Effect of Vitamin D Supplementation on Risk of Fractures and Falls According to Dosage and Interval: A Meta-Analysis
Article information
Abstract
Background
Although recent studies comparing various dosages and intervals of vitamin D supplementation have been published, it is yet to be elucidated whether there is an appropriate dose or interval to provide benefit regarding fracture risk. We aimed to assess the published evidence available to date regarding the putative beneficial effects of vitamin D supplements on fractures and falls according to various dosages and intervals.
Methods
We performed a meta-analysis of randomized controlled studies reporting associations between vitamin D supplementation and the risks of fractures and falls in PubMed, EMBASE, and Cochrane library. Studies with supplements of ergocalciferol or calcitriol, those with a number of event ≤10, or those with a follow-up duration of less than 6 months were also excluded.
Results
Thirty-two studies were included in the final analysis. Vitamin D supplementation with daily dose of 800 to 1,000 mg was associated with lower risks of osteoporotic fracture and fall (pooled relative risk [RR], 0.87; 95% confidence interval [CI], 0.78 to 0.97 and RR, 0.91; 95% CI, 0.85 to 0.98), while studies with <800 or >1,000 mg/day did not. Also, among intervals, daily administration of vitamin D was associated with the reduced risk of falls, while intermittent dose was not. Also, patients with vitamin D deficiency showed a significant risk reduction of falls after vitamin D supplementation.
Conclusion
Daily vitamin D dose of 800 to 1,000 IU was the most probable way to reduce the fracture and fall risk. Further studies designed with various regimens and targeted vitamin D levels are required to elucidate the benefits of vitamin D supplements.
INTRODUCTION
Vitamin D has been known to be vital to musculoskeletal health since it promotes mineralization of osteoid tissue and supports calcium homeostasis and muscle function [1-3]. In previous studies, vitamin D deficiency was associated with low bone mineral density and increased fracture risk in longitudinal studies [4,5]. Vitamin D deficiency was also associated with decreased muscle mass and strength, supporting the potential benefits of vitamin D supplementation [2,4]. However, the optimal ways to administer vitamin D supplementation to prevent fractures have been debated until recently [6,7].
Contrary to expectations, the effect of vitamin D supplementation on fracture or fall risk was inconsistent or neutral, especially in the community-dwelling population [6]. In current guidelines, 800 IU/day of vitamin D with calcium supplementation has been recommended in older adults with vitamin D deficiency or those who are institutionalized [8,9]. Nonetheless, in a recent meta-analysis, treatment with vitamin D did not affect the incidence of fractures or falls among asymptomatic, community-dwelling populations with low vitamin D levels [6]. However, given that physicians have various options for vitamin D supplements in various doses, intervals, and oral/injectable forms, it is yet to be elucidated whether there is an appropriate dose or interval to benefit fracture risk. Subsequently, in a recent year, studies with various dosages and intervals have been published to address this question [7,10]. Since the dosage and interval of vitamin D supplementation are essential in assessing the effects on musculoskeletal outcomes, updated guidance on the optimal doses and dosing schedules for preventing fractures and falls is needed.
Therefore, the meta-analysis aimed to assess the published evidence available to date regarding the putative beneficial effects of vitamin D supplements on fractures and falls according to various dosages and intervals.
METHODS
Search strategy and study protocol
We searched PubMed, Embase, and Cochrane Library databases using keywords related to vitamin D supplementation with cholecalciferol, fractures, falls, and a randomized controlled study published until March 30, 2021. Peer Review of Electronic Search Strategies to design a structural search strategy were done (Supplemental Methods) [11]. Also, a manual search was conducted using study identifiers or references from previous studies. The systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12] and meta-analyses of observational studies in epidemiology [13]. The PRISMA checklist is available from Supplemental Table S1 [14], and the protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO ID 246065).
