Search
- Page Path
- HOME > Search
- Thyroid
Thyroid Cancer Screening - Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
- Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
- Endocrinol Metab. 2024;39(2):310-323. Published online April 9, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1870
- 1,047 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
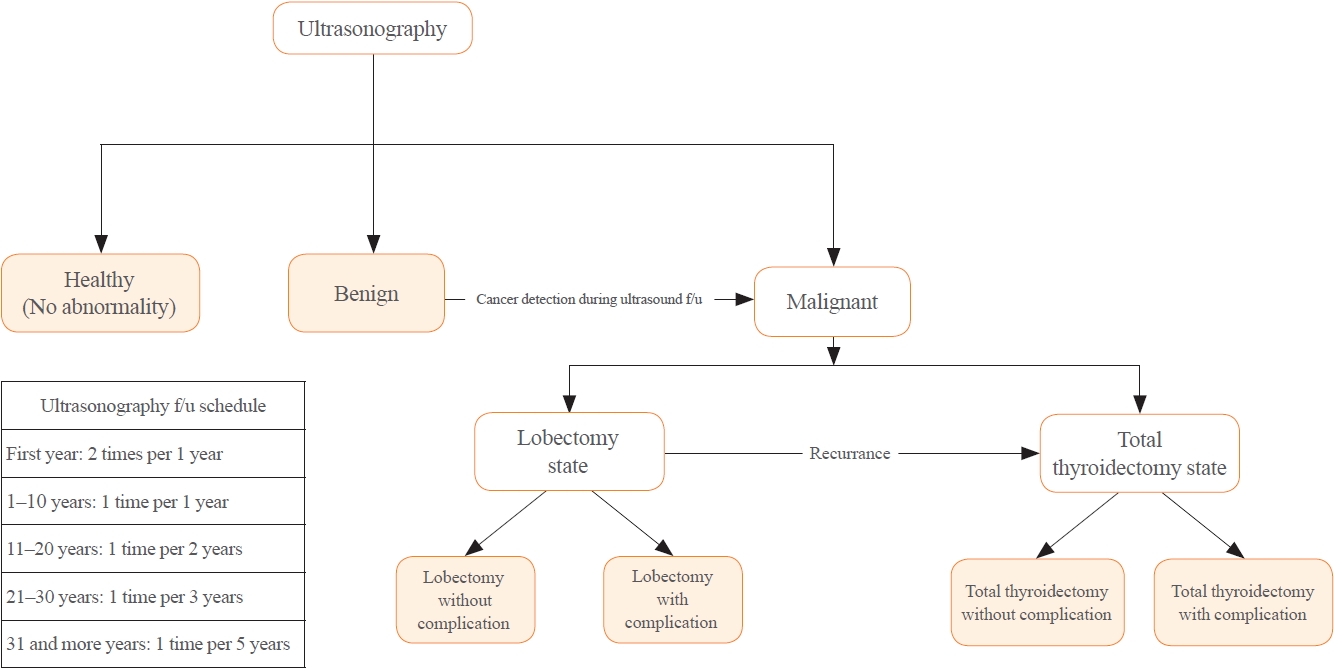
There is debate about ultrasonography screening for thyroid cancer and its cost-effectiveness. This study aimed to evaluate the cost-effectiveness of early screening (ES) versus symptomatic detection (SD) for differentiated thyroid cancer (DTC) in Korea.
Methods
A Markov decision analysis model was constructed to compare the cost-effectiveness of ES and SD. The model considered direct medical costs, health outcomes, and different diagnostic and treatment pathways. Input data were derived from literature and Korean population studies. Incremental cost-effectiveness ratio (ICER) was calculated. Willingness-to-pay (WTP) threshold was set at USD 100,000 or 20,000 per quality-adjusted life year (QALY) gained. Sensitivity analyses were conducted to address uncertainties of the model’s variables.
Results
In a base case scenario with 50 years of follow-up, ES was found to be cost-effective compared to SD, with an ICER of $2,852 per QALY. With WTP set at $100,000, in the case with follow-up less than 10 years, the SD was cost-effective. Sensitivity analysis showed that variables such as lobectomy probability, age, mortality, and utility scores significantly influenced the ICER. Despite variations in costs and other factors, all ICER values remained below the WTP threshold.
Conclusion
Findings of this study indicate that ES is a cost-effective strategy for DTC screening in the Korean medical system. Early detection and subsequent lobectomy contribute to the cost-effectiveness of ES, while SD at an advanced stage makes ES more cost-effective. Expected follow-up duration should be considered to determine an optimal strategy for DTC screening.

