Articles
- Page Path
- HOME > Endocrinol Metab > Volume 31(3); 2016 > Article
-
Original ArticleClinical Study Prognostic Factors in Patients Hospitalized with Diabetic Ketoacidosis
- Avinash Agarwal1, Ambuj Yadav1, Manish Gutch1, Shuchi Consul2, Sukriti Kumar3, Ved Prakash4, Anil Kumar Gupta5, Annesh Bhattacharjee1
-
Endocrinology and Metabolism 2016;31(3):424-432.
DOI: https://doi.org/10.3803/EnM.2016.31.3.424
Published online: September 1, 2016
1Department of Medicine, King George's Medical College, Lucknow, India.
2Department of Obstetrics and Gynecology, King George's Medical College, Lucknow, India.
3Department of Radiodiagnosis, King George's Medical College, Lucknow, India.
4Department of Pulmonary Medicine, King George's Medical College, Lucknow, India.
5Department of Physical Medicine and Rehabilitation, King George's Medical College, Lucknow, India.
- Corresponding author: Manish Gutch. Department of Medicine, King George's Medical College, Chowk, Shah Mina Road, Lucknow 226003, India. Tel: +91-522-2257242, Fax: +91-522-2258797, manish07gutch@gmail.com
Copyright © 2016 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Diabetic ketoacidosis (DKA) is characterized by a biochemical triad of hyperglycemia, acidosis, and ketonemia. This condition is life-threatening despite improvements in diabetic care. The purpose of this study was to evaluate the clinical and biochemical prognostic markers of DKA. We assessed correlations in prognostic markers with DKA-associated morbidity and mortality.
-
Methods
- Two hundred and seventy patients that were hospitalized with DKA over a period of 2 years were evaluated clinically and by laboratory tests. Serial assays of serum electrolytes, glucose, and blood pH were performed, and clinical outcome was noted as either discharged to home or death.
-
Results
- The analysis indicated that significant predictors included sex, history of type 1 diabetes mellitus or type 2 diabetes mellitus, systolic blood pressure, diastolic blood pressure, total leukocyte count, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, blood urea nitrogen, serum creatinine, serum magnesium, serum phosphate, serum osmolality, serum glutamic oxaloacetic transaminases, serum glutamic pyruvic transaminases, serum albumin, which were further regressed and subjected to multivariate logistic regression (MLR) analysis. The MLR analysis indicated that males were 7.93 times more likely to have favorable outcome compared with female patients (odds ratio, 7.93; 95% confidence interval, 3.99 to 13.51), while decreases in mean APACHE II score (14.83) and serum phosphate (4.38) at presentation may lead to 2.86- and 2.71-fold better outcomes, respectively, compared with higher levels (APACHE II score, 25.00; serum phosphate, 6.04).
-
Conclusion
- Sex, baseline biochemical parameters such as APACHE II score, and phosphate level were important predictors of the DKA-associated mortality.
- Diabetes mellitus is a clinically and genetically heterogeneous group of metabolic disorders that manifest in an abnormally high level of glucose in the blood. The hyperglycemia is a result of an insulin secretion deficiency caused by pancreatic β-cell dysfunction or resistance to the action of insulin in liver, adipose tissue, and muscle or a combination of these issues. Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of diabetes mellitus [12]. It is characterized by a triad of hyperglycemia, high anion gap metabolic acidosis, and ketonemia and represents a state of insulin deficiency and concurrent elevation in counter regulatory hormones [2]. The annual incidence ranges from 4.6 to 8 cases per 1,000 diabetic patients. DKA is associated with a mortality rate of 2% to 10% [2], while the mortality rates of hyperglycemic emergencies in Sub-Saharan Africa and Asia range from 30% to 44% [23]. The estimated mortality rate of DKA ranges between 5% to 10%, and the rate of hyperosmolar hyperglycemic syndrome varies from 10% to 50% [4]. DKA occurs more commonly in patients who have type 1 diabetes mellitus (T1DM) compared with patients who have type 2 diabetes mellitus (T2DM) [5]. However, recent data suggest that African American and Hispanic patients with T2DM are more likely to develop DKA than their Caucasian patient counterparts [67]. Management is directed to treating the precipitating factors and correcting dehydration, hyperglycemia, and electrolyte abnormalities. Despite all of the available guidelines, DKA continues to be inadequately managed, even in teaching hospitals [89]. This study evaluated the clinical and laboratory parameters that affect DKA outcomes at a tertiary care center. The primary objective of this study was to correlate final outcome with different confounding covariates (demographic characteristics, clinical characteristics, biochemical parameters) at presentation (admission).
