Search
- Page Path
- HOME > Search
- Miscellaneous
- Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
- Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
- Endocrinol Metab. 2023;38(6):750-759. Published online November 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1785
- 1,430 View
- 119 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the incidence of endocrine immune-related adverse events (irAEs) for recently developed immune checkpoint inhibitor (ICI) drugs.
Methods
We collected studies on newly developed ICI drugs using PubMed/Medline, Embase, and Cochrane Library from inception through January 31, 2023. Among ICI drugs, nivolumab, pembrolizumab, and ipilimumab were excluded from the new ICI drugs because many papers on endocrine-related side effects have already been published.
Results
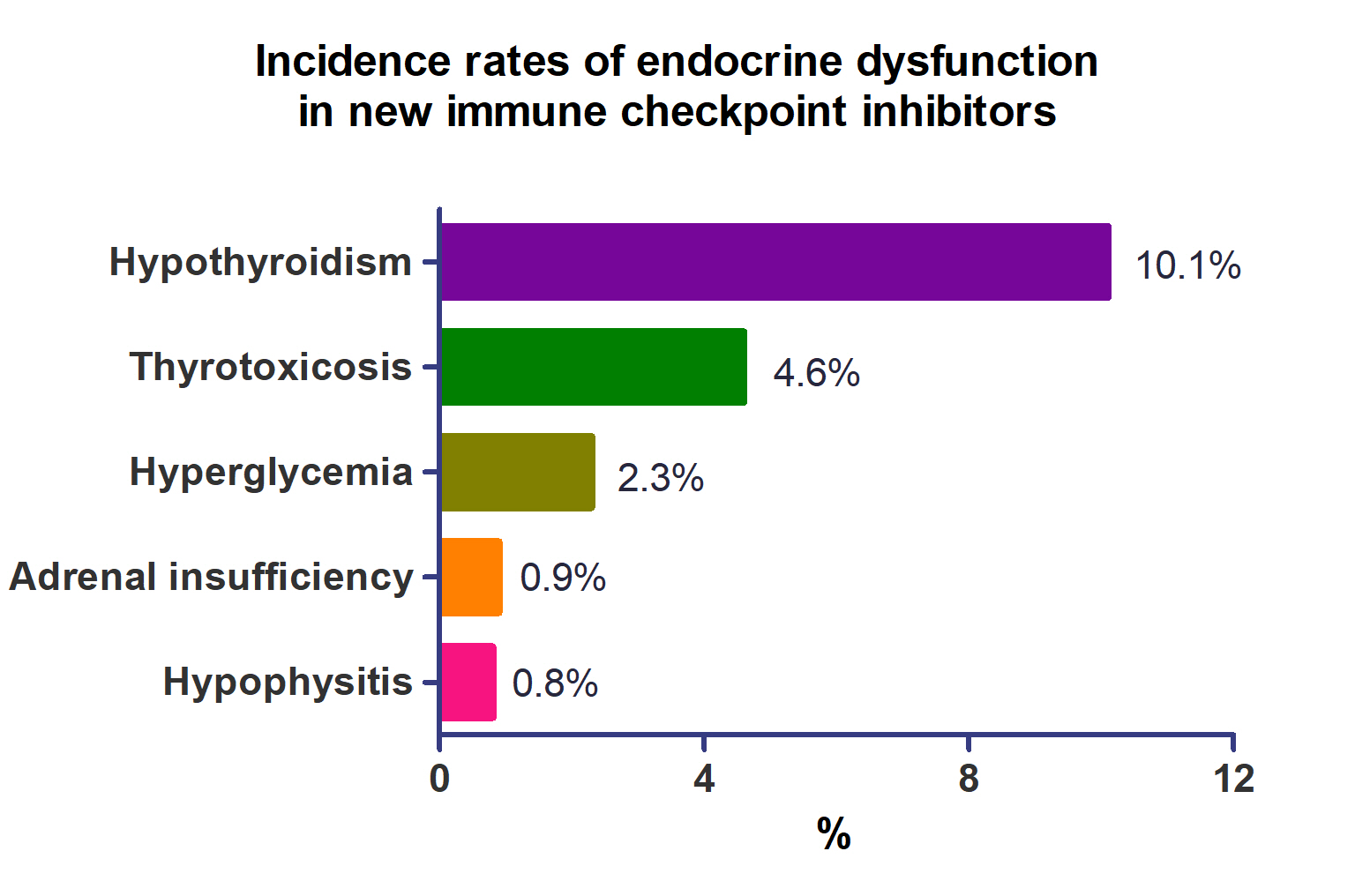
A total of 44,595 patients from 177 studies were included in this analysis. The incidence of hypothyroidism was 10.1% (95% confidence interval [CI], 8.9% to 11.4%), thyrotoxicosis was 4.6% (95% CI, 3.8% to 5.7%), hypophysitis was 0.8% (95% CI, 0.5% to 1.1%), adrenal insufficiency was 0.9% (95% CI, 0.7% to 1.1%), and hyperglycemia was 2.3% (95% CI, 1.6% to 3.4%). Hypothyroidism and thyrotoxicosis occurred most frequently with programmed cell death protein-1 (PD-1) inhibitors (13.7% and 7.5%, respectively). The rate of endocrine side effects for the combination of a programmed death-ligand 1 inhibitor (durvalumab) and cytotoxic T lymphocyte-associated antigen 4 inhibitor (tremelimumab) was higher than that of monotherapy. In a meta-analysis, the combination of tremelimumab and durvalumab had a 9- to 10-fold higher risk of pituitary and adrenal-related side effects than durvalumab alone.
Conclusion
Newly developed PD-1 inhibitors had a high incidence of thyroid-related irAEs, and combined treatment with durvalumab and tremelimumab increased the risk of pituitary- and adrenal-related irAEs. Based on these facts, it is necessary to predict the endocrine side effects corresponding to each ICI drug, diagnose and treat them appropriately, and try to reduce the morbidity and mortality of patients.

- Thyroid
- Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
- Jeongmin Lee, Gi Hyeon Seo, Keeho Song
- Endocrinol Metab. 2023;38(4):455-461. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1711
- 2,607 View
- 180 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The correlation between acute coronavirus disease 2019 (COVID-19) and subacute thyroiditis (SAT) has not been clearly investigated in “long COVID” patients. We aimed to investigate the incidence of SAT during convalescence and after the acute phase of COVID-19, comparing with that of the general population.
Methods
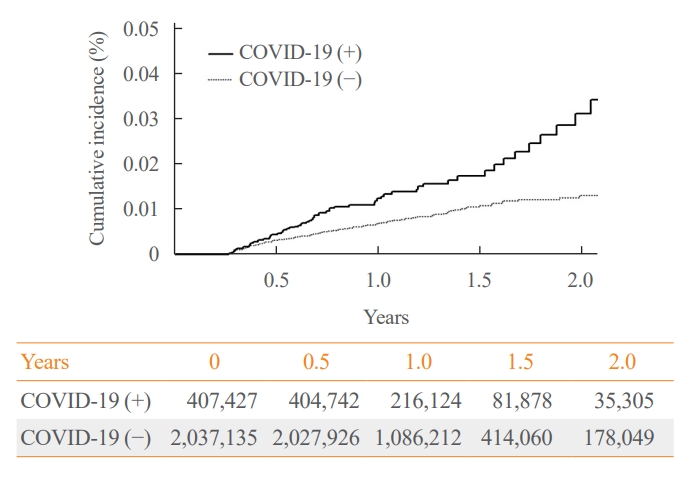
Data from a total of 422,779 COVID-19 patients and a control group of 2,113,895 individuals were analyzed. The index date was defined as the date 3 months after confirmation of COVID-19. The incidence rate (IR) of SAT and hazard ratios (HRs) were calculated per 100,000 persons. Subgroup analysis included analysis of HRs 90–179 and 180 days post-COVID-19 diagnosis; and additional analysis was conducted according to hospitalization status, sex, and age group.
Results
The IR of SAT was 17.28 per 100,000 persons (95% confidence interval [CI], 12.56 to 23.20) in the COVID-19 group and 8.63 (95% CI, 6.37 to 11.45) in the control group. The HR of COVID-19 patients was 1.76 (95% CI, 1.01 to 3.06; P=0.045). The HR of SAT was 1.39 (95% CI, 0.82 to 2.34; P=0.220) up to 6 months after the index date and 2.30 (95% CI, 1.60 to 3.30; P<0.001) beyond 6 months. The HR for SAT among COVID-19 patients was 2.00 (95% CI, 1.41 to 2.83) in hospitalized patients and 1.76 (95% CI, 1.01 to 3.06) in non-hospitalized patients compared to the control group. The IR of SAT was 27.09 (95% CI, 20.04 to 35.82) for females and 6.47 (95% CI, 3.34 to 11.30) for males. In the 19 to 64 age group, the IR of SAT was 18.19 (95% CI, 13.70 to 23.67), while the IR was 9.18 (95% CI, 7.72 to 10.84) in the 65 to 69 age group.
Conclusion
SAT could be a potential long-term complication of COVID-19. Long-term surveillance for thyroid dysfunction is needed especially in hospitalized, female and young-aged subjects. -
Citations
Citations to this article as recorded by- Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Subacute Thyroiditis in the Time of COVID-19
Hwa Young Ahn
Endocrinology and Metabolism.2024; 39(1): 186. CrossRef - Occult endocrine disorders newly diagnosed in patients with post-COVID-19 symptoms
Yasuhiro Nakano, Naruhiko Sunada, Kazuki Tokumasu, Hiroyuki Honda, Yuki Otsuka, Yasue Sakurada, Yui Matsuda, Toru Hasegawa, Daisuke Omura, Kanako Ochi, Miho Yasuda, Hideharu Hagiya, Keigo Ueda, Fumio Otsuka
Scientific Reports.2024;[Epub] CrossRef - rRisk of incident thyroid dysfunction in the post-acute phase of COVID-19: a population-based cohort study in Hong Kong
David Tak Wai Lui, Xi Xiong, Ching‐Lung Cheung, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Lanlan Li, Matthew Shing Hin Chung, Chi Ho Lee, Yu Cho Woo, Kathryn Choon Beng Tan, Carlos
Endocrine Practice.2024;[Epub] CrossRef
- Thyroid dysfunction in COVID-19

