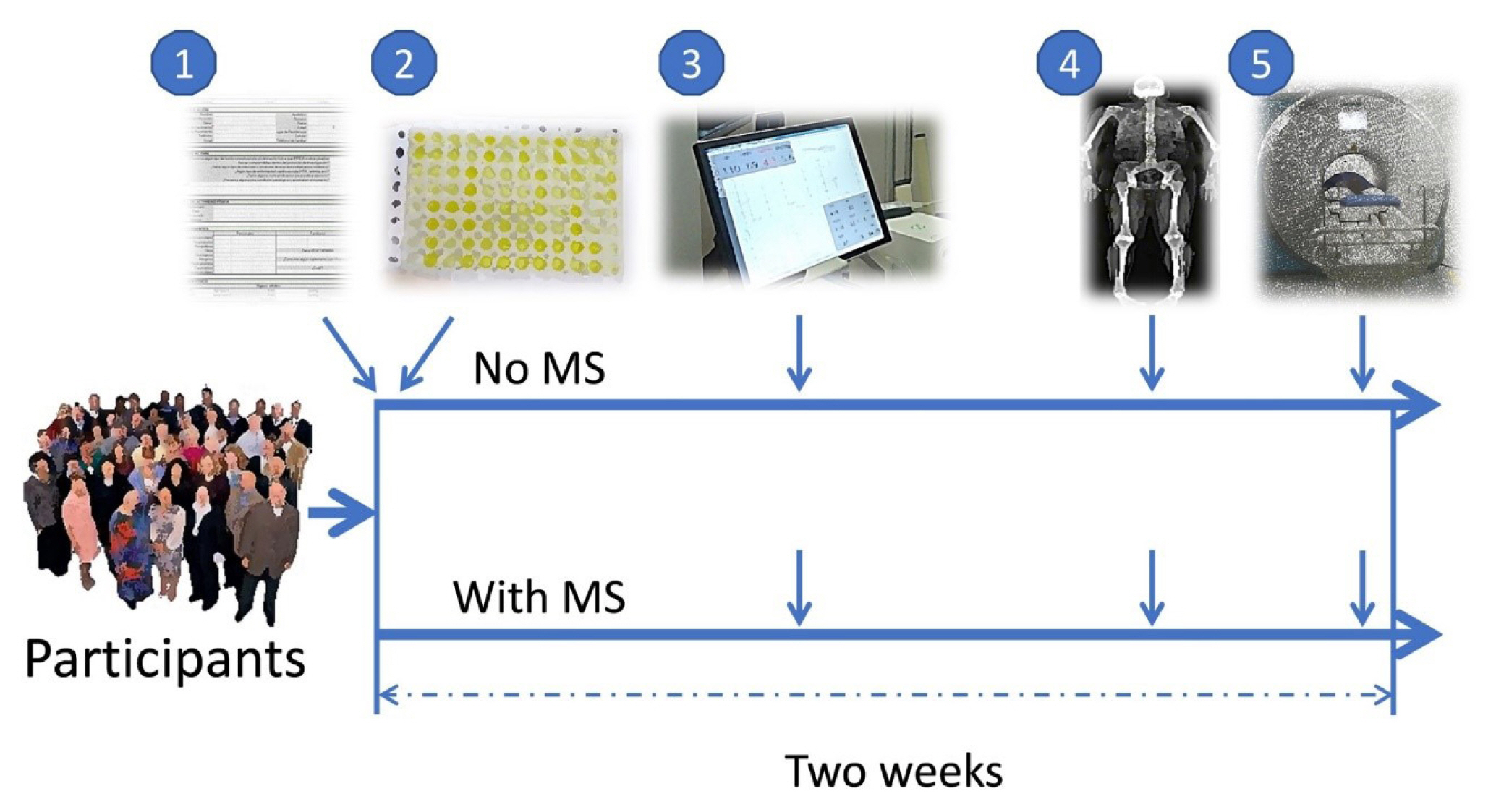
ePub - Background
We studied whether musclin function in humans is related to glycemic control, body composition, and cardiorespiratory capacity.
Methods
A cross-sectional study was performed in sedentary adults with or without metabolic syndrome (MS). Serum musclin was measured by enzyme-linked immunosorbent assay. Insulin resistance (IR) was evaluated by the homeostatic model assessment (HOMA-IR). Body composition was determined by dual-energy X-ray absorptiometry and muscle composition by measuring carnosine in the thigh, a surrogate of fiber types, through proton magnetic resonance spectroscopy. Cardiorespiratory capacity was assessed through direct ergospirometry.