INTRODUCTION
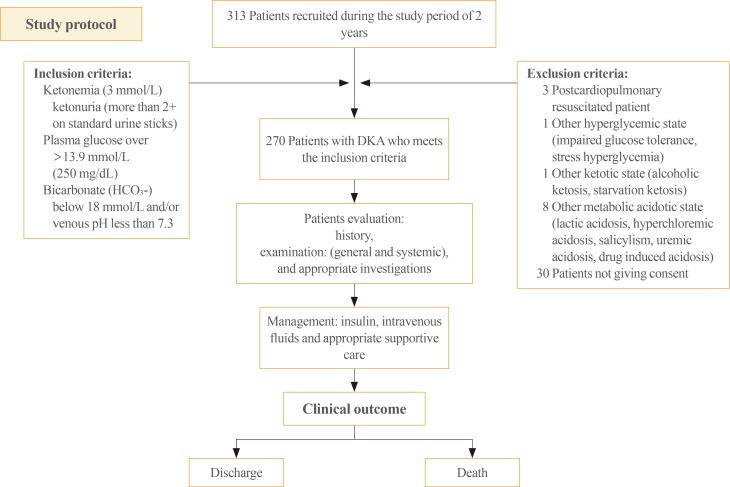
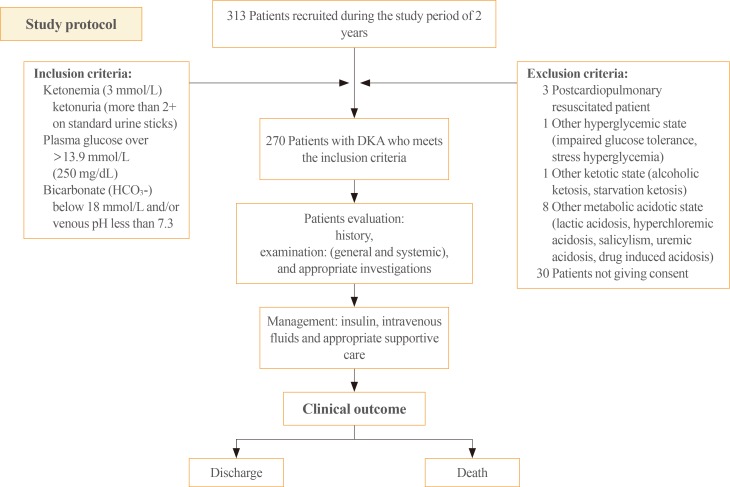
- This study was conducted in the Department of Medicine and Endocrinology Unit of the Department of Medicine at a tertiary care center in the northern part of India, over a study period of 2 years, from July 2012 to June 2014. Patients were included if they fulfilled all of the following criteria: serum glucose >13.9 mmol/L (>250 mg/dL, enzymatic method), serum bicarbonate concentration <18 mmol/L, arterial pH <7.30 (selective ion exchange method), and ketonemia (3 mmol/L) and overt or significant ketonuria (more than 2+ on standard urine sticks). Postcardiopulmonary resuscitated patients, other hyperglycemic states (impaired glucose tolerance, stress hyperglycemia), other ketotic states (alcoholic ketosis, starvation ketosis), other metabolic acidotic states (lactic acidosis, hyperchloremic acidosis, salicylism, uremic acidosis, drug-induced acidosis) and patients that did not consent were not included. Informed consent was obtained from every patient before study inclusion. The study was approved by the Local Ethics Committee.
- Patient evaluation
- Patients were evaluated on the basis of history and physical examination (general and systemic), and appropriate investigations were performed, based on patient status, including hemoglobin, total leukocyte count (TLC), differential leukocyte count, platelet count, hematocrit, fasting lipid profile, random blood sugar (RBS), pH, sodium, potassium, ionic calcium, magnesium, phosphate, bicarbonate, serum urea, serum creatinine, hemoglobin A1c (HbA1c), fasting and postprandial blood sugar, liver function test, bilirubin, serum glutamic oxaloacetic transaminases (SGOT), serum glutamic pyruvic transaminases (SGPT), serum protein, serum albumin, C-reactive protein (CRP), thyroid-stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), and serum lipase.
- Additional testing was performed as needed, including an electrocardiography, to search for the source of infection, in addition to routine urine and microscopy tests and culture sensitivity, blood culture and sensitivity, sputum culture and sensitivity, and a chest X-ray. After initial patient evaluation and investigations, the patients were graded according to Glasgow Coma Scale (GCS) and Acute Physiology and Chronic Health Evaluation II (APACHE II) scoring systems.
- Methodology
- Two hundred and seventy patients that were hospitalized with DKA over a period of 2 years were evaluated based on clinical and laboratory tests. They were managed with standard care that included insulin, intravenous fluids, and appropriate supportive care. Serial assays of serum electrolytes, glucose, and blood pH were analyzed and correlated with clinical outcomes of either discharge to home or death (Fig. 1).
- Statistical analysis
- Continuous data were summarized as mean±SD, while discrete (categorical) data are reported as number and percentage. Two continuous independent groups were compared by parametric independent Student t test, and the significance of the parametric t test was validated with the nonparametric alternative Mann-Whitney U test, where appropriate. Discrete (categorical) groups were compared by chi-square tests. Predictors of final outcome were evaluated using multivariate logistic regression analysis. A two-sided (α=2) P<0.05 was considered statistically significant. All analyses were performed on STATISTICA software version 17 (StatSoft Inc., Chicago, IL, USA).