- Thyroid
- Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
- Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2024;39(1):152-163. Published online January 22, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1794
- 1,236 View
- 44 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
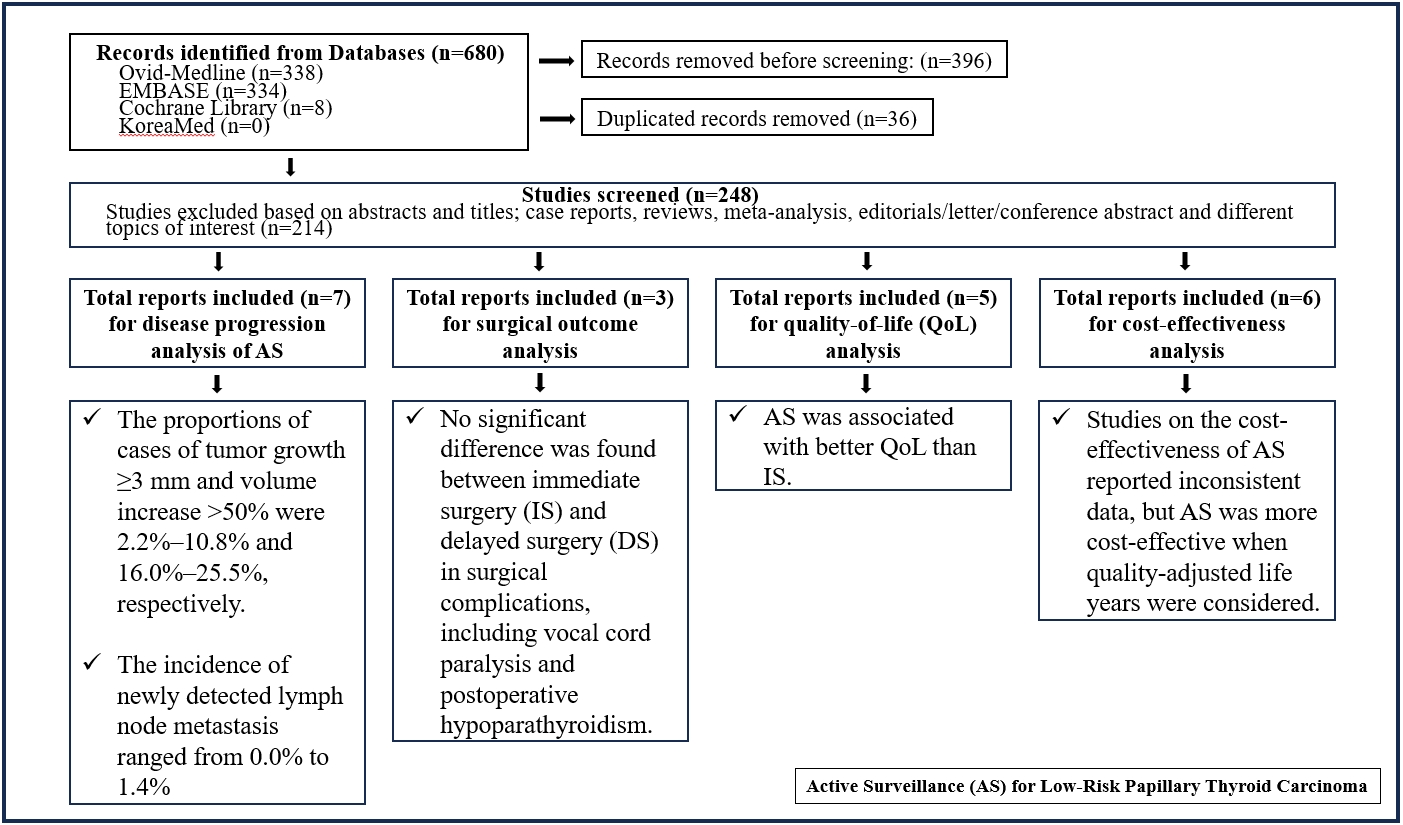
Active surveillance (AS) has been introduced as a management strategy for low-risk papillary thyroid carcinoma (PTC) due to its typically indolent nature. Despite this, the widespread adoption of AS has encountered several challenges. The aim of this systematic review was to evaluate the safety of AS related to disease progression and its benefits compared with immediate surgery (IS).
Methods
Studies related to AS in patients with low-risk PTC were searched through the Ovid MEDLINE, Embase, Cochrane Library, and KoreaMed databases. Studies on disease progression, surgical complication, quality of life (QoL), and cost-effectiveness were separately analyzed and narratively synthesized.
Results
In the evaluation of disease progression, the proportions of cases with tumor growth ≥3 mm and a volume increase >50% were 2.2%–10.8% and 16.0%–25.5%, respectively. Newly detected lymph node metastasis was identified in 0.0%–1.4% of patients. No significant difference was found between IS and delayed surgery in surgical complications, including vocal cord paralysis and postoperative hypoparathyroidism. AS was associated with better QoL than IS. Studies on the cost-effectiveness of AS reported inconsistent data, but AS was more cost-effective when quality-adjusted life years were considered.