Study selection and data extraction
The studies were selected using the PRISMA flow diagram [12]. After removing duplicates, the titles and abstracts were screened to identify eligible studies for full-text review. Studies with ≤10 patients with fractures or falls were excluded because the calculations of mean and standard deviations (SDs) were considered unreliable in these studies. Studies comparing vitamin D supplements with placebo or vitamin D supplements of dose <400 IU/day were selected. The authors were contacted to provide organized results when data were not presented according to fracture or fall status. Studies using ergocalciferol or calcitriol or those with a follow-up duration of less than 6 months were also excluded. We collected article information from each study, including the authors’ details, study design, location, intervention, follow-up period, and study outcome. In addition, patient characteristics were collected, including sex, age, and study settings (community-based or institutionalized). In the subgroup analysis, studies were categorized according to a daily vitamin D dose of <800, 800 to 1,000, and >1,000 IU/day. In addition, according to the administration intervals, studies were categorized into daily and intermittent administration.
Statistical considerations and assessment of bias
Forest plots with a random-effects model were used to explore the baseline characteristics and impact of each variable on the critical outcome. I2 statistics were used to assess the heterogeneity [15]. The pooled relative risks (RRs) were calculated for fractures or falls. The 95% confidence intervals (CIs) were calculated for each pooled value and are presented in square brackets throughout the manuscript.
The process of study screening, data extraction, and assessment of quality and risk of bias were performed by two independent reviewers (S.H.K. and H.N.J.). Quality assessment was performed using the Cochrane Collaboration tool for assessing risk of bias. This scale contains several items (two items on selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases). Each item was judged as ‘low risk,’ high risk,’ or ‘unclear risk’ of bias. Inconsistent ratings between the two investigators were reached through discussion [16]. Egger’s regression tests were performed to assess publication bias [17].