- Thyroid
- Immunoglobulin G4-Related Thyroid Disease: A Single-Center Experience and Literature Review
- Meihua Jin, Bictdeun Kim, Ahreum Jang, Min Ji Jeon, Young Jun Choi, Yu-Mi Lee, Dong Eun Song, Won Gu Kim
- Endocrinol Metab. 2022;37(2):312-322. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1318
- 3,997 View
- 179 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
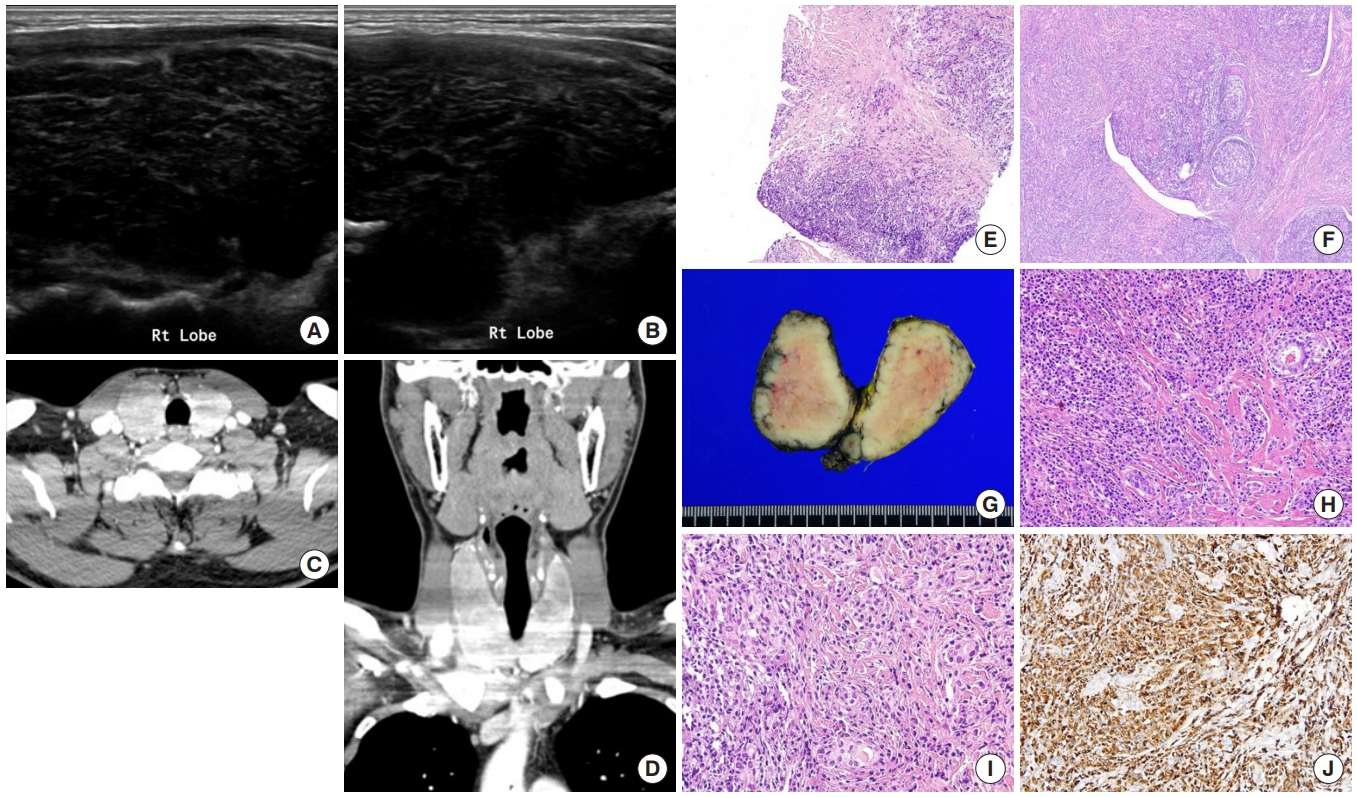
Immunoglobulin G4 (IgG4)-related disease is an entity that can involve the thyroid gland. The spectrum of IgG4-related thyroid disease (IgG4-RTD) includes Hashimoto thyroiditis (HT) and its fibrotic variant, Riedel thyroiditis, as well as Graves’ disease. The early diagnosis of IgG4-RTD is important because it is a medically treatable disease, and a delay in the diagnosis might result in unnecessary surgery. We present a case series of IgG4-RTD with a review of the literature.
Methods
We retrospectively reviewed the clinical presentation and the radiological and pathological findings of patients diagnosed with IgG4-RTD between 2017 and 2021 at a tertiary medical center in Korea. We also conducted a literature review of IgG4-RTD.
Results
Five patients were diagnosed with IgG4-RTD during the study period. The patients’ age ranged from 31 to 76 years, and three patients were men. Most patients visited the clinic for a neck mass, and hypoechogenic nodular lesions were observed on neck ultrasonography. Three patients had IgG4 HT, and two patients had IgG4 Riedel thyroiditis. All patients developed hypothyroidism that necessitated L-thyroxine replacement. The diagnosis of IgG4-RTD was confirmed after a pathological examination of the surgical specimen in the first two cases. However, the early diagnosis was possible after a core needle biopsy in three clinically suspected patients.
Conclusion
The diagnosis of IgG4-RTD requires clinical suspicion combined with serology and histological analyses using IgG4 immunostaining. The early diagnosis of IgG4-RTD is difficult; thus, biopsy with IgG4 immunostaining and serum IgG4 measurements will help diagnose patients suspected of having IgG4-RTD. -
Citations
Citations to this article as recorded by- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study
K. Kenarlı, A. B. Bahçecioğlu, Ö. B. Aksu, S. Güllü
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Reshaping the Concept of Riedel’s Thyroiditis into the Larger Frame of IgG4-Related Disease (Spectrum of IgG4-Related Thyroid Disease)
Mara Carsote, Claudiu Nistor
Biomedicines.2023; 11(6): 1691. CrossRef
- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study