Conclusion
AS is an acceptable management option for patients with low-risk PTC based on the low rate of disease progression and the absence of an increased mortality risk. AS has additional benefits, including improved QoL and greater QoL-based cost-effectiveness. -
Citations
Citations to this article as recorded by- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef
- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
- Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
- Endocrinol Metab. 2022;37(5):759-769. Published online October 5, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1515
- 3,229 View
- 192 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
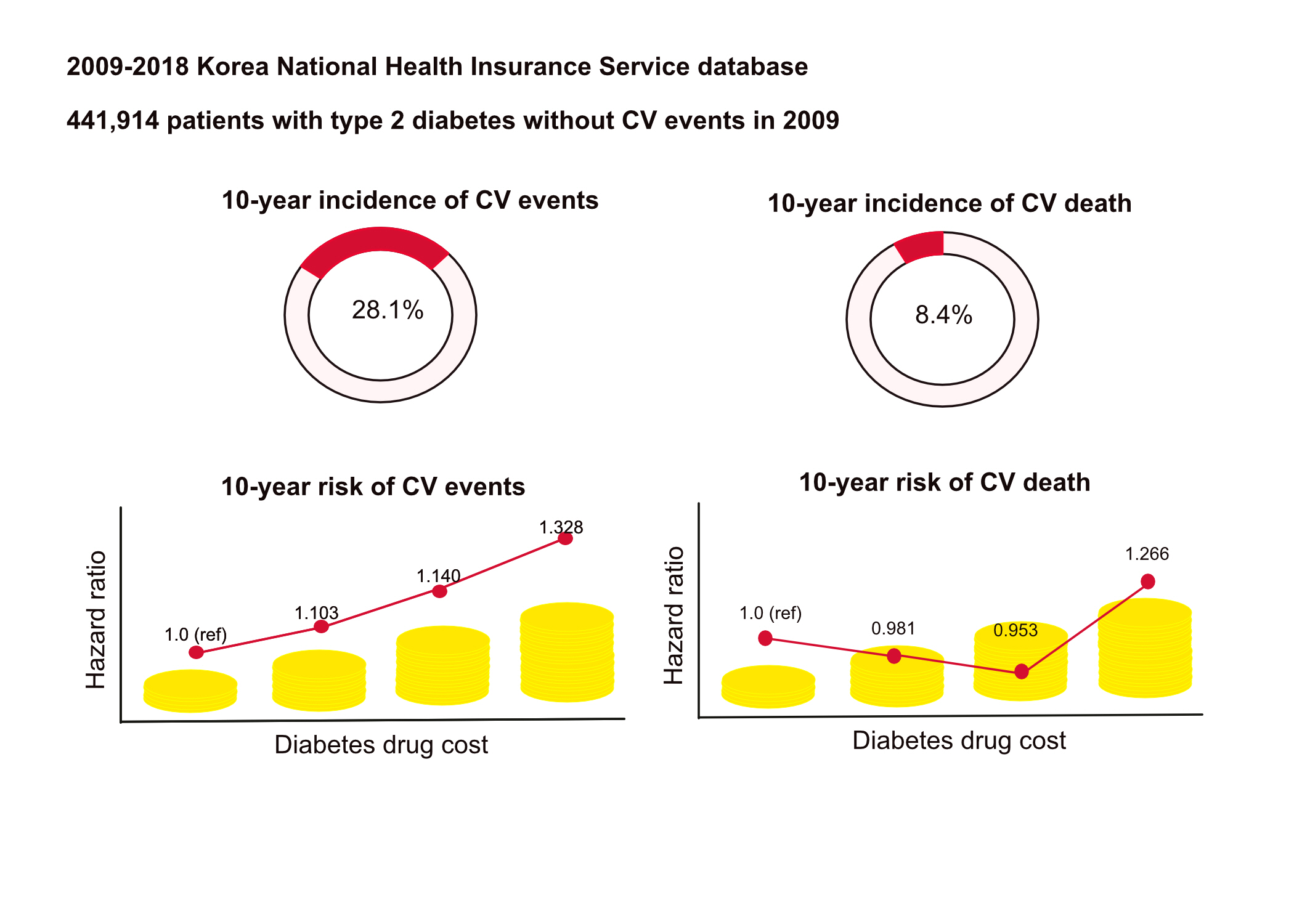
This study aimed to investigate the long-term effects of diabetes drug costs on cardiovascular (CV) events and death.
Methods
This retrospective observational study used data from 2009 to 2018 from the National Health Insurance in Korea. Among the patients with type 2 diabetes, those taking antidiabetic drugs and who did not have CV events until 2009 were included. Patients were divided into quartiles (Q1 [lowest]–4 [highest]) according to the 2009 diabetes drug cost. In addition, the 10-year incidences of CV events (non-fatal myocardial infarction, stroke, hospitalization for heart failure, and coronary revascularization) and CV death (death due to CV events) were analyzed.