Analyses were performed for the outcomes of all osteoporotic fractures, hip fractures, and falls in the overall population and in subgroups according to the dose and interval. The effects of vitamin D supplementation on the outcomes were assessed separately according to the dose and interval categories: <800, 800 to 1,000, >1,000 IU/day for dose, and daily, intermittent administration for an interval. Sensitivity analyses were performed among studies without any restrictions in patient selection to reduce the heterogeneity of the results. All statistical analyses were performed using Stata version 16 (Stata statistical software: Release 16, StataCorp., College Station, TX, USA).
RESULTS
Study characteristics
The initial search yielded 3,861 studies, which were narrowed down to 2,254 studies after duplicate removal. After screening, 1,970 studies were removed, and 284 articles were assessed using a full-text review. After removing 251 non-relevant studies, our systematic review included 32 studies (Fig. 1). The complete list and characteristics of the included studies are listed in Table 1 [7,10,18-47].
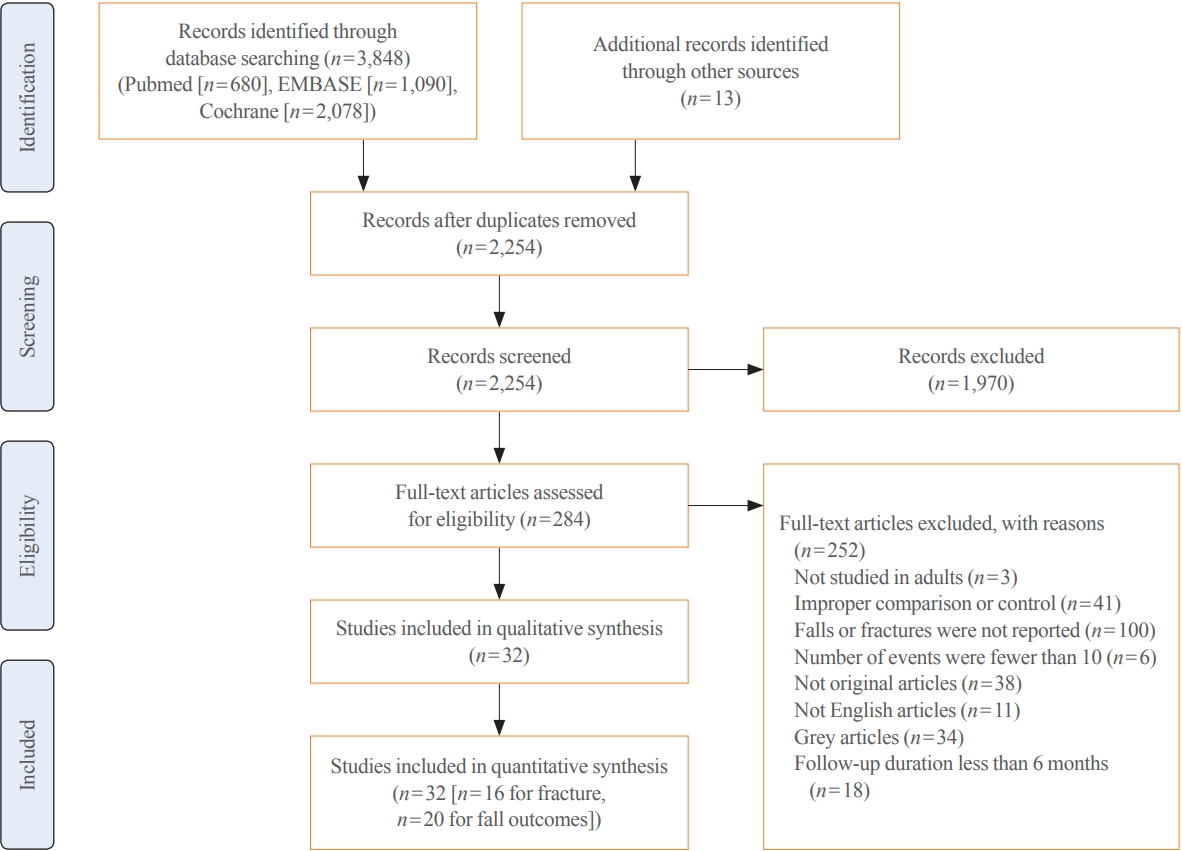
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) diagram of study selection.

Study Characteristics of Randomized Controlled Trials Reporting Effects of Vitamin D Treatment on Risk of Fractures and Falls
The 32 studies included 104,363 patients, with a median of 3,162 patients per study (range, 46 to 36,282). The studies were conducted in Europe (n=18), North America (n=10), Australasia (n=3), and Asia (n=1). Among them, 16 and 20 studies reported fractures and falls as outcomes, and 10 reported hip fractures. The median daily dose of cholecalciferol was 800 IU/day, and eight studies reported <800 IU/day, 15 studies reported 800 to 1,000 IU/day, and nine studies reported >1,000 IU/day. Regarding the interval, 26 studies reported daily administration, while six reported intermittent cholecalciferol administration. The median follow-up duration was 24 months (range, 9 to 120), and the median age was 72 years (range, 53 to 85). Most studies included women (32 [96.9%] studies), with 75% of participants (range, 15% to 100%) (Table 1).