- Thyroid
- Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
- Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
- Endocrinol Metab. 2022;37(2):323-332. Published online April 13, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1413
- 3,656 View
- 143 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
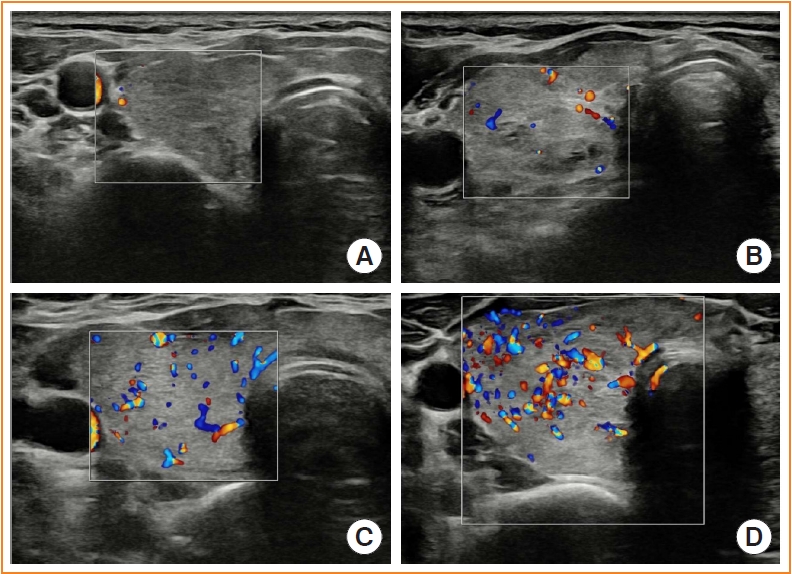
Microvascular ultrasonography (MVUS) is a third-generation Doppler technique that was developed to increase sensitivity compared to conventional Doppler. The purpose of this study was to compare MVUS with conventional color Doppler (CD) and power Doppler (PD) imaging to distinguish Graves’ disease (GD) from destructive thyroiditis (DT).
Methods
This prospective study included 101 subjects (46 GDs, 47 DTs, and eight normal controls) from October 2020 to November 2021. All ultrasonography examinations were performed using microvascular flow technology (MV-Flow). The CD, PD, and MVUS images were semi-quantitatively graded according to blood flow patterns. On the MVUS images, vascularity indices (VIs), which were the ratio (%) of color pixels in the total grayscale pixels in a defined region of interest, were obtained automatically. Receiver operating characteristic curve analysis was performed to verify the diagnostic performance of MVUS. The interclass correlation coefficient and Cohen’s kappa analysis were used to analyze the reliability of MVUS (ClinicalTrials.gov:NCT04879173).
Results
The area under the curve (AUC) for CD, PD, MVUS, and MVUS-VI was 0.822, 0.844, 0.808, and 0.852 respectively. The optimal cutoff value of the MVUS-VI was 24.95% for distinguishing GD and DT with 87% sensitivity and 80.9% specificity. We found a significant positive correlation of MVUS-VI with thyrotropin receptor antibody (r=0.554) and with thyroid stimulating immunoglobulin bioassay (r=0.841). MVUS showed high intra- and inter-observer reliability from various statistical method.
Conclusion
In a real time and quantitative manner, MVUS-VI could be helpful to differentiate GD from thyroiditis in thyrotoxic patients, with less inter-observer variability. -
Citations
Citations to this article as recorded by- Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management
Jin Wang, Ke Wan, Xin Chang, Rui-Feng Mao
World Journal of Diabetes.2024; 15(3): 348. CrossRef - The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Duplex Hemodynamic Parameters of Both Superior and Inferior Thyroid Arteries in Evaluation of Thyroid Hyperfunction Disorders
Maha Assem Hussein, Alaa Abdel Hamid, Rasha M Abdel Samie, Elshaymaa Hussein, Shereen Sadik Elsawy
International Journal of General Medicine.2022; Volume 15: 7131. CrossRef - Case 5: A 41-Year-Old Woman With Palpitation
Jiwon Yang, Kabsoo Shin, Jeongmin Lee, Jeonghoon Ha, Dong-Jun Lim, Han-Sang Baek
Journal of Korean Medical Science.2022;[Epub] CrossRef - Microvascular assessment of fascio-cutaneous flaps by ultrasound: A large animal study
Guillaume Goudot, Yanis Berkane, Eloi de Clermont-Tonnerre, Claire Guinier, Irina Filz von Reiterdank, Antonia van Kampen, Korkut Uygun, Curtis L. Cetrulo, Basak E. Uygun, Anahita Dua, Alexandre G. Lellouch
Frontiers in Physiology.2022;[Epub] CrossRef
- Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management

- Miscellaneous
- COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
- Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim, the Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2021;36(4):757-765. Published online August 17, 2021
- DOI: https://doi.org/10.3803/EnM.2021.404
- 10,317 View
- 418 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since the first outbreak of coronavirus disease 2019 (COVID-19), ongoing efforts have been made to discover an efficacious vaccine against COVID-19 to combat the pandemic. In most countries, both mRNA and DNA vaccines have been administered, and their side effects have also been reported. The clinical course of COVID-19 and the effects of vaccination against COVID-19 are both influenced by patients’ health status and involve a systemic physiological response. In view of the systemic function of endocrine hormones, endocrine disorders themselves and the therapeutics used to treat them can influence the outcomes of vaccination for COVID-19. However, there are very limited data to support the development of clinical guidelines for patients with specific medical backgrounds based on large clinical trials. In the current severe circumstances of the COVID-19 pandemic, position statements made by clinical specialists are essential to provide appropriate recommendations based on both medical evidence and clinical experiences. As endocrinologists, we would like to present the medical background of COVID-19 vaccination, as well as precautions to prevent the side effects of COVID-19 vaccination in patients with specific endocrine disorders, including adrenal insufficiency, diabetes mellitus, osteoporosis, autoimmune thyroid disease, hypogonadism, and pituitary disorders.
-
Citations
Citations to this article as recorded by- COVID-19 mRNA vaccine may trigger subacute thyroiditis
Mehmet Sözen, Ömercan Topaloğlu, Berrin Çetinarslan, Alev Selek, Zeynep Cantürk, Emre Gezer, Damla Köksalan, Taner Bayraktaroğlu
Human Vaccines & Immunotherapeutics.2024; 17(12): 5120. CrossRef - The role of co-morbidities in the development of an AEFI after COVID-19 vaccination in a large prospective cohort with patient-reported outcomes in the Netherlands
C. Ouaddouh, J.W. Duijster, T. Lieber, F.P.A.M. van Hunsel
Expert Opinion on Drug Safety.2024; 23(3): 323. CrossRef - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Prior immunization status of COVID-19 patients and disease severity: A multicenter retrospective cohort study assessing the different types of immunity
Javaria Aslam, Faisal Shahzad Khan, Muhammad Talha Haris, Hewad Hewadmal, Maryam Khalid, Mohammad Y. Alshahrani, Qurrat-ul-ain Aslam, Irrum Aneela, Urooj Zafar
Vaccine.2023; 41(2): 598. CrossRef - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(2): 253. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Inactivated SARS-CoV-2 vaccination does not disturb the clinical course of Graves’ disease: An observational cohort study
Shichen Xu, Huixin Yu, Xian Cheng, Jing Wu, Jiandong Bao, Li Zhang
Vaccine.2023; 41(38): 5648. CrossRef - Adrenal Crisis Associated With COVID-19 Vaccination in Patients With Adrenal Insufficiency
Yukako Kurematsu, Takako Mohri, Sadanori Okada, Yutaka Takahashi
JCEM Case Reports.2023;[Epub] CrossRef - Adverse Events Associated with COVID-19 Vaccination in Adolescents with Endocrinological Disorders: A Cross-Sectional Study
İbrahim Mert Erbaş, İrem Ceren Erbaş, Gözde Akın Kağızmanlı, Kübra Yüksek Acinikli, Özge Besci, Korcan Demir, Ece Böber, Nurşen Belet, Ayhan Abacı
Journal of Clinical Research in Pediatric Endocrinology.2023; 15(3): 248. CrossRef - Neue Aspekte der Glukokortikoidsubstitution bei Nebennierenrindeninsuffizienz
Tina Kienitz, Gesine Meyer
Der Internist.2022; 63(1): 12. CrossRef - Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence
Rimesh Pal, Ameya Joshi, Sanjay K. Bhadada, Mainak Banerjee, Suresh Vaikkakara, Satinath Mukhopadhyay
Endocrine Practice.2022; 28(4): 425. CrossRef - Safety of Inactivated and mRNA COVID-19 Vaccination Among Patients Treated for Hypothyroidism: A Population-Based Cohort Study
Xi Xiong, Carlos King Ho Wong, Ivan Chi Ho Au, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Kristy Tsz Kwan Lau, Chi Ho Lee, Yu Cho Woo, David Tak Wai Lui, Ian Chi Kei Wong
Thyroid.2022; 32(5): 505. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Adrenal Crisis Secondary to COVID-19 Vaccination in a Patient With Hypopituitarism
Nikolina Markovic, Anila Faizan, Chirag Boradia, Sridhar Nambi
AACE Clinical Case Reports.2022; 8(4): 171. CrossRef - The Effect of Inactivated SARS-CoV-2 Vaccines on TRAB in Graves’ Disease
LingHong Huang, ZhengRong Jiang, JingXiong Zhou, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Osteoporosis in Patients With Respiratory Diseases
Yue Ma, Shui Qiu, Renyi Zhou
Frontiers in Physiology.2022;[Epub] CrossRef - Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology
Ach Taieb, El Euch Mounira
Vaccines.2022; 10(12): 2004. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - No need of glucocorticoid dose adjustment in patients with adrenal insufficiency before COVID-19 vaccine
Tania Pilli, Cristina Dalmiglio, Gilda Dalmazio, Alfonso Sagnella, Raffaella Forleo, Lucia Brilli, Fabio Maino, Cristina Ciuoli, Maria Grazia Castagna
European Journal of Endocrinology.2022; 187(1): K7. CrossRef - Diabetes and COVID-19 Vaccination
Hae Dong Choi, Jun Sung Moon
The Journal of Korean Diabetes.2021; 22(4): 221. CrossRef
- COVID-19 mRNA vaccine may trigger subacute thyroiditis