METHODS
- The study evaluated clinical and laboratory parameters that affect DKA outcomes at a tertiary care center. A total of 270 patients were recruited and evaluated. The comparative details are summarized below.
- Demographic characteristics
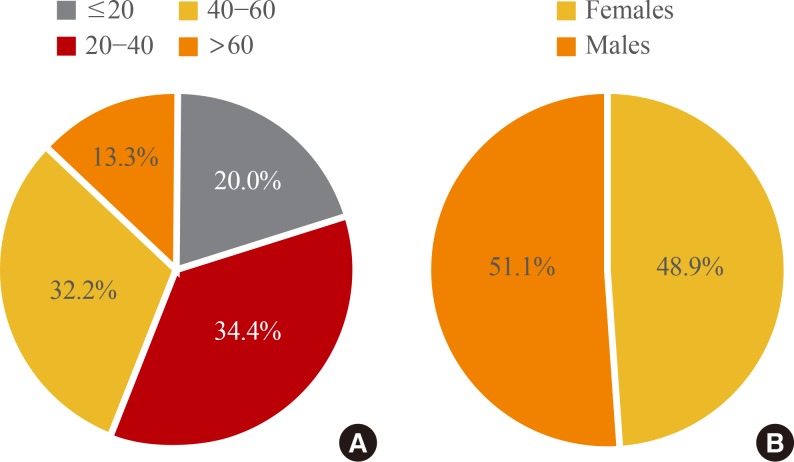
- Table 1, Fig. 2 show the age and sex distributions of patients included in this study. The ages of study subjects ranged between 13 to 80 years with a mean±SD of 38.99±18.32 years and a median of 39 years. The majority of patients were younger than 40 years (54.4%) and were male (51.1%). At the final evaluation, a total of 189 patients were discharged (70.0%), while 81 patients were deceased (30.0%). The final outcome was not associated with age (χ2=5.98, P=0.112), although favorable outcome was 23.8% more frequent in the lower age (<40 years) group than the higher age (≥40 years) group. Favorable outcome was significantly associated with sex and was significantly more frequent (33.4%) in males compared to females (33.3% vs. 66.7%, χ2=20.34, P<0.001). In this study, newly diagnosed T1DM accounted for about 62.6% (115/270) of cases, and T2DM was present in about 24.5% (155/270) of the total study population.
- Precipitating factors
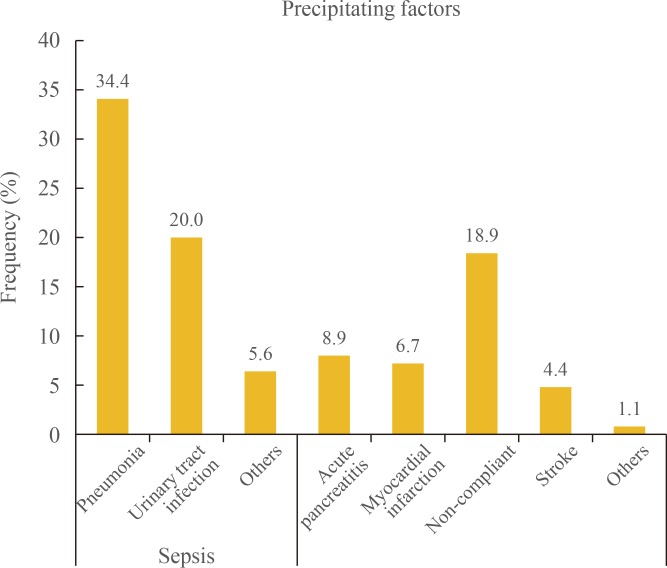
- Precipitating factors are shown in Fig. 3. Many patients experienced sepsis (infection) as a precipitating factor (60.0%), and there was also a high incidence of pneumonia (34.4%). Other precipitating factors were non-compliance (18.9%), acute pancreatitis (8.9%), myocardial infarction (6.7%), stroke (4.4%), and others (1.1%).