Effect of vitamin D supplementation on risk of fractures and falls
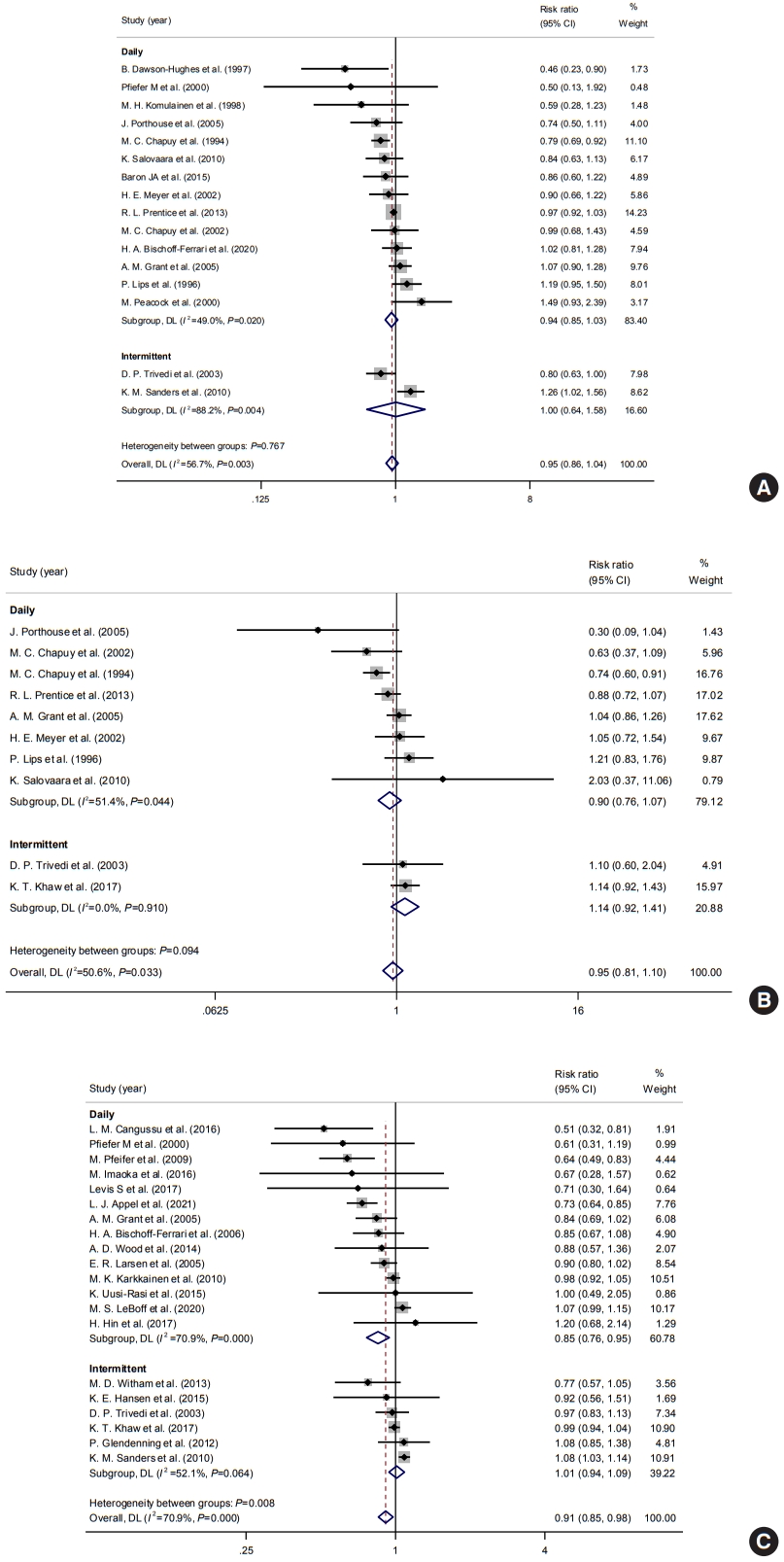
Among the 32 studies, 16, 10, and 20 studies reported the risk of osteoporotic, hip fracture, and fall as outcomes. In terms of fractures, of 67,570 participants, 7,107 and 1,663 suffered osteoporotic and hip fractures, respectively. A meta-analysis of 16 studies revealed that vitamin D supplementation was not associated with a risk of osteoporotic fracture (pooled RR, 0.95; 95% CI, 0.86 to 1.04; I2=56.7%) (Fig. 2A). Although some studies published in the late 1990s reported preventive effects of vitamin D supplementation on the risk of fractures, most studies reported neutral effects, which were statistically insignificant overall. In a subgroup analysis, 10 studies reported hip fracture as an outcome. The pooled RR was 0.95 (95% CI, 0.81 to 1.10; I2=50.6%) (Fig. 2B). In terms of falls, 11,396 patients experienced falls during the follow-up. A meta-analysis of 21 studies showed that vitamin D supplementation was associated with a reduced risk of falls (pooled RR, 0.91; 95% CI, 0.85 to 0.98; I2=70.9%) (Fig. 2C). However, there was substantial evidence for heterogeneity in previous analyses, mainly due to different magnitudes of risk and follow-up duration across studies.
Effects according to the daily dose of vitamin D supplementation
Subgroup analyses according to the daily dose of vitamin D supplementation were performed to improve the heterogeneity and determine the impact of dosage. The daily dose of 800 to 1,000 IU/day of vitamin D supplement was associated with a decreased fracture risk with a pooled RR of 0.87 (95% CI, 0.78 to 0.97; I2=23.5%), while vitamin D doses <800 and >1,000 IU/day were not associated with fracture risks (<800 IU/day: pooled RR, 0.97, 95% CI, 0.80 to 1.18; I2=61.7%; >1,000 IU/day: pooled RR, 1.14; 95% CI, 0.93 to 1.41; I2=44.1%) (Fig. 3A). In a subgroup analysis of hip fractures, vitamin D doses <800 and 800–1,000 IU/day were not significantly associated with the risk of hip fracture (<800 IU/day: pooled RR, 0.98; 95% CI, 0.81 to 1.19; I2=20.1%; 800–1,000 IU/day: pooled RR, 0.84; 95% CI, 0.64 to 1.10; I2=56.5%) (Fig. 3B).