- Thyroid
- Insights from a Prospective Follow-up of Thyroid Function and Autoimmunity among COVID-19 Survivors
- David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung, Karen Siu Ling Lam
- Endocrinol Metab. 2021;36(3):582-589. Published online June 8, 2021
- DOI: https://doi.org/10.3803/EnM.2021.983
- 10,830 View
- 265 Download
- 32 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The occurrence of Graves’ disease and Hashimoto thyroiditis after coronavirus disease 2019 (COVID-19) raised concerns that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may trigger thyroid autoimmunity. We aimed to address the current uncertainties regarding incident thyroid dysfunction and autoimmunity among COVID-19 survivors.
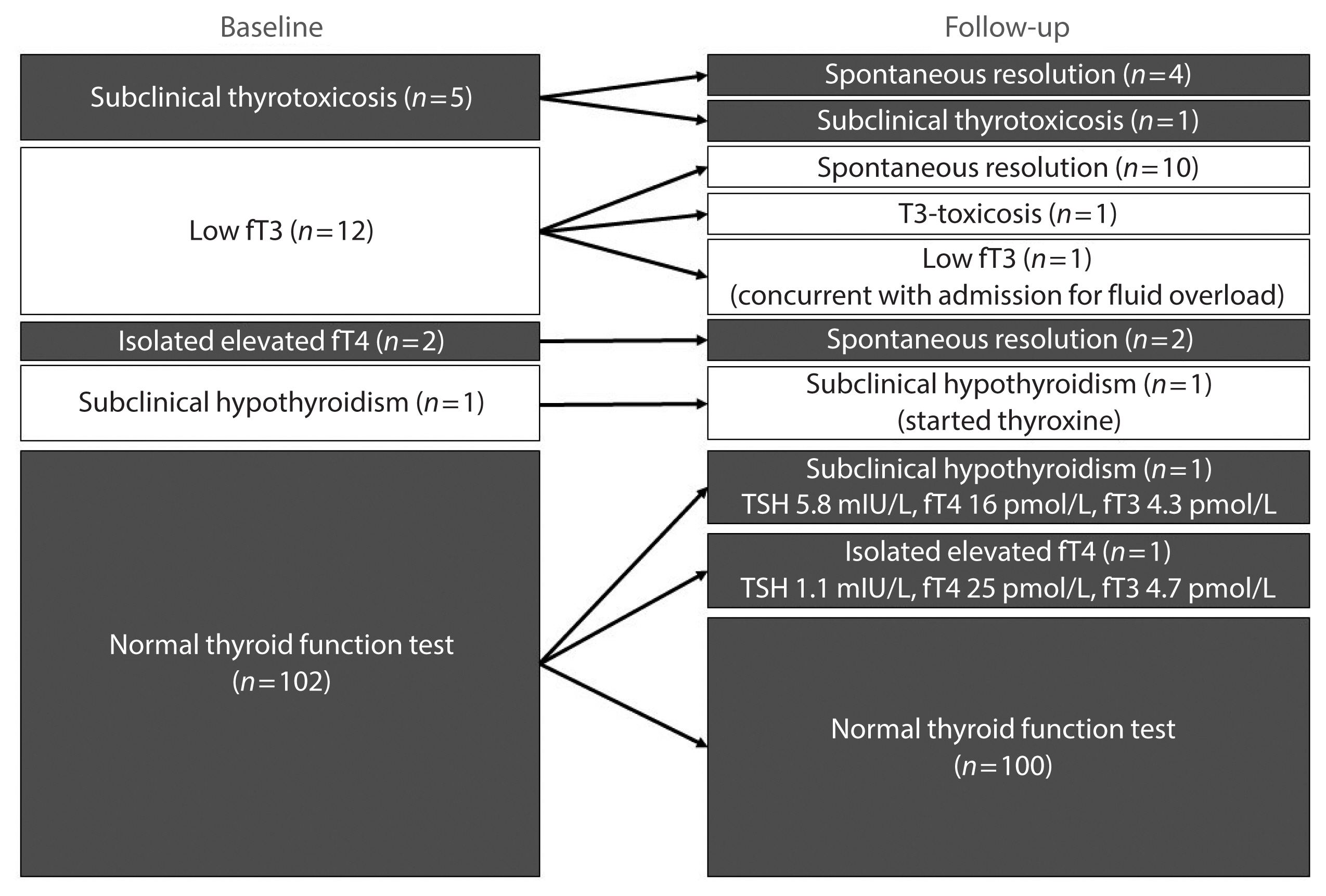
Methods
We included consecutive adult COVID-19 patients without known thyroid disorders, who were admitted to Queen Mary Hospital from July 21 to September 21, 2020 and had serum levels of thyroid-stimulating hormone, free thyroxine, free triiodothyronine (fT3), and anti-thyroid antibodies measured both on admission and at 3 months.
Results
In total, 122 patients were included. Among 20 patients with abnormal thyroid function tests (TFTs) on admission (mostly low fT3), 15 recovered. Among 102 patients with initial normal TFTs, two had new-onset abnormalities that could represent different phases of thyroiditis. Among 104 patients whose anti-thyroid antibody titers were reassessed, we observed increases in anti-thyroid peroxidase (TPO) (P<0.001) and anti-thyroglobulin (P<0.001), but not anti-thyroid stimulating hormone receptor titers (P=0.486). Of 82 patients with negative anti-TPO findings at baseline, 16 had a significant interval increase in anti-TPO titer by >12 U, and four became anti-TPO-positive. Worse baseline clinical severity (P=0.018), elevated C-reactive protein during hospitalization (P=0.033), and higher baseline anti-TPO titer (P=0.005) were associated with a significant increase in anti-TPO titer.
Conclusion
Most patients with thyroid dysfunction on admission recovered during convalescence. Abnormal TFTs suggestive of thyroiditis occurred during convalescence, but infrequently. Importantly, our novel observation of an increase in anti-thyroid antibody titers post-COVID-19 warrants further follow-up for incident thyroid dysfunction among COVID-19 survivors. -
Citations
Citations to this article as recorded by- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis
Sadra Ashrafi, Hossein Hatami, Razieh Bidhendi-Yarandi, Mohammad Hossein Panahi
BMC Endocrine Disorders.2024;[Epub] CrossRef - Does COVID-19 affect thyroid more than non-COVID-19 infections? A retrospective study
Yasemin Ucal, Muhittin Serdar, Hande Karpuzoğlu, Neval Yurttutan Uyar, Meltem Kilercik, Mustafa Serteser, Aysel Ozpinar
Turkish Journal of Biochemistry.2024;[Epub] CrossRef - Thyroiditis and COVID-19: focus on pediatric age. A narrative review
F. d’Aniello, M. E. Amodeo, A. Grossi, G. Ubertini
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - The most common persistent symptoms in patients with COVID-19 who were evaluated in the Internal Medicine polyclinic
Zeynep KOÇ, Seydahmet AKIN
The European Research Journal.2023; 9(1): 97. CrossRef - Clinical assessment of children with long COVID syndrome
Réka Garai, Péter Krivácsy, Vivien Herczeg, Fanni Kovács, Bálint Tél, Judit Kelemen, Anna Máthé, Eszter Zsáry, Johanna Takács, Dániel Sándor Veres, Attila J. Szabó
Pediatric Research.2023; 93(6): 1616. CrossRef - T Cell Receptor Sequences Amplified during Severe COVID-19 and Multisystem Inflammatory Syndrome in Children Mimic SARS-CoV-2, Its Bacterial Co-Infections and Host Autoantigens
Robert Root-Bernstein, Elizabeth Churchill, Shelby Oliverio
International Journal of Molecular Sciences.2023; 24(2): 1335. CrossRef - A Literature Review on SARS-CoV-2 and Other Viruses in Thyroid Disorders: Environmental Triggers or No-Guilty Bystanders?
Francesca Gorini, Cristina Vassalle
International Journal of Environmental Research and Public Health.2023; 20(3): 2389. CrossRef - Thyroid dysfunction as a long-term post-COVID-19 complication in mild-to-moderate COVID-19
Vesselina Yanachkova, Teodora Stankova, Radiana Staynova
Biotechnology & Biotechnological Equipment.2023; 37(1): 194. CrossRef - The Influence of SARS-CoV-2 Infection on the Thyroid Gland
Aleksandra Piekarska, Marta Góral, Marta Kozula, Aleksandra Jawiarczyk-Przybyłowska, Katarzyna Zawadzka, Marek Bolanowski
Biomedicines.2023; 11(2): 614. CrossRef - Thyroid Function Abnormalities and Outcomes in Hospitalized Patients
with COVID-19 Infection: A Cross-Sectional Study
Deepika Patel, Dukhabandhu Naik, Sadishkumar Kamalanathan, Kadhiravan Tamilarasu, Jayaprakash Sahoo, Ayan Roy, Chandhana Merugu, Varun Suryadevara
Hormone and Metabolic Research.2023; 55(03): 169. CrossRef - The Spectrum of Thyroid Function Tests and Autoantibodies During Hospitalization and After Six Months of Discharge in COVID-19 Patients: Does COVID-19 Trigger Autoimmunity?
Ziynet Alphan Uc, Pinar Yagcı, Zelal Adibelli, Cevdet Duran
Endocrine Research.2023; 48(2-3): 44. CrossRef - Increased prevalence of autoimmune thyroid disease after COVID-19: A single-center, prospective study
Alessandro Rossini, Sara Cassibba, Francesca Perticone, Simone Vasilij Benatti, Serena Venturelli, Greta Carioli, Arianna Ghirardi, Marco Rizzi, Tiziano Barbui, Roberto Trevisan, Silvia Ippolito
Frontiers in Endocrinology.2023;[Epub] CrossRef - A prospective follow-up of thyroid volume and thyroiditis features on ultrasonography among survivors of predominantly mild to moderate COVID-19
Man Him Matrix Fung, David Tak Wai Lui, Keith Wan Hang Chiu, Sherman Haynam Lee, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Chun Yiu Law, Kelvin Kai Wang To, Ching W
PeerJ.2023; 11: e15034. CrossRef - Study on Clinicopathological Features and Risk Factors of Patients with Multiple Primary Breast Cancers and Thyroid Disease
Jie Li, Yonghong Liu, Jian Jin, Qingfeng Shi, Yanting Ji, Bo Zhang, Pengfei Hu, Jinghua Pan
Mediators of Inflammation.2023; 2023: 1. CrossRef - Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
Jeongmin Lee, Gi Hyeon Seo, Keeho Song
Endocrinology and Metabolism.2023; 38(4): 455. CrossRef - Thyroid Autoimmunity and SARS-CoV-2 Infection
Poupak Fallahi, Giusy Elia, Francesca Ragusa, Sabrina Rosaria Paparo, Armando Patrizio, Eugenia Balestri, Valeria Mazzi, Salvatore Benvenga, Gilda Varricchi, Laura Gragnani, Chiara Botrini, Enke Baldini, Marco Centanni, Clodoveo Ferri, Alessandro Antonell
Journal of Clinical Medicine.2023; 12(19): 6365. CrossRef - Autoimmune complications of COVID‐19
Niloufar Yazdanpanah, Nima Rezaei
Journal of Medical Virology.2022; 94(1): 54. CrossRef - The Independent Association of TSH and Free Triiodothyronine Levels With Lymphocyte Counts Among COVID-19 Patients
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Chloe Yu Yan Cheung, Carol Ho Yi Fong, Chun Yiu Law, Kelvin Kai Wang To, Ching Wan Lam, Kathryn Choon Beng Tan, Yu Cho Woo, Ivan Fan Ngai Hung,
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comment on Khunti et al. COVID-19, Hyperglycemia, and New-Onset Diabetes. Diabetes Care 2021;44:2645–2655
Carmine Gazzaruso, Adriana Coppola, Pietro Gallotti, Ileana Terruzzi, Tiziana Montalcini, Livio Luzi
Diabetes Care.2022; 45(2): e45. CrossRef - The potential impact of COVID-19 on thyroid gland volumes among COVID-19 survivors
Emre Urhan, Zuleyha Karaca, Canan Sehit Kara, Zeynep Ture Yuce, Kursad Unluhizarci
Endocrine.2022; 76(3): 635. CrossRef - Systematic review of COVID-19 and autoimmune thyroiditis
Esra Tutal, Resat Ozaras, Hakan Leblebicioglu
Travel Medicine and Infectious Disease.2022; 47: 102314. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Should we expect a wave of type 1 diabetes following SARS‐CoV‐2 pandemic?
Laura Montefusco, Andrea Mario Bolla, Paolo Fiorina
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - COVID-19 and Thyroid Function: A Bi-Directional Two-Sample Mendelian Randomization Study
Gloria Hoi-Yee Li, Ching-Man Tang, Ching-Lung Cheung
Thyroid.2022; 32(9): 1037. CrossRef - Development of a prediction score (ThyroCOVID) for identifying abnormal thyroid function in COVID-19 patients
D. T. W. Lui, C. H. Lee, W. S. Chow, A. C. H. Lee, A. R. Tam, C. Y. Y. Cheung, C. H. Y. Fong, S. T. M. Kwok, C. Y. Law, K. K. W. To, C. W. Lam, K. C. B. Tan, Y. C. Woo, I. F. N. Hung, K. S. L. Lam
Journal of Endocrinological Investigation.2022; 45(11): 2149. CrossRef - Symptomatic Bradycardia Manifesting as Acute Hypothyroidism Following COVID-19 Infection: A Case Report
Jaydip Desai, Arsh N Patel, Courtney L Evans, Molly Triggs, Fulton Defour
Cureus.2022;[Epub] CrossRef - Schilddrüse und SARS-CoV-2
Georg Zettinig
Journal für Klinische Endokrinologie und Stoffwechsel.2022; 15(3): 100. CrossRef - Thyroid diseases are associated with coronavirus disease 2019 infection
Yutian Tian, Junyu Zhao, Tingting Wang, Haipeng Wang, Jinming Yao, Song Wang, Yaru Mou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thyrotropin Levels in Patients with Coronavirus Disease 2019: Assessment during Hospitalization and in the Medium Term after Discharge
Abdallah Al-Salameh, Noémie Scherman, Imane Adda, Juliette André, Yoann Zerbib, Julien Maizel, Jean-Daniel Lalau, Etienne Brochot, Claire Andrejak, Rachel Desailloud
Life.2022; 12(12): 2014. CrossRef - Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role?
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung,
Endocrine Practice.2021; 27(9): 894. CrossRef - Hashimoto’s thyroiditis following SARS-CoV-2 infection
Rafael Silvestre Knack, Taliê Hanada, Renata Silvestre Knack, Kamilla Mayr
BMJ Case Reports.2021; 14(8): e244909. CrossRef - Higher SARS-CoV-2 viral loads correlated with smaller thyroid volumes on ultrasound among male COVID-19 survivors
David Tak Wai Lui, Matrix Man Him Fung, Keith Wan Hang Chiu, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Wade Wei Wong, Cassandra Yuen Yan Lee, Chun Yiu Law, Kelvin K
Endocrine.2021; 74(2): 205. CrossRef - SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases
Avaniyapuram Kannan Murugan, Ali S Alzahrani
Journal of Inflammation Research.2021; Volume 14: 6191. CrossRef - POST-COVID ENDOCRINOPATHY :ABOUT A CASE ENDOCRINOPATHIE POST- COVID :À PROPOS D’UN CAS
S. Rafi, G. Elmghari, N, Elansari
INDIAN JOURNAL OF APPLIED RESEARCH.2021; : 13. CrossRef
- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis

- The Incidence of Thyroid Autoantibody in Subacute Thyroiditis and the Clinical Characteristics of Greeping Thyroiditis.
- Jae Seok Jeon, Won Bae Kim, Hae Young Park, Young Joo Park, Hyun Kyung Chung, Sang Jeon Choi, Chan Soo Shin, Kyoung Soo Park, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee, Chang Soon Koh
- J Korean Endocr Soc. 1996;11(4):438-446. Published online November 7, 2019
- 1,257 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Subacute thyroiditis is a spontaneously resolving inflammatory disorder of thyroid gland, usually associated with painful goiter and short-lived thyrotoxicosis. Although its etiology is yet to be established, much evidence suggests viral infections and genetic factors play important roles. Usually, both lobes of thyroid gland are involved simultaneously, but in some patients one lobe is involved first and the other later(creeping thyroiditis), Thyroid autoantibodies which might appear probably due to inflammatory release of thyroid antigens, are found in a variable number of patients with subacute thyroiditis. However there have been few detailed reports on their incidence in Korean patients with subacute thyroiditis. So, we were to see the elinical characteristics of patients with subacute thyroiditis with special regards to the incidence of thyroid autoantibodies and to the incidence and characteristics of creeping thyroiditis, Methods: We reviewed the clinical records of 85 patients with subacute thyroiditis(7 men and 78 wornen, meam age of 43+9 years) who had visited the thyroid clinic in Seoul National University Hospital between 1986 and 1994. Results: At initial visit, the incidenees of thyroid autoantibodies were as follows: anti- microsomal antibody 7.8%, anti-thyroglobulin antibody 22.1%, and thyratropin binding inhibitor inununglobulin 6.3%. During the follow-up period, thyroid autoantibodies appeared most frequently between the first and the second month after initial visit. Compared to those with non-creeping thyroiditis, the patients with creeping thyroiditis(21.4%) had nonspecific systemic sy~rnptoms more frequently(89% vs. 42%, p<0.05). They required steroid therapy more ftequently(89% vs. 52%, p <0.05), and needed longer duration of treatment(9.3+6.2weeks vs, 4.7+3.7weeks, p<0.05). The incidence of abnormalities in liver function and the incidence of thyroid autoantibodies were higher in non-creeping thyroiditis group. Conclusion: In accordance with previous reports, thyroid autoantibodies were detected in only a small portion of Korean patients with subacute thyroiditis. Rather different clinical manifestations and different incidences of thyroid autoantibodies between ereeping group and non-creeping group suggest differences in the pathogenetic mechanisms between those two groups. However, there is need for further study to validate such observation and to elucidate the mechanisms.