Results
A total of 441,914 participants were enrolled (median age, 60 years; men, 57%). CV events and death occurred in 28.1% and 8.36% of the patients, respectively. The 10-year incidences of CV events and deaths increased from Q1 to 4. After adjusting for sex, age, income, type of diabetes drugs, comorbidities, and smoking and drinking status, the risk of CV events significantly increased according to the sequential order of the cost quartiles. In contrast, the risk of CV death showed a U-shaped pattern, which was the lowest in Q3 (hazard ratio [HR], 0.953; 95% confidence interval [CI], 0.913 to 0.995) and the highest in Q4 (HR, 1.266; 95% CI, 1.213 to 1.321).
Conclusion
Diabetes drug expenditure affects 10-year CV events and mortality. Therefore, affording an appropriate diabetes drug cost at a similar risk of CV is an independent protective factor against CV death. -
Citations
Citations to this article as recorded by- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef
- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study

- Thyroid
- The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
- Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
- Endocrinol Metab. 2021;36(4):725-736. Published online August 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1164
- 4,400 View
- 147 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
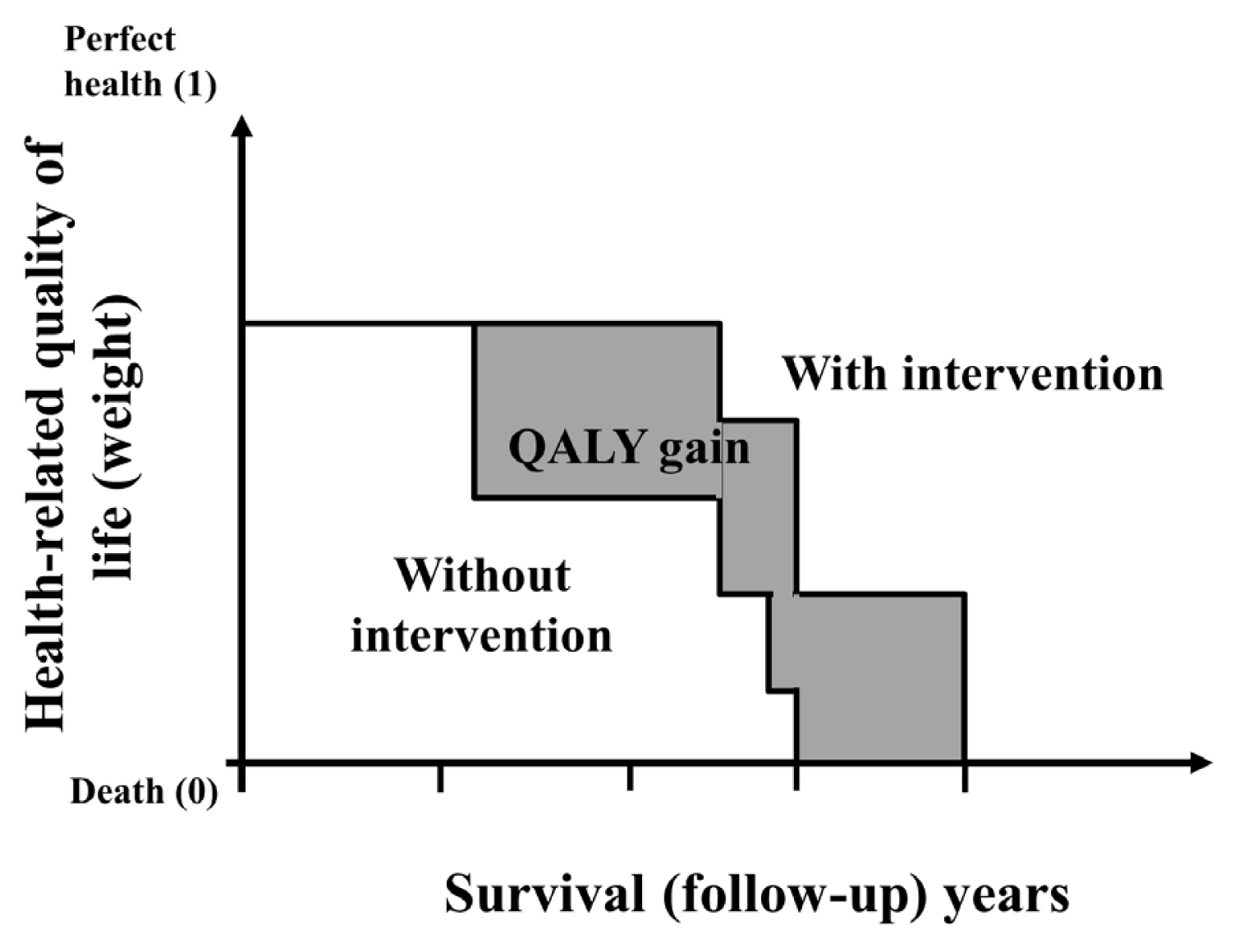
ePub - Economic evaluation is a type of comparative analysis between interventions in terms of both their resource use and health outcomes. Due to the good prognosis of thyroid cancer (TC), the socioeconomic burden of TC patients post-diagnosis is increasing. Therefore, economic evaluation studies focusing on TC are recommended. This study aimed to describe the concept and methods of economic evaluation and reviewed previous TC studies. Several previous studies compared the costs of interventions or evaluated recurrence, complications, or quality of life as measures of their effectiveness. Regarding costs, most studies focused on direct costs and applied hypothetical models. Cost-minimization analysis should be distinguished from simple cost analysis. Furthermore, due to the universality of the term “cost-effectiveness analysis” (CEA), several studies have not distinguished CEA from cost-utility analysis; this point needs to be considered in future research. Cost-benefit analyses have not been conducted in previous TC research. Since TC has a high survival rate and good prognosis, the need for economic evaluations has recently been pointed out. Therefore, correct concepts and methods are needed to obtain clear economic evaluation results. On this basis, it will be possible to provide appropriate guidelines for TC treatment and management in the future.
-
Citations
Citations to this article as recorded by- Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