Results
The control (n=29) and MS (n=61) groups were comparable in age (51.5±6.5 years old vs. 50.7±6.1 years old), sex (72.4% vs. 70.5% women), total lean mass (58.5%±7.4% vs. 57.3%±6.8%), and peak oxygen consumption (VOpeak) (31.0±5.8 mL O2./kg.min vs. 29.2±6.3 mL O2/kg.min). Individuals with MS had higher body mass index (BMI) (30.6±4.0 kg/m2 vs. 27.4± 3.6 kg/m2), HOMA-IR (3.5 [95% confidence interval, CI, 2.9 to 4.6] vs. 1.7 [95% CI, 1.1 to 2.0]), and musclin (206.7 pg/mL [95% CI, 122.7 to 387.8] vs. 111.1 pg/mL [95% CI, 63.2 to 218.5]) values than controls (P˂0.05). Musclin showed a significant relationship with HOMA-IR (β=0.23; 95% CI, 0.12 to 0.33; P˂0.01), but not with VOpeak, in multiple linear regression models adjusted for age, sex, fat mass, lean mass, and physical activity. Musclin was significantly associated with insulin, glycemia, visceral fat, and regional muscle mass, but not with BMI, VCO2peak, maximum heart rate, maximum time of work, or carnosine.
Conclusion
In humans, musclin positively correlates with insulinemia, IR, and a body composition profile with high visceral adiposity and lean mass, but low body fat percentage. Musclin is not related to BMI or cardiorespiratory capacity. -
Citations
Citations to this article as recorded by- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation
Wonjun Cho, Heeseung Oh, Sung Woo Choi, A. M. Abd El-Aty, Fatma Yeşilyurt, Ji Hoon Jeong, Tae Woo Jung
Inflammation.2024; 47(1): 1. CrossRef - Glucose restriction enhances oxidative fiber formation: A multi-omic signal network involving AMPK and CaMK2
Kaiyi Zhang, Ning Xie, Huaqiong Ye, Jiakun Miao, Boce Xia, Yu Yang, Huanqi Peng, Shuang Xu, Tianwen Wu, Cong Tao, Jinxue Ruan, Yanfang Wang, Shulin Yang
iScience.2024; 27(1): 108590. CrossRef - Myokines: metabolic regulation in obesity and type 2 diabetes
Zhi-Tian Chen, Zhi-Xuan Weng, Jiandie D Lin, Zhuo-Xian Meng
Life Metabolism.2024;[Epub] CrossRef - Epidemiological, mechanistic, and practical bases for assessment of cardiorespiratory fitness and muscle status in adults in healthcare settings
Jaime A. Gallo-Villegas, Juan C. Calderón
European Journal of Applied Physiology.2023; 123(5): 945. CrossRef - Serum Levels of Myonectin Are Lower in Adults with Metabolic Syndrome and Are Negatively Correlated with Android Fat Mass
Jorge L. Petro, María Carolina Fragozo-Ramos, Andrés F. Milán, Juan C. Aristizabal, Jaime A. Gallo-Villegas, Juan C. Calderón
International Journal of Molecular Sciences.2023; 24(8): 6874. CrossRef - The correlation of serum musclin with diabetic nephropathy
Jie Zhang, Jing Shi, Zengguang Cheng, Wenchao Hu
Cytokine.2023; 167: 156211. CrossRef - Efficacy of high-intensity interval- or continuous aerobic-training on insulin resistance and muscle function in adults with metabolic syndrome: a clinical trial
Jaime Gallo-Villegas, Leonardo A. Castro-Valencia, Laura Pérez, Daniel Restrepo, Oscar Guerrero, Sergio Cardona, Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis H. Valbuena, Miguel Peña, Andrés F. Milán, Maria C. Trillos-Almanza, Sergio Granados, Juan C.