- A Clinical Study of Postpartum Autoimmute Thyroiditis.
- Hee Jin Kim, Yeon Ah Sung, Nan Ho Kyung
- J Korean Endocr Soc. 1996;11(3):302-310. Published online November 7, 2019
- 1,098 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Postpartum thyroiditis is a painless, destructive lymphocytic inflammation of the thyroid gland that occurs during the postpartum period and is associated with a high prevalence of serum thyroid autoantibodies. Clinical symptoms and laboratory fi#ndings of postpartum thyroiditis vary widely during the course of illness and the final outcome of this disease remains unpredictive in some patients. The purpose of this study is to investigate the clinical course and the predictors of the outcome of the disease. Methods: Thirty-eight patients proven to have postpartum thyroiditis at the Ewha Womans University Hospital were studied. We analyzed their clinical features, laboratory findings and duration of recovery to characterize the course of the disease. Results: Their mean age was 29.0±3.3 years and the time of diagnosis was 4.9±1.9 months after delivery. The prevailed months of delivery were November through January in this study. Twenty six patients were hypothyroid and 12 were thyrotoxic at initial thyroid function. The positive rates of antithyroglobulin and anitmicrosomal antibodies were 92%, 67% in the hypothyroid group and 75%, 67% in th thyrotoxic group respectively. TSH receptor antibodies were negative in all patients. In the hypothyroid group the titers of antimicrosomal antibodies were significantly higer than the thyrotoxic group. The titers of antimicrosomal antibodies were positively correlated with serum TSH and negatively correlated with serum T4. In all patients, the titers in thyroid function tests returned to the normal range without long-term hypothyroidism. Conclusion: The titers of antimicrosomal antibodies were significantly higher in the hypothyroid group than the thyrotoxic group. Thus the titers of antimicrosomal antibodies can help guide the physician in the care of patients with postpartum thyroiditis who will probably be hypothyroid. In this study, we were surprised that all patients became euthyroid without permanent hypothyroidism.

- A Case of Subsequent Papillary Carcinoma of the Thyroid gland and Hashimoto's Thyroiditis.
- Sang Woong Han, Yong Seon So, Seok Hwan Kim, Ki Hyun Kwon, Tae Hyeung Kim, Jong Soon Kim, Kwang Hoe Kim, Byung Doo Lee
- J Korean Endocr Soc. 1996;11(2):214-220. Published online November 7, 2019
- 1,132 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - The association of thyroid carcinoma and Hashimotos thyroiditis in same thyroid gland is controversial. Incidence of carcinoma who has Hashimotos thyroiditis has been reported from 0.5 to 22.5 per cent by Crile and by Hirabayashi et al. The reason that there are such great diffarences in the reported incidences of carcinoma in Hashimotos disease is the result of the way the material is reported. The carcinomas of the thyroid which occur in association with Hashirnotos thyroiditis are predominently papillary tumors of lower grade malignancy. Thyroid carcinoma need not be feared in patimts with Hashimotos thymiditis, if one examines the ghmd catefully. When patients with Hashimotos disease are treated with thyroxine, there is little or no tendency for Hashimotos disease propess to clinieally detectable carcinoma of the thymid, and the microcarcinoma does not appear. In this case, single thyroid nodule was detected in Hashiimotos disease patient who was treated with thyroxine. There was no significant volume change of thyroid nodule despite of TSH suppression therapy during six months. Therefore we perforrned FNABC twice, the results were highly suspicious thyroid malignancy and subtotoal thyroidectomy was performed. The final pathologic result was microscopic papillary carcinoma with background Hashlmotos thyroiditis. In conclusion, we experienced a case of subsequent microscopic papillary carcinoma of the thyroid in patient with Hashimotos thyroiditis who was TSH suppression therapy with thyroxine.

- Graves' disease associated with Hashimoto's thyroiditis.
- Seong Bin Hong, Myoung Sik Kim, Kwan Woo Lee, Mi Rin Kim, Hyoun Ho In, Kyoung Rae Kim, Young Up Cho, Young Chae Joo
- J Korean Endocr Soc. 1996;11(2):182-188. Published online November 7, 2019
- 1,170 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - Hashimotos thyroiditis and Graves disease have been thought to be the autoirnmune diseases having their distinct and separate clinical and pathologic features. Because of the partial and complete simi1arity in histologic feature, it has been hypothesized that Hashimoto's thyroiditis and Oraves disease may be interrelated. Several patients who had been diagnosed as Graves disease showed features of hypothyroidism, and were proven to have histologie features of Hashimotos thyroiditis in their thyroid tissue. Two meehanisms had been suggested to explain tbis phenomenon. One is that the combined Hashimotos thyroiditis in Graves' disease may become predominant with time, The other is that the amount of TSH receptor blocking antibody may increase in the course of Graves disease. Early recognition of these patients would be impartant to estabilish therapeutic plan. Futhermcee, extensive study of these patients would give more understanding of the mechanism of these diseases. Here we report 5 cases of clinically diagnosed Graves disease with pathologic features of Hashimotos thyroiditis or focal lymphocytic thyroiditis.