Endocrinology and Metabolism.2024; 39(2): 310. CrossRef - Role of Prehabilitation and Rehabilitation on Functional Recovery and Quality of Life in Thyroid Cancer Patients: A Comprehensive Review
Lorenzo Lippi, Alessio Turco, Stefano Moalli, Marco Gallo, Claudio Curci, Antonio Maconi, Alessandro de Sire, Marco Invernizzi
Cancers.2023; 15(18): 4502. CrossRef - Sex-specific Associations between Body Mass Index and Thyroid Cancer Incidence among Korean Adults
Kyoung-Nam Kim, Kyungsik Kim, Sangjun Lee, Sue K. Park
Cancer Epidemiology, Biomarkers & Prevention.2023; 32(9): 1227. CrossRef - Active Surveillance Versus Immediate Surgery for Low-Risk Papillary Thyroid Microcarcinoma Patients in South Korea: A Cost-Minimization Analysis from the MAeSTro Study
Kyungsik Kim, June Young Choi, Su-jin Kim, Eun Kyung Lee, Young Ki Lee, Jun Sun Ryu, Kyu Eun Lee, Jae Hoon Moon, Young Joo Park, Sun Wook Cho, Sue K. Park
Thyroid.2022; 32(6): 648. CrossRef - A Systematic Review of Economic Evaluation of Thyroid Cancer
Mijin Kim, Woojin Lim, Kyungsik Kim, Ja Seong Bae, Byung Joo Lee, Bon Seok Koo, Eun Kyung Lee, Eu Jeong Ku, June Young Choi, Bo Hyun Kim, Sue K. Park
International Journal of Thyroidology.2022; 15(2): 74. CrossRef
- Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population

- Clinical Study
- Economic Evaluation of Recombinant Human Thyroid Stimulating Hormone Stimulation vs. Thyroid Hormone Withdrawal Prior to Radioiodine Ablation for Thyroid Cancer: The Korean Perspective
- Seo Young Sohn, Hye Won Jang, Yoon Young Cho, Sun Wook Kim, Jae Hoon Chung
- Endocrinol Metab. 2015;30(4):531-542. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.531
- 3,556 View
- 43 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Previous studies have suggested that recombinant human thyroid stimulating hormone (rhTSH) stimulation is an acceptable alternative to thyroid hormone withdrawal (THW) when radioiodine remnant ablation is planned for thyroid cancer treatment, based on superior short-term quality of life with non-inferior remnant ablation efficacy. This study evaluated the cost-effectiveness of radioiodine remnant ablation using rhTSH, compared with the traditional preparation method which renders patients hypothyroid by THW, in Korean perspective.
Methods This economic evaluation considered the costs and benefits to the Korean public healthcare system. Clinical experts were surveyed regarding the current practice of radioiodine ablation in Korea and their responses helped inform assumptions used in a cost effectiveness model. Markov modelling with 17 weekly cycles was used to assess the incremental costs per quality-adjusted life year (QALY) associated with rhTSH. Clinical inputs were based on a multi-center, randomized controlled trial comparing remnant ablation success after rhTSH preparation with THW. The additional costs associated with rhTSH were considered relative to the clinical benefits and cost offsets.