European Journal of Applied Physiology.2022; 122(2): 331. CrossRef - Reactive Oxygen and Nitrogen Species (RONS) and Cytokines—Myokines Involved in Glucose Uptake and Insulin Resistance in Skeletal Muscle
Paola Llanos, Jesus Palomero
Cells.2022; 11(24): 4008. CrossRef
- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Subjects with Positive Fecal Immunochemical Test: A Nationwide Population-Based Study
- Kwang Woo Kim, Hyun Jung Lee, Kyungdo Han, Jung Min Moon, Seung Wook Hong, Eun Ae Kang, Jooyoung Lee, Hosim Soh, Seong-Joon Koh, Jong Pil Im, Joo Sung Kim
- Endocrinol Metab. 2021;36(5):1069-1077. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1119
- 3,611 View
- 97 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
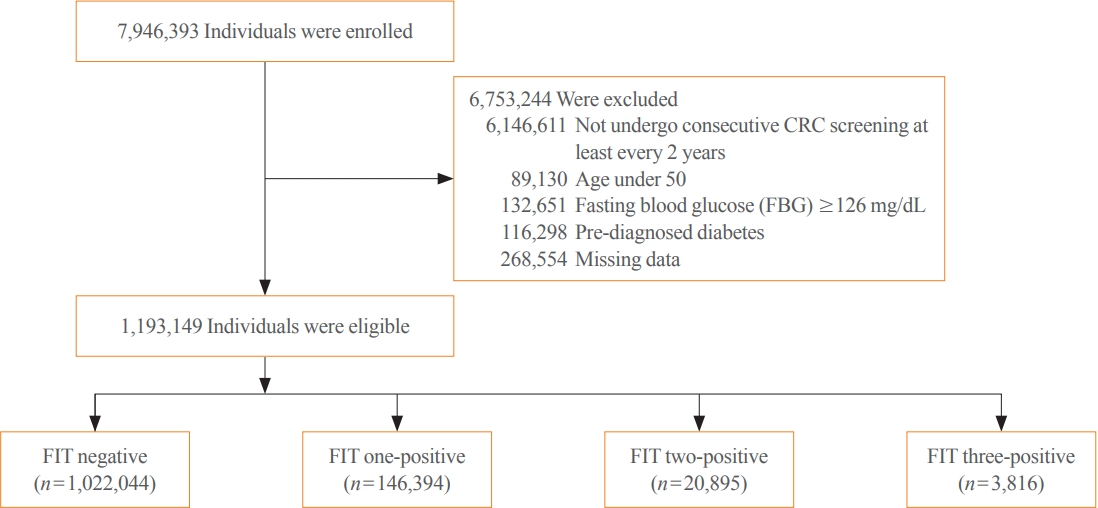
Positive fecal immunochemical test (FIT) results have been recently suggested as a risk factor for systemic inflammation. Diabetes induces inflammation in the gastrointestinal tract via several ways. We investigated the association between FIT results and the incidence of diabetes.
Methods
A total of 7,946,393 individuals aged ≥50 years from the National Cancer Screening Program database who underwent FIT for colorectal cancer (CRC) screening from 2009 to 2012 were enrolled. The primary outcome was newly diagnosed diabetes based on the International Classification of Disease 10th revision codes and administration of anti-diabetic medication during the follow-up period.
Results
During a mean follow-up of 6.5 years, the incidence rates of diabetes were 11.97, 13.60, 14.53, and 16.82 per 1,000 personyears in the FIT negative, one-positive, two-positive, and three-positive groups, respectively. The hazard ratios (HRs) for the incidence of diabetes were 1.14 (95% confidence interval [CI], 1.12 to 1.16; HR, 1.21; 95% CI, 1.16 to 1.27; and HR, 1.40; 95% CI, 1.28 to 1.55) in the one-positive, two-positive, and three-positive FIT groups compared with the FIT negative group, respectively. The effect was consistent in individuals with normal fasting blood glucose (adjusted HR 1.55 vs. 1.14, P for interaction <0.001).
Conclusion
Positive FIT results were associated with a significantly higher risk of diabetes, suggesting that the FIT can play a role not only as a CRC screening tool, but also as a surrogate marker of systemic inflammation; thus, increasing the diabetes risk. -
Citations
Citations to this article as recorded by- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality
Chi Pang Wen, Min Kuang Tsai, June Han Lee, Hung Yi Chiou, Christopher Wen, Ta-Wei David Chu, Chien Hua Chen
European Journal of Internal Medicine.2024; 120: 69. CrossRef - Faecal haemoglobin concentrations are associated with all-cause mortality and cause of death in colorectal cancer screening
Lasse Kaalby, Ulrik Deding, Issam Al-Najami, Gabriele Berg-Beckhoff, Thomas Bjørsum-Meyer, Tinne Laurberg, Aasma Shaukat, Robert J. C. Steele, Anastasios Koulaouzidis, Morten Rasmussen, Morten Kobaek-Larsen, Gunnar Baatrup
BMC Medicine.2023;[Epub] CrossRef - Positive Results from the Fecal Immunochemical Test Can Be Related to Dementia: A Nationwide Population-Based Study in South Korea
Yu Kyung Jun, Seung Woo Lee, Kwang Woo Kim, Jung Min Moon, Seong-Joon Koh, Hyun Jung Lee, Joo Sung Kim, Kyungdo Han, Jong Pil Im
Journal of Alzheimer's Disease.2023; 91(4): 1515. CrossRef - Faecal Haemoglobin Estimated by Faecal Immunochemical Tests—An Indicator of Systemic Inflammation with Real Clinical Potential
Karen N. Barnett, Gavin R. C. Clark, Robert J. C. Steele, Callum G. Fraser
Diagnostics.2021; 11(11): 2093. CrossRef
- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality


 KES
KES



 First
First Prev
Prev