- Spontaneous Recovery from Hypothyroidism in Autommune Thyroiditis.
- Bo Youn Cho, Jae Hoon Chung, Kwang Won Kim, Kyu Jeung Ahn, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee
- J Korean Endocr Soc. 1996;11(1):30-40. Published online November 7, 2019
- 2,185 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - Background
A lifelong thyroxine therapy is indicated in all patients who have hypothyroidism as a result of autoimmune thyroiditis. However, it has been reported that some hypothyroid patients with autoimmune thyroiditis have spontaneous remission with restriction of iodine intake instead of thyroxine therapy. The purpose of study was to investigate how many hypothyroid patients with autoimmune thyroiditis can recover from hypothyroidism with restriction of iodine intake instead of thyroxine therapy and which factors predict recovery from hypothyroidism. Methods: We studied 64 patients with autoimmune thyroiditis(goitrous autoimmune thyroiditis 56, atrophic autoimmune thyroiditis 8). Thyroxine therapy was discontinued in patients with goitrous autoimmune thyroiditis on the way(group 1, n=32) or from the beginning(group 2, n=24) and atrophic autoimmune thyroiditis on the way(group 3, n-8). All patients were asked to avoid iodine-rich foods and thyroid function was monitored every one to two months for up to 35 months. Serum T3, T4, TSH concentrations, antithyroglobulin and antimicrosomal antibodies were measured by radioimmunoassay(RIA). TSH binding inhibitor immunoglobulin(TBII) was measured in serum using radioreceptor assay. Two hundred micrograms of thyrotropin releasing hormone (TRH) were given as intravenous bolus and TSH levels were measured in blood samples taken at 0, 30, and 60 minutes. All values were expressed as mean+-SEM. Statistical analysis was done with paired or non-paired t-test, ANOVA, and the Chi-square test. Statistical significance was defined as p-value below 0.05. Results: Thirteen(40.6%) of 32 patients in group 1 remained euthyroid after 12-35 months of discontinuation of thyroxine therapy. The other 19(59.4%) patients in group 1 had recurrences of hypothyroidism within 3 months after discontinuation of thyroxine therapy. In 11(45.8%) out of 24 patients in group 2, serum TSH concentrations declined below 5 mU/L within 3 months without thyroxine therapy. The other 13(54.2%) patients in group 2 remained hypothyroid till 2-16 months and the thyroxine was given. In contrast, all 8 patients in group 3 had recurrences of hypothy- roidism within 3 months after stopping thyroxine therapy. When we compared the recovered patients of goitrous autoimmune thyroiditis with the non-recovered patients of goitrous autoimmune thyroiditis, regardless of thyroxine therapy from the beginning, age at onset of disease of the 24 recovered patients was significantly younger than the 32 non-recovered patients(30.1+2.0 years vs. 40.2+ 2.4 years; p=0.004). Concl#usion: These findings suggest that 42.9% of hypothyroid patients with goitrous autoim- mune thyroiditis remain or become spontaneously euthyroid with restriction of iodine intake instead of thyroxine therapy. Young age may be a predicting factor of recovery from hypothyroidism in goitrous autoimmune thyroiditis.

- A Case of Primary Thyroid Lymphoma Involving Bone Marrow (Stage IVE) Assoeiated with Hashimoto's Thyroiditis.
- Young Kee Shong, Joong Yeol Park, Ghi Su Kim, Jae Kun Cho, Yun Ho Chu, Wan Sik Eom, Sang Hee Kim, Hyun Sook Chi, Gyung Yub Gong, Ki Up Lee
- J Korean Endocr Soc. 1994;9(4):390-394. Published online November 6, 2019
- 1,102 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Primary lymphoma of the thyroid is a relatively rare malignant tumor of the thyroid. It is known to be frequently associated with Hashimoto's thyroiditis. In Korea, a few cases of primary lymphoma of the thyroid have been reported and most of these cases were in the stage I E or II E. Recently, we experienced a case of the primary thyroid lymphoma, stage IV E associated with Hashimoto's thyroiditis in a 70-year-old woman who presented with dysphagia and dyspnea due to rapidly enlarging neck mass.She was treated with combination chemotherapy(cyclophosphamide, adriamycin, vincristine and methylprednisolone) and local radiotherapy and achieved partial response with resolution of dysphagia and dyspnea.

- A Case of Acute Suppurative Thyroiditis by Xanthomonas Maltophilia.
- Chung Gu Cho, Du Hwan Choi, Jae Bum Soh, Kwang Hyon You, Kyoung Nyeon Kim, Bong Joo Shin
- J Korean Endocr Soc. 1994;10(2):131-135. Published online November 6, 2019
- 1,019 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Acute thyroiditis(acute suppurative thyroiditis, bacterial thyroiditis, pyogenic thyroiditis) is an uncommon inflammatory disease, usually bacterial in orign, but may be fungi, parasitic organisms. A case of acute suppurative thyroiditis was reported and review of literature was made. A 51-year-old female noted pain and swelling of her neck. Cardinal physical finding on admission was enlargement of thyroid gland accompanied by tenderness and local heat. Diagnosis of acute suppurative thyroiditis was made by needle aspiration of the thyroid gland. The aspirated material showed inflammatory cells and follicular cells. In culture, Xanthomonas maltophilia was isolated. After antibiotics administration, she was discharged with improvement of tender enlargement of the thyroid gland.