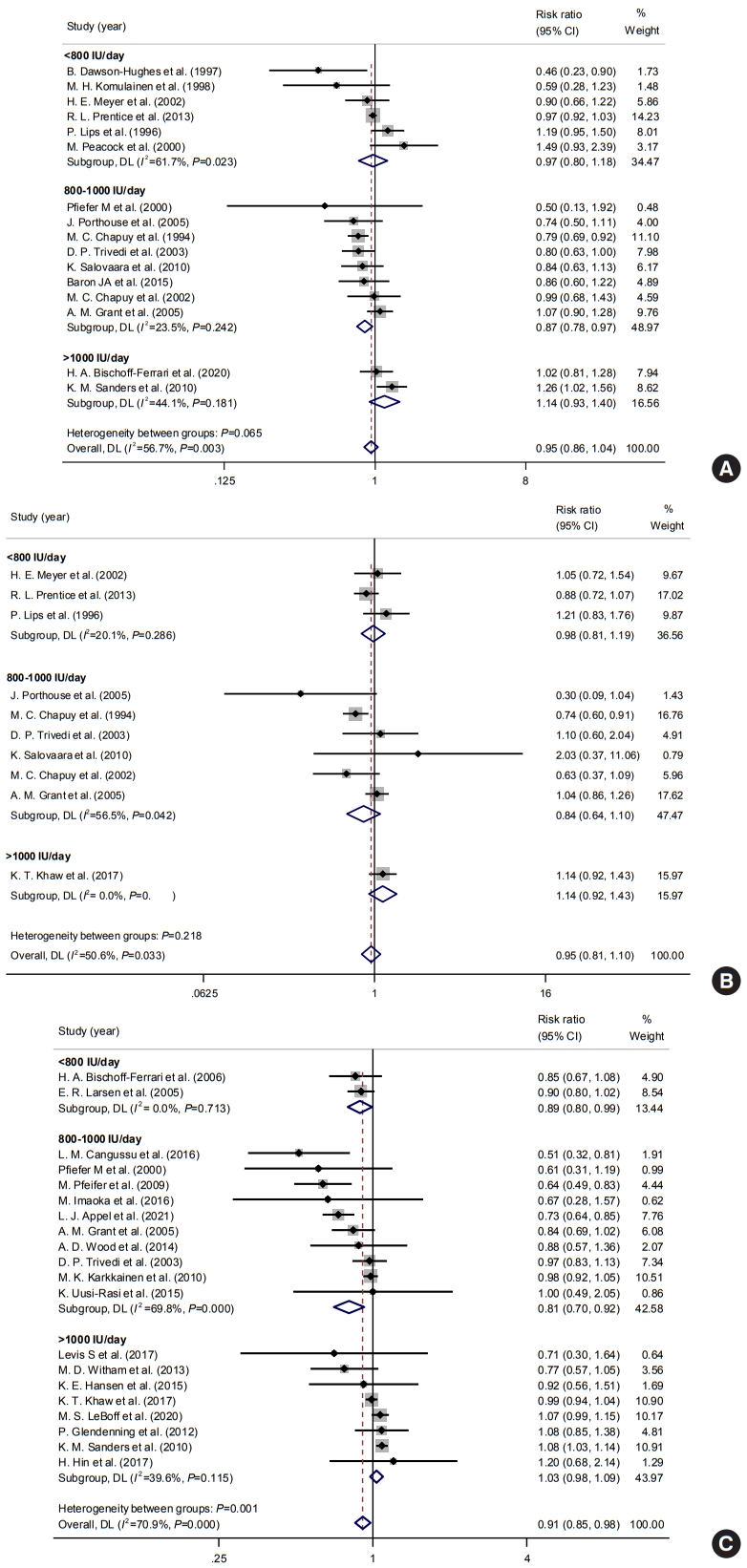
Impacts of vitamin D supplements on the risks of (A) any osteoporotic, (B) hip fracture, and (C) fall according to daily dosages. CI, confidence interval.