- Clinical characteristics
- The clinical characteristics systolic blood pressure (SBP) and diastolic blood pressure (DBP) were significantly (P<0.001) associated with final outcome. Patients who had lower mean±SD) SBP and DBP at presentation, 90 (89.85±21.28) and 54 mm Hg (54.07±13.23), respectively, had significantly (P<0.001) poorer outcomes (death) compared to those with higher mean±SD, SBP and DBP, 110.0 (110.86±16.60) and 67.0 mm Hg (67.24±11.81), respectively (Table 2). History of T1DM or T2DM was found to be significantly (P<0.05) associated with final outcome. Patients with a history of T1DM had significantly better outcomes (31.7% vs. 11.1%, χ2=4.23, P=0.040), while patients with a history of T2DM had significantly poorer outcomes (36.5% vs. 59.3%, χ2=3.98, P=0.046). In addition, history of treatment and newly-diagnosed DM were not associated with final outcome (Table 2). The APACHE II score was significantly (P<0.001) associated with final outcome. Patients with a higher mean±SD APACHE II score at presentation, 25.0 (25.00±9.74), had significantly poorer outcomes compared to those that had a lower mean±SD APACHE II score of about 15.0 (14.83±5.95) at presentation. However, GCS score was not significantly associated (P>0.05) with final outcome even though there was a higher mortality rate (11.2%) in patients with a lower (GCS <9) score compared to those with higher score (GCS >9) (44.4% vs. 55.6%, χ2=5.16, P=0.076) (Table 2).
- Biochemical profile
- Biochemical features of blood urea, serum creatinine, serum magnesium, serum phosphate, SGOT, SGPT, and serum albumin were found to be significantly (P<0.05, P<0.01, or P<0.001) associated with the final outcome or differed significantly between the two outcomes. However, hemoglobin, platelet count, hematocrit, HbA1c, serum sodium, serum potassium, serum calcium (total), serum calcium (ionic), CRP, T3, T4, TSH, serum cholesterol, triglycerides, serum high density lipoprotein, serum low density lipoprotein, serum very low density lipoprotein, serum bilirubin, serum alkaline phosphatase, and serum protein were similar (P>0.05) between the two outcomes, i.e., did not differ statistically (Table 3). TLC and serum osmolality were both significantly (P<0.05 or P<0.001) associated with final outcome. Patients with TLC ≤16,000.0 (median cutoff) and serum osmolality up to 320.0 Osm/mL at presentation had significantly (36.6% and 42.9%, respectively) more favorable outcomes compared to those that had TLC >16,000.0 and serum osmolality >320.0 Osm/mL, respectively. However, RBS, pH, bicarbonate, and serum lipase were not found to be associated with the final outcome (Table 4).
- Predictors of final outcome
- The significant predictors of final outcome were sex, history of T1DM or T2DM, SBP, DBP, TLC, APACHE II score, blood urea nitrogen (BUN), serum creatinine, serum magnesium, serum phosphate, serum osmolality, SGOT, SGPT, and serum albumin, and these predictors were further regressed together and subjected to MLR. The MLR analysis revealed that males had 7.93-fold better outcomes compared to females (odds ratio, 7.93; 95% confidence interval [CI], 3.99 to 13.51), while decrease in mean APACHE II score (14.83) and serum phosphate (4.38) at presentation led to 2.86 (OR, 2.86; 95% CI, 1.72 to 7.03) and 2.71 (OR, 2.71; 95% CI, 1.51 to 6.99) fold better outcomes, respectively, compared to those with higher levels (APACHE II score, 25.00; serum phosphate, 6.04). However, the other variables were not statistically significantly associated with outcome (P>0.05) (Table 5).
RESULTS
- In our study, a total of 270 patients were enrolled with the aim to evaluate the clinical and biochemical prognostic markers of DKA and to correlate prognostic markers with mortality.
- At final evaluation, of the 270 patients, 189 patients were discharged (70.0%), while 81 patients were deceased (30.0%). These results contrasted with the studies by Ellemann et al. [10], where mortality rates ranged from 2.5% to 9%. This may be because the aforementioned study had mortality rates that were reported and associated with DKA alone and excluded mortality attributable to factors that precipitated DKA. Other factors that contributed to higher mortality in the present study could be due to limited resources in developing countries, greater patient load in tertiary care health centers, and late referrals [11]. The mortality in patients with DKA is rarely caused by metabolic complications of hyperglycemia or metabolic acidosis and is usually related to underlying medical illnesses that precipitate the metabolic decompensation. In another study conducted by Oschatz et al. [12] at the Department of Emergency Medicine, Vienna General Hospital-University of Vienna Medical School, Austria, the mortality was 29% in patients with DKA, which was similar to the results of our study.
- In our study, sepsis was the most common precipitating factor of DKA and was identified in 60% of cases. Pneumonia (34%) and urinary tract infection (20%) accounted for the majority of infections. Other conditions that precipitated DKA were non-compliance (18.9%), acute pancreatitis (8.9%), myocardial infarction (6.7%), stroke (4.4%), and others (1.1%). Umpierrez et al. [13] also stated that "infection is the most common precipitating factor for DKA, occurring in 30% to 50% of cases. Urinary tract infection and pneumonia account for the majority of infections," which supported the results of this study. However, in a study conducted by Randall et al. [14], insulin discontinuation (non-compliance) was the leading precipitating cause in 68% of patients; other causes were new-onset diabetes (10%), infection (15%), medical illness (4%), and undetermined causes (3%).