Results The additional benefits of rhTSH (0.036 QALY) are achieved with an additional cost of Korean won ₩961,105, equating to cost per QALY of ₩26,697,361. Sensitivity analyses had only a modest impact upon cost-effectiveness, with one-way sensitivity results of approximately ₩33,000,000/QALY.
Conclusion The use of rhTSH is a cost-effective alternative to endogenous hypothyroid stimulation prior to radioiodine ablation for patients who have undergone thyroidectomy in Korea.
-
Citations
Citations to this article as recorded by- Comparison of Recombinant Human Thyroid-Stimulating Hormone and Thyroid Hormone Withdrawal for 131I Therapy in Patients With Intermediate- to High-Risk Thyroid Cancer
Sohyun Park, Ji-In Bang, Keunyoung Kim, Youngduk Seo, Ari Chong, Chae Moon Hong, Dong-Eun Lee, Miyoung Choi, Sang-Woo Lee, So Won Oh
Clinical Nuclear Medicine.2024; 49(3): e96. CrossRef - Thyroid Hormone Withdrawal versus Recombinant Human TSH as Preparation for I-131 Therapy in Patients with Metastatic Thyroid Cancer: A Systematic Review and Meta-Analysis
Luca Giovanella, Maria Luisa Garo, Alfredo Campenní, Petra Petranović Ovčariček, Rainer Görges
Cancers.2023; 15(9): 2510. CrossRef - Health-related quality of life of thyroid cancer patients undergoing radioiodine therapy: a cohort real-world study in a reference public cancer hospital in Brazil
Jayda Eiras Ramim, Marcella Araugio Soares Cardoso, Gessen Lopes Carneiro de Oliveira, Maria Luisa Gomes, Tiago Teixeira Guimarães, Rossana Corbo Ramalho de Mello, Anke Bergmann, Priscilla Brunelli Pujatti
Supportive Care in Cancer.2020; 28(8): 3771. CrossRef - Predictive factors determining incomplete response to radioiodine therapy in patients with differentiated thyroid cancer
Ewelina Szczepanek-Parulska, Magdalena Wojewoda-Korbelak, Martyna Borowczyk, Malgorzata Kaluzna, Barbara Brominska, Katarzyna Ziemnicka, Rafal Czepczynski, Maciej Baczyk, Marek Ruchala
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2020;[Epub] CrossRef - Initial Adoption of Recombinant Human Thyroid-Stimulating Hormone Following Thyroidectomy in the Medicare Thyroid Cancer Patient Population
Michaela A. Dinan, Yanhong Li, Shelby D. Reed, Julie Ann Sosa
Endocrine Practice.2019; 25(1): 31. CrossRef - Triennial Report ofEndocrinology and Metabolism, 2015 to 2017
Eun-Jung Rhee, Hey Yeon Jang, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 195. CrossRef - Recombinant human TSH stimulated thyroglobulin levels at remnant ablation predict structural incomplete response to treatment in patients with differentiated thyroid cancer
Jeonghoon Ha, Min Hee Kim, Kwanhoon Jo, Yejee Lim, Ja Seong Bae, Sohee Lee, Moo Il Kang, Bong Yun Cha, Dong Jun Lim
Medicine.2017; 96(29): e7512. CrossRef - Does the Risk of Metabolic Syndrome Increase in Thyroid Cancer Survivors?
Min-Hee Kim, Jin-young Huh, Dong-jun Lim, Moo-Il Kang
Thyroid.2017; 27(7): 936. CrossRef
- Comparison of Recombinant Human Thyroid-Stimulating Hormone and Thyroid Hormone Withdrawal for 131I Therapy in Patients With Intermediate- to High-Risk Thyroid Cancer

- Thyroid
- Cost-of-Illness Trends Associated with Thyroid Disease in Korea
- Kyung-Rae Hyun, Sungwook Kang, Sunmi Lee
- Endocrinol Metab. 2014;29(3):257-269. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.257
- 3,757 View
- 30 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study is to analyze the scale of and trends associated with the cost-of-illness of thyroid disease in Korea at 2-year intervals during the last 10 years for which data are available.
Methods Cost-of-illness was estimated in terms of direct and indirect costs. Direct costs include direct medical costs due to hospitalization, outpatient and pharmacy sectors, transportation, and care-giver costs. Indirect costs include future income loss due to premature death and loss of productivity as a result of absence from work.
Results The cost-of-illness of thyroid disease in Korea was estimated at 224.2 billion won in 2002, 303.4 billion won in 2004, 400.3 billion won in 2006, 570.4 billion won in 2008, and 762.2 billion won in 2010. For example, the cost-of-illness of thyroid disease in 2010 was 3.4 times greater compared to 2002. The direct cost of the total cost-of-illness was 69.7%, which accounted for the highest proportion of costs. Cost-of-illness for individuals between the ages of 30 and 50 accounted for the greatest share of costs.