Regarding falls, both <800 and 800–1,000 IU/day of vitamin D supplements showed a protective effect on the risk of falls (pooled RR, 0.89; 95% CI, 0.80 to 1.00; I2=0% and pooled RR, 0.81; 95% CI, 0.70 to 0.92; I 2=69.8%) (Fig. 3C). Besides, >1,000 IU/day of vitamin D supplements was not associated with the risk of falls.
Effects according to administration intervals of vitamin D supplementation
Subgroup analyses were performed according to the intervals of vitamin D supplementation to determine the impact of the gap between administration. Subgroups were divided into two groups: daily and intermittent administration. The interval of administration was not significantly associated with the risk of osteoporotic fractures (daily: pooled RR, 0.94; 95% CI, 0.85 to 1.03; I2=49.0%; intermittent: pooled RR, 1.00; 95% CI, 0.64 to 1.58; I2=88.2%) (Fig. 4A). Intervals were not significantly associated with the risk of hip fractures also (Fig. 4B). However, daily administration of vitamin D supplementation was significantly associated with a reduced risk of falls (daily: pooled RR, 0.85; 95% CI, 0.76 to 0.95; I2=70.9%; intermittent: pooled RR, 1.01; 95% CI, 0.94 to 1.09; I2=52.1%) (Fig. 4C).
Effects according to calcium supplements and patient characteristics
In a subgroup analysis regarding calcium supplementation, studies of calcium/vitamin D supplementation were associated with a significant risk reduction of falls, while risks of any osteoporotic fractures and hip fractures were not. (Fig. 5). Also, among studies with baseline vitamin D levels (n=23), vitamin D supplements were significantly related to reduced risks of falls in patients with vitamin D deficiency at their baseline.

Impacts of vitamin D supplements on the risks of any osteoporotic, hip fracture, and fall according to combined calcium supplementation and baseline vitamin D level. CI, confidence interval.
Additionally, according to calcium supplementation, a subgroup analysis within the 800 to 1,000 IU/day group was done (Fig. 6). About fracture risk, studies with calcium/vitamin D supplementation showed significant risk reduction within 800-1,000 IU/day (pooled RR, 0.88; 95% CI, 0.78 to 1.00). On the other hand, the risk of fall was significantly reduced in both types of studies with both vitamin D only and calcium/vitamin D supplementation (vitamin D only: RR, 0.80; 95% CI, 0.65 to 0.97; calcium/vitamin D supplementation: RR, 0.81; 95% CI, 0.65 to 0.99). Also, in subgroup analysis according to institutionalized state, there was a significant reduction in the risk of falls in community-dwelling patients, while study numbers were insufficient to determine for institutionalized patients (Fig. 7).

Impacts of 800 to 1,000 IU/day of vitamin D supplements on the risks of (A) osteoporotic fracture and (B) fall according to combined calcium supplementation. CI, confidence interval.

Impacts of vitamin D supplements on the risks of (A) osteoporotic fracture and (B) fall according to institutionalized and communitydwelling populations. CI, confidence interval.
In meta-regression analysis, baseline vitamin D level, age, percentage of women among study participants, and follow-up duration were insignificantly correlated with risk of any osteoporotic fracture (Supplemental Fig. S1), hip fracture (Supplemental Fig. S2), and fall (Supplemental Fig. S3).
Assessment of study quality and publication bias
Most studies at least partly met the quality standards of each area, while others did not. Among the 32 studies, five did not blind the participants and personnel, three did not adequately blind the outcome assessment, and five received funds from pharmaceuticals, which may cause reporting bias (Supplemental Fig. S4). Overall, there were concerns with quality in the four studies. Regarding publication bias, none of the studies showed significant publication bias in assessing risks of any osteoporotic, hip fractures, and falls (Supplemental Fig. S5).