- Patient age in the present study ranged between 13 to 80 years with a mean±SD of 38.99±18.32 years. In addition, 54.4% of the patients were younger than 40 years, and subjects were predominantly male (51.1%). Kitabchi et al. [5] found that most patients with DKA were between the ages of 18 and 44 years (56%) and 45 and 65 years (24%), with only 18% of patients <20 years of age. Barski et al. [15] concluded that advanced age was an independent predictor of mortality; however, in the present study, the final outcome was not statistically significantly associated with age, although the favorable outcomes were 23.8% higher in the lower age (<40 years) group than the higher age (≥40 years) group. This may be due to the small sample size, indicating that additional larger studies are needed. Favorable outcome was found significantly associated with sex in this study and was significantly higher (33.4%) in males compared to females. The possible reasons for increased mortality in females might be attributable to decreased health seeking behavior among females and because decision-making power lies with the male sex in our country, which can lead to very infrequent visits to primary care health center for disease treatment, which cause late referrals of female patients to tertiary care health centers. The MLR analysis found that sex was a significant and independent predictor of final outcome. The MLR analysis further revealed that males had a 7.93-fold higher favorable (discharged) outcome compared to females. We did not identify any other studies that correlated sex with mortality in DKA patients. Additionally, patients with T2DM had significantly poorer outcomes (36.5% vs. 59.3%, χ2=3.98, P=0.046) than patients with T1DM in DKA. Barski et al. [15] also reported similar results and indicated that "DKA in patients with T2DM is a more severe disease with worse outcomes compared with T1DM."
- Clinical characteristics of SBP and DBP of patients at presentation were found to be significantly (P<0.001) associated with final outcome. Patients that had lower mean±SD SBP and DBP at presentation, 90±21.28 and 54±13.23 mm Hg, respectively, had significantly (P<0.001) poorer outcomes (death) compared with those that had higher mean±SD SBP and DBP of 110.0±16.60 and 67.0±11.81 mm Hg, respectively. Similar correlations were also found in studies by Bassyouni et al. [16] and Otieno et al. [17], who reported that "hypotension was associated with higher mortality rate among patients with DKA."
- Patients with DKA may present with altered sensorium. In this study, GCS score was not significantly associated with final outcome; however, the P value was 0.076, which indicated that there is a trend toward better outcome if GCS is high. In the study by Otieno et al. [17], altered level of consciousness was a major predictor of mortality in DKA patients. Hence, additional, larger studies are needed to show the association between GCS and mortality. The APACHE II score calculated at presentation was found to be significantly (P<0.001) associated with the final outcome. Patients who had higher mean±SD APACHE II score of 25.0±9.74 had significantly increased mortality compared to those with a lower mean 15.0±5.95 score. We were not able to identify any other studies that showed direct correlation between APACHE II score and mortality in DKA.
- Analysis of the hematological parameters at presentation indicated that there was no significant association with final outcome, with the exception of TLC. Patients with TLC ≤16,000 mm3 (median cutoff) at presentation had 42.9% better outcomes compared to those with TLC >16,000/mm3. According to Slovis et al. [18], TLC in the range of 10,000 to 15,000/mm3 is expected in DKA and may not be indicative of an infectious process; however, leucocytosis with cell count >25,000/mm3 may indicate sepsis and require further evaluation. Leucocytosis in DKA is attributed to stress and may be correlated with elevated levels of cortisol and norepinephrine [19]. Because TLC >25,000/mm3 indicates sepsis, patients with DKA that also have sepsis have increased mortality, a finding supported by Oschatz et al. [12].
- Biochemical features including BUN, serum creatinine, serum magnesium, serum phosphate, N-terminal prohormone of brain natriuretic peptide, SGOT, SGPT, and serum albumin were found to be significantly (P<0.05, P<0.01, or P<0.001) associated with final outcome or differed significantly between the two outcomes. Increased levels of BUN and serum creatinine at presentation were found to be significantly associated with increased mortality. According to Otieno et al. [17], "all patients in the study who died had poor renal functions." The same result was reproduced in the present study.
- In this study, increased level of serum phosphate at presentation was associated with increased mortality. Additionally, MLR found that serum phosphate was a significant and independent predictor of final outcome. Kebler et al. [20] also concluded that hyperphosphatemia is common in DKA, prior to therapy. The increase in serum phosphate is likely to be due to a transcellular shift. Potential factors of this shift include serum glucose, through its osmotic effect, and organic anions. In another study by Shen and Braude et al. [21], it was concluded that initial hyperphosphatemia is reflective of intravascular volume depletion and prerenal renal impairment. However, correlation of serum phosphate with mortality has not been studied in the available literature, suggesting the need for further studies.