- Thyroid
- Natural Killer Cells and Thyroid Diseases
- Eun Kyung Lee, John B. Sunwoo
- Endocrinol Metab. 2019;34(2):132-137. Published online June 24, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.132
- 5,913 View
- 92 Download
- 15 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Abnormal production of thyroid hormone is one of the common endocrine disorders, and thyroid hormone production declines with age. The aging process also negatively affects the immune system. An interaction between endocrine system and the immune system has been proposed to be bidirectional. Emerging evidence suggests an interaction between a lymphocyte population, called natural killer (NK) cells and thyroid gland function. Here, we review the relationship between NK cells and thyroid function and disease.
-
Citations
Citations to this article as recorded by- Tumor microenvironment in thyroid cancer: Immune cells, patterns, and novel treatments
Beatriz Febrero, Juan José Ruiz‐Manzanera, Inmaculada Ros‐Madrid, Antonio Miguel Hernández, Esteban Orenes‐Piñero, José Manuel Rodríguez
Head & Neck.2024;[Epub] CrossRef - Thyroid hormones and minerals in immunocorrection of disorders in autoimmune thyroid diseases
Viktor Kravchenko, Tamara Zakharchenko
Frontiers in Endocrinology.2023;[Epub] CrossRef - New Insights into Immune Cells and Immunotherapy for Thyroid Cancer
Yujia Tao, Peng Li, Chao Feng, Yuan Cao
Immunological Investigations.2023; 52(8): 1039. CrossRef - Innate Immunity in Autoimmune Thyroid Disease during Pregnancy
Tatjana Bogović Crnčić, Neva Girotto, Maja Ilić Tomaš, Ines Krištofić, Sanja Klobučar, Lara Batičić, Božena Ćurko-Cofek, Vlatka Sotošek
International Journal of Molecular Sciences.2023; 24(20): 15442. CrossRef - Risk Factors Associated with Mortality among Patients with COVID-19: Analysis of a Cohort of 1213 Patients in a Tertiary Healthcare Center
Carlos Alfonso Romero-Gameros, Guadalupe Vargas-Ortega, Mario Enrique Rendón-Macias, Carlos Fredy Cuevas-García, Tania Colín-Martínez, Luis Alejandro Sánchez-Hurtado, Lourdes Josefina Balcázar-Hernández, Iván Emilio De la Cruz-Rodríguez, Enid Karina Pérez
Journal of Clinical Medicine.2022; 11(10): 2780. CrossRef - Combined unsupervised and semi-automated supervised analysis of flow cytometry data reveals cellular fingerprint associated with newly diagnosed pediatric type 1 diabetes
Camillo Bechi Genzano, Eugenia Bezzecchi, Debora Carnovale, Alessandra Mandelli, Elisa Morotti, Valeria Castorani, Valeria Favalli, Angela Stabilini, Vittoria Insalaco, Francesca Ragogna, Valentina Codazzi, Giulia Maria Scotti, Stefania Del Rosso, Benedet
Frontiers in Immunology.2022;[Epub] CrossRef - Long COVID and the Neuroendocrinology of Microbial Translocation Outside the GI Tract: Some Treatment Strategies
Adonis Sfera, Carolina Osorio, Sabine Hazan, Zisis Kozlakidis, Jose Campo Maldonado, Carlos Manuel Zapata-Martín del Campo, Jonathan J. Anton, Leah Rahman, Christina V. Andronescu, Garth L. Nicolson
Endocrines.2022; 3(4): 703. CrossRef - HS3ST3A1 and CAPN8 Serve as Immune-Related Biomarkers for Predicting the Prognosis in Thyroid Cancer
Zhao-Hui Chen, Hao-Ran Yue, Jun-Hui Li, Ruo-Yu Jiang, Xiao-Ning Wang, Xue-Jie Zhou, Yue Yu, Xu-Chen Cao, Rengyun Liu
Journal of Oncology.2022; 2022: 1. CrossRef - Construction of an Expression Classifier Based on an Immune-related Ten-gene Panel for Rapid Diagnosis of Papillary Thyroid Carcinoma Risks
Jingxue Sun, Jingjing Li, Yaguang Zhang, Jun Han, Jiaxing Wei, Yanmeizhi Wu, Bing Liu, Hongyu Han, Hong Qiao
Current Bioinformatics.2022; 17(10): 924. CrossRef - Papillary Thyroid Carcinoma Landscape and Its Immunological Link With Hashimoto Thyroiditis at Single-Cell Resolution
Jun Pan, Fang Ye, Chengxuan Yu, Qinsheng Zhu, Jiaqi Li, Yaohui Zhang, Hedi Tian, Yunjin Yao, Minjie Zhu, Yibin Shen, Feng Zhu, Yingying Wang, Xinhui Zhou, Guoji Guo, Yijun Wu
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - The Intriguing Thyroid Hormones–Lung Cancer Association as Exemplification of the Thyroid Hormones–Cancer Association: Three Decades of Evolving Research
Maria V. Deligiorgi, Dimitrios T. Trafalis
International Journal of Molecular Sciences.2021; 23(1): 436. CrossRef - Mass Cytometry Studies of Patients With Autoimmune Endocrine Diseases Reveal Distinct Disease-Specific Alterations in Immune Cell Subsets
Louise Magnusson, Hugo Barcenilla, Mikael Pihl, Sophie Bensing, Daniel Espes, Per-Ola Carlsson, Rosaura Casas
Frontiers in Immunology.2020;[Epub] CrossRef - Reduced proportion and activity of natural killer cells in patients with Graves’ disease
Qingqing Yang, Li Zhang, Cheng Guo, ChunJia Kou, Yu Long, Jianting Li, Hai-Qing Zhang
European Journal of Inflammation.2020; 18: 205873922094233. CrossRef - Immunological Drivers in Graves' Disease: NK Cells as a Master Switcher
Daniela Gallo, Eliana Piantanida, Matteo Gallazzi, Luigi Bartalena, Maria Laura Tanda, Antonino Bruno, Lorenzo Mortara
Frontiers in Endocrinology.2020;[Epub] CrossRef - Quantitative and Functional Analysis of PD-1+ NK Cells in Patients With Autoimmune Thyroid Disease
Alma Cesleste Ortega-Rodríguez, Rebeca Martínez-Hernández, Adriana Monsiváis-Urenda, Ana Serrano-Somavilla, Raquel Sánchez-Gutiérrez, Roberto González-Amaro, Mónica Marazuela
The Journal of Clinical Endocrinology & Metabolism.2020; 105(11): e4001. CrossRef - Immune Cell Confrontation in the Papillary Thyroid Carcinoma Microenvironment
Zhenyu Xie, Xin Li, Yuzhen He, Song Wu, Shiyue Wang, Jianjian Sun, Yuchen He, Yu Lun, Jian Zhang
Frontiers in Endocrinology.2020;[Epub] CrossRef - Immune and Inflammatory Cells in Thyroid Cancer Microenvironment
Ferrari, Fallahi, Galdiero, Ruffilli, Elia, Ragusa, Paparo, Patrizio, Mazzi, Varricchi, Marone, Antonelli
International Journal of Molecular Sciences.2019; 20(18): 4413. CrossRef
- Tumor microenvironment in thyroid cancer: Immune cells, patterns, and novel treatments

- Thyroid
- Thyroid Dysfunction Associated with Administration of the Long-Acting Gonadotropin-Releasing Hormone Agonist
- Eun Jin Han, Ha Do Song, Ji Hoon Yang, So Young Park, Sung Hoon Kim, Hyun Koo Yoon, Chang Hoon Yim
- Endocrinol Metab. 2013;28(3):221-225. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.221
- 4,480 View
- 47 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Gonadotropin-releasing hormone (GnRH) agonist has been used in the treatment of a wide variety of sex-hormone-related diseases, as the administration of GnRH agonist can alter the secretion of gonadotropin and sex hormones. Recently, we found that the long-acting GnRH agonist aggravated hyperthyroidism and induced painless thyroiditis. This is the first report to demonstrate the association of thyroid dysfunction with GnRH agonist injection in Korea. Here, we report three cases and emphasize the clinical importance of this aggravating factor in autoimmune thyroid disease.
-
Citations
Citations to this article as recorded by- Thyroid Dysfunction after Gonadotropin-Releasing Hormone Agonist Administration in Women with Thyroid Autoimmunity
Loris Marin, Guido Ambrosini, Marco Noventa, Flavia Filippi, Eugenio Ragazzi, Francesco Dessole, Giampiero Capobianco, Alessandra Andrisani, Alexander Schreiber
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Effects of controlled ovarian stimulation on thyroid function during pregnancy
Lingfei Li, Ling Li, Ping Li
Biology of Reproduction.2022; 107(6): 1376. CrossRef - Is gonadotropin-releasing hormone agonist usage really leading to thyroid dysfunction?
Nafiye Yilmaz, Necati Hancerliogullari, Mustafa Kara, Yaprak Engin-Ustun
Interventional Medicine and Applied Science.2020; 11(3): 136. CrossRef - FANCA Polymorphism Is Associated with the Rate of Proliferation in Uterine Leiomyoma in Korea
Eunyoung Ha, Seungmee Lee, So Min Lee, Jeeyeon Jung, Hyewon Chung, Eunsom Choi, Sun Young Kwon, Min Ho Cha, So-Jin Shin
Journal of Personalized Medicine.2020; 10(4): 228. CrossRef - Effects of controlled ovarian stimulation on thyroid stimulating hormone in infertile women
Yuan-Jie Du, Xin Xin, Na Cui, Lei Jiang, Ai-Min Yang, Gui-Min Hao, Bu-Lang Gao
European Journal of Obstetrics & Gynecology and Reproductive Biology.2019; 234: 207. CrossRef - Myxedema Coma Following the Administration of Gonadotropin-releasing Hormone Agonist Complicated by Acute Pancreatitis
Naoki Gocho, Ema Aoki, Chiho Okada, Takeshi Hirashima
Internal Medicine.2018; 57(21): 3117. CrossRef - The impact of thyroid autoimmunity on IVF/ICSI outcome: a systematic review and meta-analysis
Andrea Busnelli, Alessio Paffoni, Luigi Fedele, Edgardo Somigliana
Human Reproduction Update.2016; 22(6): 775. CrossRef - The Potential Role of GnRH Agonists and Antagonists in Inducing Thyroid Physiopathological Changes During IVF
Salvatore Gizzo, Marco Noventa, Michela Quaranta, Amerigo Vitagliano, Federica Esposito, Alessandra Andrisani, Roberta Venturella, Carlo Alviggi, Mario Plebani, Michele Gangemi, Giovanni Battista Nardelli, Donato D’Antona
Reproductive Sciences.2016; 23(4): 515. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Thyroid Dysfunction after Gonadotropin-Releasing Hormone Agonist Administration in Women with Thyroid Autoimmunity


 KES
KES

 First
First Prev
Prev