Conclusion The cost-of-illness of thyroid disease was relatively large in economically active age groups, and demonstrated a very rapid growth rate compared to other major diseases in Korea. Therefore, we suggest nationwide recognition of the importance of prevention and management of thyroid disease and prioritization of the management of thyroid disease among current and future health promotion policies in Korea.
-
Citations
Citations to this article as recorded by- Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Who loses more? Identifying the relationship between hospitalization and income loss: prediction of hospitalization duration and differences of gender and employment status
Minsung Sohn, Daseul Moon, Patricia O’Campo, Carles Muntaner, Haejoo Chung
BMC Public Health.2022;[Epub] CrossRef - The importance and effectiveness of nutritional counselling in patients with autoimmune thyroid diseases in Poland
Ewa Czubek, Klaudia Alcer, Mirjana Varjacic, Piotr Romaniuk
Cost Effectiveness and Resource Allocation.2022;[Epub] CrossRef - Socioeconomic Costs of Dementia Based on Utilization of Health Care and Long-Term-Care Services: A Retrospective Cohort Study
Eun-Jeong Han, JungSuk Lee, Eunhee Cho, Hyejin Kim
International Journal of Environmental Research and Public Health.2021; 18(2): 376. CrossRef - Triennial Report ofEndocrinology and Metabolism, 2015 to 2017
Eun-Jung Rhee, Hey Yeon Jang, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 195. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Cost-of-Illness Trend of Thyroid Gland Disease in Korea
Jae Hoon Chung
Endocrinology and Metabolism.2014; 29(3): 248. CrossRef - Letter: Insufficient Experience in Thyroid Fine-Needle Aspiration Leads to Misdiagnosis of Thyroid Cancer (Endocrinol Metab2014;29:293-9, Jung Il Son et al.)
Hyon-Seung Yi, Sihoon Lee
Endocrinology and Metabolism.2014; 29(4): 590. CrossRef
- Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019

- A Case of Pituitary Abscess that was Difficult to Diagnose due to Repeated Symptomatic Responses to Every Corticosteroid Administration.
- Jin Sun Jang, Jae Seung Yun, Jung Ah Shin, Min Hee Kim, Dong Jun Lim, Jae Hyung Cho, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Ho Young Son, Yong Kil Hong
- Endocrinol Metab. 2011;26(1):72-77. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.72
- 1,640 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Pituitary abscess is a rare pathology, but it is a potentially life-threatening condition. Therefore, timely intervention, including antibiotics and an operation, can prevent the morbidity and mortality in such cases. A 31-year-old woman, who was 16 months after her second delivery, presented with intermittent headache for 3 months. Amenorrhea, polyuria and polydipsia were noticed and the endocrinological hormone studies were compatible with panhypopituitarism and diabetes insipidus. Pituitary MRI demonstrated a 2.3 cm sized cystic mass with an upper small nodular lesion. Her symptoms such as headache and fever were repeatedly improved whenever corticosteroid was administered, which led us to suspect the diagnosis of an inflammatory condition like lymphocytic hypophysitis. During the hormone replacement therapy, her cystic pituitary mass had grown and her symptoms progressively worsened for another two months. The patient underwent trans-sphenoidal exploration and she turned out to have a pituitary abscess. At the 3-month follow-up, amenorrhea was noticed and her residual function of the pituitary was tested by a combined pituitary stimulation test. The results were compatible with panhypopituitarism. She received levothyroxine 100 microg, prednisolone 5 mg and desmopressin spray and she is being observed at the out-patient clinic. The authors experienced a patient with primary pituitary abscess that was confirmed pathologically and we report on its clinical course with a literature review.

- A Case of Insulin Autoimmune Syndrome in a Patient with Partial Hypopituitarism.
- Obin Kwon, Eun Young Park, Jin Young Yoon, Kwang Joon Kim, Yong ho Lee, Jae Won Hong, Eun Jig Lee, Sung Kil Lim, Hyun Chul Lee, Bong Soo Cha
- J Korean Endocr Soc. 2009;24(4):281-286. Published online December 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.4.281
- 1,737 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Insulin autoimmune syndrome is one of the rare causes of hypoglycemia, and characterized by hyperinsulinemic hypoglycemia associated with high titer of antibodies to endogenous insulin. We report a case of insulin autoimmune syndrome in a 57-year-old woman, presenting with mental changes due to hypoglycemia. She had no history of diabetes or insulin administration. The serum C-peptide level was 4.69 ng/mL and the insulin concentration was 229.55 microU/mL, when fasting plasma glucose level was 32 mg/dL. The insulin-to-glucose ratio was 7.17, while there was no radiologic evidence of insulinoma. The insulin antibody level was over 100 microU/mL, resulting in the diagnosis of insulin autoimmune syndrome. Hormonal studies revealed partial hypopituitarism and a lack of glucagon-response to hypoglycemia. Hypoglycemia disappeared with replacement of prednisolone with levothyroxine therapy. Under secretion of growth hormone and of adrenocorticotropic hormone due to hypopituitarism were associated with insufficient counterregulation to hypoglycemia. One should keep in mind that insulin autoimmune syndrome or hypopituitarism is one cause of hypoglycemia in patients with no history of diabetes, and corticosteroid can be an effective treatment for both diseases.