- Serum osmolality was significantly associated with final outcome. The patients with serum osmolality ≤320.0 mOsmol/kg-water at presentation had significantly better outcomes (42.9%) than patients with serum osmolality ≥320.0 mOsm/kg. Jayashree and Singhi et al. [22] concluded that serum osmolality at admission was the most important predictor of mortality. In the present study, increased levels of SGOT, SGPT, and serum magnesium and decreased level of serum albumin were also significantly associated with increased mortality. However, there is a lack of studies for comparison; therefore, additional studies are needed to conclude any association with final outcome. Finally, HbA1c, pH, CRP, serum lipase, thyroid profile, and lipid profile were similar (P>0.05) between the two outcomes, and no statistically significant correlations were identified.
- In conclusion, DKA is characterized by a biochemical triad of hyperglycemia, acidosis, and ketonemia. It continues to be a life-threatening condition despite improvements in diabetic care. Timely identification and intervention are imperative for adequate treatment. This study determined that sex, baseline biochemical parameters such as the APACHE II score, and phosphate level were important predictors of DKA-associated mortality.
- This was a cross-sectional study, and patients were assessed at the time of admission and during the hospital stay based on stimulated C-peptide level and by positive glutamic acid decarboxylase 65 and islet cell antibody levels to classify them with T1DM or T2DM. We did not follow the patients after discharge, so we were unable to determine if patients switched to oral hypoglycemic agents or remained on insulin.
DISCUSSION
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
Article information
- 1. Kearney T, Dang C. Diabetic and endocrine emergencies. Postgrad Med J 2007;83:79–86. ArticlePubMedPMC
- 2. Delaney MF, Zisman A, Kettyle WM. Diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic syndrome. Endocrinol Metab Clin North Am 2000;29:683–705. ArticlePubMed
- 3. Chu CH, Lee JK, Lam HC, Lu CC. Prognostic factors of hyperglycemic hyperosmolar nonketotic state. Chang Gung Med J 2001;24:345–351. PubMed
- 4. National Diabetes Data Group. National Institute of Diabetes and Digestive and Kidney Diseases. Chapter 13, Acute metabolic complications in diabetes. Diabetes in America; 2nd ed. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1995. p. 283–292.
- 5. Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Diabetes Care 2006;29:2739–2748. ArticlePubMed
- 6. Umpierrez GE, Smiley D, Kitabchi AE. Narrative review: ketosis-prone type 2 diabetes mellitus. Ann Intern Med 2006;144:350–357. ArticlePubMed
- 7. Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V. New profiles of diabetic ketoacidosis: type 1 vs type 2 diabetes and the effect of ethnicity. Arch Intern Med 1999;159:2317–2322. ArticlePubMed
- 8. Singh RK, Perros P, Frier BM. Hospital management of diabetic ketoacidosis: are clinical guidelines implemented effectively? Diabet Med 1997;14:482–486. ArticlePubMed
- 9. Sola E, Garzon S, Garcia-Torres S, Cubells P, Morillas C, Hernandez-Mijares A. Management of diabetic ketoacidosis in a teaching hospital. Acta Diabetol 2006;43:127–130. ArticlePubMedPDF
- 10. Ellemann K, Soerensen JN, Pedersen L, Edsberg B, Andersen OO. Epidemiology and treatment of diabetic ketoacidosis in a community population. Diabetes Care 1984;7:528–532. ArticlePubMed
- 11. Gutch M, Razi SM, Kumar S, Gupta KK. Diabetes mellitus: trends in northern India. Indian J Endocrinol Metab 2014;18:731–734. ArticlePubMedPMC
- 12. Oschatz E, Mullner M, Herkner H, Laggner AN. Multiple organ failure and prognosis in adult patients with diabetic ketoacidosis. Wien Klin Wochenschr 1999;111:590–595. PubMed
- 13. Umpierrez GE, Murphy MB, Kitabchi AE. Diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Diabetes Spectr 2002;15:28–36.Article
- 14. Randall L, Begovic J, Hudson M, Smiley D, Peng L, Pitre N, et al. Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Diabetes Care 2011;34:1891–1896. ArticlePubMedPMC
- 15. Barski L, Nevzorov R, Harman-Boehm I, Jotkowitz A, Rabaev E, Zektser M, et al. Comparison of diabetic ketoacidosis in patients with type-1 and type-2 diabetes mellitus. Am J Med Sci 2013;345:326–330. ArticlePubMed
- 16. Bassyouni A, El Ebrashy I, El Hefnawy H. Epidemiology of diabetic ketoacidosis in National Institute of Diabetes and Endocrinology. Endocr Abstr 2012;29:659.