DISCUSSION
The present meta-analysis included up-to-date randomized controlled trials (RCTs) with more than 100,000 patients to summarize the effect of vitamin D supplements on the risk of fractures and falls, according to different dosages and intervals. The analysis showed that vitamin D supplementation was associated with the reduced risk of fall, but not with fracture. However, vitamin D dose of 800 to 1,000 IU/day was associated with a 13% and 19% lower risk of fractures and falls, respectively. Also, daily administration of vitamin D was associated with decreased risk of falls, while intermittent administration was not. In patients with vitamin D deficiency, vitamin D supplementation showed a substantially reduced risk of falls. Correlations of participants’ age, sex, baseline vitamin D level, and follow-up duration with the risk of any osteoporotic, hip, and fall were all insignificant.
Consistent with previous meta-analyses [48], vitamin D supplementation showed a significant association with the risk of falls. It was also in agreement with a meta-analysis by Murad et al. [49] that vitamin D with calcium supplementation was related to the fall lowering effect. However, Bolland et al. [50] and US Preventive Services Task Force recommendation reported an insignificant association between vitamin D supplementation and fall [50-52]. The discrepancy among studies could be mainly due to the heterogeneity of study characteristics, such as various ways of vitamin D administration, insufficient number of participants, and short follow-up duration. From our analysis, including only studies with sufficient follow-up duration and event numbers, vitamin D3 could help reduce fall events. One of the feasible reasons for the effect of vitamin D on fall prevention is that vitamin D supplementation may help affect muscle strength, which could reduce body sway [18,53].
Regarding fracture outcome, it was also consistent with previous studies that vitamin D supplementation was not associated with the risk of fractures [6,48,54]. However, it has been suggested that some studies with negative results may not have enough events or follow-up duration to observe a meaningful difference [18,48]. In a recent meta-analysis, only a subgroup of follow-up duration >12 months showed a significant protective effect of vitamin D supplements on fracture risk [48], implying that the studies with enough follow-up duration can yield significant results. Also, there are some RCTs assessing very high annual doses of vitamin D that showed an increased risk of fractures and falls in participants who received vitamin D [19,55]. Various designs and administration methods of vitamin D may confuse and attenuate the final result, even though we excluded studies with short duration and small event numbers [6,48,54]. In addition, fragility fractures are complex events that many factors contribute simultaneously, such as physical activity, balancing ability, and especially, bone density [56,57]. Therefore, although efforts were made to include selected studies, vitamin D supplementation alone may not result in a significant difference in fracture outcome.
To overcome the pitfalls of heterogeneity and find the best way to replace vitamin D, subgroup analyses according to different dosages were performed. Vitamin D supplements of 800 to 1,000 IU/day reduced the risk of osteoporotic fractures and falls with low heterogeneity. These results are consistent with previous findings that a moderate dose of vitamin D supplements may help reduce fracture and fall risk [20-22,58]. It is notable that many previous studies involving vitamin D supplements of 800 to 1,000 IU/day are based on the institutionalized population [20,21]. However, only a few studies were based on institutionalized patients in this analysis [20,21], mainly because most previous studies had a short follow-up duration and a small number of participants, making the main population of the study community-dwelling. Therefore, the result implies that community-dwelling patients may also benefit from taking vitamin D. Interestingly, subgroup analysis of the calculated daily dose >1,000 IU showed a trend of increased risk of fractures and falls, although it was insignificant. A recent study by Bolland et al. [50] showed similar results, along with other meta-analyses [59,60], that intermittent vitamin D supplements raised fall risks. Although the reasons are not clear, intermittent supplements are usually given in high doses that are suspected to be the cause of increased fractures and falls. Some studies suggested the U-shaped association between vitamin D and risk of fractures and falls, which could be mediated via the vitamin D receptor in the central nervous system [59,60]. Also, as the half-life of 25-hydroxyvitamin D (25(OH)D) is approximately 15 days, monthly or yearly intervals are likely to cause fluctuations that may lead to toxic levels of 25(OH)D in the blood [19,22,60]. To summarize, a moderate dose of 800 to 1,000 IU and daily administration of vitamin D can be beneficial in preventing osteoporotic fractures and falls in the general population.