- 17. Otieno CF, Kayima JK, Mbugua PK, Amayo AA, Mcligeyo SO. Prognostic factors in patients hospitalised with diabetic ketoacidosis at Kenyatta National Hospital, Nairobi. East Afr Med J 2010;87:66–73. ArticlePubMed
- 18. Slovis CM, Mork VG, Slovis RJ, Bain RP. Diabetic ketoacidosis and infection: leukocyte count and differential as early predictors of serious infection. Am J Emerg Med 1987;5:1–5. ArticlePubMed
- 19. Razavi Nematollahi L, Kitabchi AE, Stentz FB, Wan JY, Larijani BA, Tehrani MM, et al. Proinflammatory cytokines in response to insulin-induced hypoglycemic stress in healthy subjects. Metabolism 2009;58:443–448. ArticlePubMed
- 20. Kebler R, McDonald FD, Cadnapaphornchai P. Dynamic changes in serum phosphorus levels in diabetic ketoacidosis. Am J Med 1985;79:571–576. ArticlePubMed
- 21. Shen T, Braude S. Changes in serum phosphate during treatment of diabetic ketoacidosis: predictive significance of severity of acidosis on presentation. Intern Med J 2012;42:1347–1350. ArticlePubMed
- 22. Jayashree M, Singhi S. Diabetic ketoacidosis: predictors of outcome in a pediatric intensive care unit of a developing country. Pediatr Crit Care Med 2004;5:427–433. ArticlePubMed
References
Demographic Characteristics of the Patients
Associations of Final Outcome with Clinical Characteristics
Values are expressed as mean±SD or number (%).
SBP, systolic blood pressure; DBP, diastolic blood pressure; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; CVA, cerebrovascular accident; CAD, coronary artery disease; HTN, hypertension; OHA, oral hypoglycemic agents; DM, diabetes mellitus; GCS, Glasgow Coma Scale; APACHE II, Acute Physiology and Chronic Health Evaluation II.
Associations between Continuous Biochemical Profiles and Final Outcome
Values are expressed as mean±SD.
CRP, C-reactive protein; T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; VLDL, very low density lipoprotein; SGOT, serum glutamic oxaloacetic transaminases; SGPT, serum glutamic pyruvic transaminases; SALP, serum alkaline phosphatase.
Associations between Categorical Biochemical Profiles and Final Outcome
Predictors of Final Outcome by Multivariate Logistic Regression Analysis
SE, standard error; OR, odds raio; CI, confidence interval; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; SBP, systolic blood pressure; DBP, diastolic blood pressure; TLC, total leukocyte count; APACHE II, Acute Physiology and Chronic Health Evaluation II; BUN, blood urea nitrogen; SGOT, serum glutamic oxaloacetic transaminases; SGPT, serum glutamic pyruvic transaminases.
aOR with respect to females; bOR with respect to No.
Figure & Data
References
Citations

- Prognosis of patients with extreme acidosis on admission to the emergency department: A retrospective cohort study
Amichai Gutgold, Shaden Salameh, Jeries Nashashibi, Yonatan Gershinsky
The American Journal of Emergency Medicine.2024; 76: 36. CrossRef - The critical role of pen needles and training in insulin delivery
Tracey Sainsbury
British Journal of Nursing.2024; 33(5): 242. CrossRef - Clinical characteristics of people with diabetic ketoacidosis at a clinic in The Gambia: a retrospective study
Orighomisan F Agboghoroma, Modou Jobe, Karen Forrest
Journal of Endocrinology, Metabolism and Diabetes of South Africa.2023; 28(1): 14. CrossRef - Elevated alanine transaminase is nonlinearly associated with in-hospital death in ICU-admitted diabetic ketoacidosis patients
Qiaoling Liu, Chen Gong, Yunjie Geng, Jiuhong You
Diabetes Research and Clinical Practice.2023; 197: 110555. CrossRef - Diabetic keto-acidosis in pancreatic diabetes – how is it different from DKA in type 1 or type 2 DM?
Sunetra Mondal, Riddhi DasGupta, Moushumi Lodh, Ashok Parida, Mandira Haldar, Arunangshu Ganguly
International Journal of Diabetes in Developing Countries.2023;[Epub] CrossRef - Comparative study of diabetic ketoacidosis in the elderly and non-elderly patients: A nine-year experience from an academic hospital in North India
Ashok Kumar Pannu, Ravindran Kiran, Abhishek Kumar, Saurabh Chandrabhan Sharda, Mandip Bhatia, Atul Saroch, Pinaki Dutta, Navneet Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(12): 102903. CrossRef - Clinical Profile and Outcome of Diabetic Ketoacidosis in Type 1 and Type 2 Diabetes: A Comparative Study
Sachin Kamle, Madhuri Holay, Prashant Patil, Parimal Tayde
Vidarbha Journal of Internal Medicine.2022; 32: 21. CrossRef - Effect of subjective tool based aerobic exercise on pulmonary functions in patients with type 2 diabetes mellitus – a feasibility RCT
M. Saini, J. Kaur
Comparative Exercise Physiology.2022; 18(3): 239. CrossRef - Clinical characteristics and outcomes of care in patients hospitalized with diabetic ketoacidosis
Mohsen S. Eledrisi, Haifaa Alkabbani, Malk Aboawon, Aya Ali, Imad Alabdulrazzak, Maab Elhaj, Ashraf Ahmed, Hazim Alqahwachi, Joanne Daghfal, Salem A. Beshyah, Rayaz A. Malik
Diabetes Research and Clinical Practice.2022; 192: 110041. CrossRef - An Audit of Factors Impacting the Time to Resolution of the Metabolic Parameters in Diabetic Ketoacidosis Patients
Muath F AlWahbi , Sami H Alharbi, Saleh A Almesned, Faisal A Alfawzan, Rayan T Alsager, Abdullah A AlHojailan, Emad A Alfadhel, Fahad G Al-Harbi
Cureus.2022;[Epub] CrossRef - Incidence of Diabetic Ketoacidosis among Adults with Type 1 Diabetes in Saudi Arabia: Systematic review
Ayoub Ali Alshaikh, Rawan Zaifallh Alsalman, Nada Hamzah Albarqi, Razan Salem Alqahtani, Ali Ahmed Almontashri, Atheer Saud Alshahrani, Mohammed Abdullah Alshehri
Pharmacophore.2022; 13(4): 105. CrossRef - Features and long‐term outcomes of patients hospitalized for diabetic ketoacidosis
Michal Michaelis, Tzippy Shochat, Ilan Shimon, Amit Akirov
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Incidence, characteristics and long-term outcomes of patients with diabetic ketoacidosis: a prospective prognosis cohort study in an emergency department
Rachel Teixeira Leal Nunes, Carolina Frade Magalhães Girardin Pimentel Mota, Paulo Ricardo Gessolo Lins, Fernanda Salles Reis, Thais Castanheira de Freitas Resende, Ludmila de Andrade Barberino, Pedro Henrique Luiz da Silva, Aecio Flavio Teixeira de Gois
Sao Paulo Medical Journal.2021; 139(1): 10. CrossRef - Management of diabetic ketoacidosis in special populations
Mohsen S. Eledrisi, Salem A. Beshyah, Rayaz A. Malik
Diabetes Research and Clinical Practice.2021; 174: 108744. CrossRef - Profile of diabetic ketoacidosis at the National Diabetes and Endocrine Center in Tripoli, Libya, 2015
Aida Elkituni, Halla Elshwekh, Nesrein M. Bendala, Wafeya S. Atwear, Fawzia A. Aldaba, Abdulmunam M. Fellah
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(3): 771. CrossRef - Frequency of Diabetic Ketoacidosis and Its Determinants Among Pediatric Diabetes Mellitus Patients in Northwest Ethiopia
Atitegeb Abera Kidie, Ayenew Molla Lakew, Tiruneh Ayele
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4819. CrossRef - Diabetic ketoacidosis
Ketan K. Dhatariya, Nicole S. Glaser, Ethel Codner, Guillermo E. Umpierrez
Nature Reviews Disease Primers.2020;[Epub] CrossRef - Risk and Relevance of Insulin Pump Therapy in the Aetiology of Ketoacidosis in People with Type 1 Diabetes
Lena Christina Giessmann, Peter Herbert Kann
Experimental and Clinical Endocrinology & Diabetes.2020; 128(11): 745. CrossRef - Clinical and biochemical profile, precipitants and prognostic factors of diabetic ketoacidosis: A retrospective study from a tertiary care center of north India
Harpreet Singh, Atul Saroch, Ashok Kumar Pannu, H.J. Sachin, Navneet Sharma, Pinaki Dutta
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(4): 2357. CrossRef - Sudden death due to diabetic ketoacidosis following power failure of an insulin pump: Autopsy and pump data
Mette Louise Blouner Gram Kjærulff, Birgitte Schmidt Astrup
Journal of Forensic and Legal Medicine.2019; 63: 34. CrossRef - Defining and characterising diabetic ketoacidosis in adults
Ketan K. Dhatariya
Diabetes Research and Clinical Practice.2019; 155: 107797. CrossRef - Effects of diabetic ketoacidosis in the respiratory system
Alice Gallo de Moraes, Salim Surani
World Journal of Diabetes.2019; 10(1): 16. CrossRef - Increasing Hospitalizations for DKA: A Need for Prevention Programs
Priyathama Vellanki, Guillermo E. Umpierrez
Diabetes Care.2018; 41(9): 1839. CrossRef - Guidelines and controversies in the management of diabetic ketoacidosis – A mini-review
Tasnim Islam, Khalid Sherani, Salim Surani, Abhay Vakil
World Journal of Diabetes.2018; 9(12): 226. CrossRef - Closing the Mortality Gap in Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: Implications of a Clinical Decision Support App
Saperstein Y, Park J, McFarlane SI
International Journal of Clinical Endocrinology and Metabolism.2018; : 008. CrossRef - Incidence and prevalence of diabetic ketoacidosis (DKA) among adults with type 1 diabetes mellitus (T1D): a systematic literature review
Soulmaz Fazeli Farsani, Kimberly Brodovicz, Nima Soleymanlou, Jan Marquard, Erika Wissinger, Brett A Maiese
BMJ Open.2017; 7(7): e016587. CrossRef

 KES
KES

 PubReader
PubReader Cite
Cite