In addition, patients who had vitamin D deficiency at their baseline could benefit from vitamin D supplements, which showed a 22% reduction in the risk of fall in our data. The results could be partly explained by previous studies that vitamin D supplementation improved functional outcomes, such as lower limb strength and balance in elderly patients with vitamin D deficiency [61]. Besides, in association analysis, vitamin D level, calcium supplementation, age, the proportion of women, and follow-up duration were not associated with the risk of fractures or falls. However, it could be due to the high heterogeneity of included studies in the association analysis. Especially, baseline vitamin D levels were presented in only nine studies, which may mislead the result of linear association, unlike subgroup analysis. More studies are needed to conclude that age and additional calcium supplementation affect the risk of fractures and falls during vitamin D supplementation.
Overall, the key to the success of trials of vitamin D supplements could be the study design to achieve targeted 25(OH)D levels in the selected population. As there is a strong correlation between baseline vitamin D level and bone mineral density [4,5], muscle mass, and function [2], the inconsistent results in the RCTs can be largely influenced by subject selection and vitamin D concentration at the baseline. Also, 25(OH)D levels reached with the fixed doses can vary greatly. Further trials with a design targeting optimal levels with flexible dosages in a selected population are required.
This study has several strengths. As there was a need for integrated updated meta-analysis due to recently published RCTs [7,10,25], our analysis has its strength in integrating the recent results until March 2021. Also, the study confirmed previous knowledge and revealed some novel findings. We found a significantly decreased risk of fractures and falls with vitamin D supplements of 800 to 1,000 IU/day. Also, as intervals of vitamin D supplementation were separately analyzed, the results from subgroup analyses may help determine the dosage and intervals of vitamin D supplementation in clinical practice. The updated meta-analysis differs from previous meta-analyses [50,54] in that it excluded RCTs with short follow-up durations (i.e., <6 months) or those including few fracture events (i.e., <10 events) to minimize the risks of bias. Also, studies regarding ergocalciferol were not included in the analysis to reduce the heterogeneity of studies.
This study also has some limitations. First, only a few studies selected for the review were conducted on institutionalized patients due to the limitation of follow-up duration and number of events. However, it may help reduce the heterogeneity of analysis that studies focusing on specific clinical conditions to evaluate the treatment of vitamin D deficiency to improve the disease or symptoms were excluded from the analysis. Most of the studies were mainly on community-dwelling populations. Second, residual heterogeneity was observed in some subgroup analyses. The residual extent of heterogeneity may be partially explained by differences in age distribution, underlying diseases, or nutritional status among the studies.
Our meta-analyses summarized the effects of vitamin D supplements at different dosages and intervals on the risk of fractures and falls. Among the various administration methods, only a daily dose of 800 to 1,000 IU may reduce the risk of osteoporotic fractures and falls. We also identified that a daily interval of vitamin D supplementation could help reduce the risk of falls. Also, vitamin D deficient patients were more likely to benefit from vitamin D supplementation by reducing the risk of falls. To summarize, consistent with previous recommendations, a daily vitamin D dose of 800 to 1,000 IU was the most probable way to reduce the fracture and fall risk. As it is not possible that one regimen suits all, further studies with various regimens targeting vitamin D levels are required to elucidate the benefits of vitamin D supplements.
Supplementary Information
PRISMA-S Checklist
Meta-regression plot of risk of osteoporotic fractures with (A) baseline vitamin D level, (B) age, (C) percentage of women, and (D) follow-up duration. CI, confidence interval.
Meta-regression plot of risk of hip fractures with (A) baseline vitamin D level, (B) age, (C) percentage of women, and (D) follow-up duration. CI, confidence interval.
Meta-regression plot of risk of fall with (A) baseline vitamin D level, (B) age, (C) percentage of women, and (D) follow-up duration. CI, confidence interval.
Diagram of publication bias.
Funnel plots of the risks of (A) any osteoporotic, (B) hip fracture, and (C) fall.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: S.H.K., C.S.S. Acquisition, analysis, or interpretation of data: S.H.K., H.N.J. Drafting the work or revising: S.H.K. Final approval of the manuscript: S.H.K., H.N.J., J.H.K., S.W.K., C.S.S.