- Suppression of Pathogenic Autoreactive CD4+ T Cells by CD137-mediated Expansion of CD4+CD25+ Regulatory T Cells in Graves' Disease.
- Eun Sook Kim, Hyo Won Jung, Jung Il Choi, Il Seung Nam-Goong, Soon Hyung Hong, Young Il Kim
- J Korean Endocr Soc. 2007;22(5):332-338. Published online October 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.5.332
- 1,796 View
- 21 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Graves' disease (GD) is an organ-specific autoimmune disease that is characterized by lymphocyte infiltration of the thyroid, which finally leads to follicular destruction. The CD4+CD25+ regulatory T cells are important for maintaining peripheral tolerance to self-antigens and impaired activity can cause autoimmune diseases. CD137 (4-1BB), a member of the tumor necrosis factor receptor superfamily and expressed on activated T cells, is a candidate molecule for a co-stimulatory role in autoimmune thyroid disease. In this study, we aimed to assay the frequency of CD4+CD25+ T cells in GD patients and to investigate the role of CD137-mediated costimulation in CD4+CD25+ T cells. METHODS: The frequencies of the CD4+CD25+ T cells in the peripheral blood (PB) of GD patients were determined by flow cytometric analysis. After the CD4+CD25+ T cells were isolated from PB mononuclear cells (PBMC) of the GD patients using immunomagnetic beads, the functional activity of the CD4+CD25+ T cells was characterized by use of a proliferation assay. mRNA expression of Foxp 3 in the CD4+CD25+ T cells of the GD patients was observed by real-time RT-PCR. RESULTS: In this study, we found that GD patients had a low proportion of CD4+CD25+ T cells (mean +/- SD; 1.47 +/- 0.31%) in PBMC as compared with normal subjects. CD137-mediated costimulation increased the expression of CD25 and Foxp 3 in CD4+ T cells in GD patients as compared with normal subjects. Moreover, the CD137-mediated costimulation also induced the proliferation of CD4+CD25+ T cells in GD patients, and the expanded CD4+CD25+ T cells could suppress other CD4+CD25- T cells in a co-culture. CONCLUSION: These results suggest that the peripheral expansion of CD4+CD25+ T cells by CD137-mediated co-stimulation can suppress effector T cells and may be a potent therapy for Graves' disease. -
Citations
Citations to this article as recorded by- Effects of Gastrodia elata Blume on Apoptotic Cell Death of Liver Cancer Cells by Expression of Bcl-2, Bax, and AMPKα
Jae Hyun Park, Min Ho Kang, Ji Woo Hong, So Hee Kim, Yoon Seon Hwang, Jae Hoon Park, Jin Woo Kim
Korean Journal of Medicinal Crop Science.2022; 30(5): 311. CrossRef
- Effects of Gastrodia elata Blume on Apoptotic Cell Death of Liver Cancer Cells by Expression of Bcl-2, Bax, and AMPKα

- Expression of 4-1BB and 4-1BBL in Graves'Disease.
- Eun Sook Kim, Hyo Won Jung, Il Sung Nam-Goong, Soon Joo Woo, Jung Il Choi, Young Il Kim
- J Korean Endocr Soc. 2006;21(2):116-124. Published online April 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.2.116
- 1,835 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
4-1BB mediated costimulatory signal is a recently identified immunotherapeutic strategy for treating autoimmune diseases without depressing the immune response. In this study, we investigated the expression of 4-1BB and 4-1BBL on the peripheral blood mononuclear cells (PBMC) and we assessed whether the serum levels of soluble (s) 4-1BB and s4-1BBL in the patients with Graves' disease (GD) and compared them with normal subjects. METHODS: Expression of 4-1BB and 4-1BBL on PBMC of GD patients was determined by flow cytometry. The concentrations of s4-1BB and s4-1BBL were assessed in the sera of GD patients by performing ELISA. RESULTS: 4-1BB was constitutively expressed on naive CD4+ and CD8+ T cells of the GD patients and this was increased by stimulation. 4-1BBL was also expressed on the antigen-presenting cells such as CD19+ B cells, monocytes and dendritic cells in GD patients. The serum levels of s4-1BB and s4-1BBL were significantly higher in GD patients than those in controls, and these levels were significantly correlated with the serum levels of thyroid-binding inhibitory immunoglobulin and free T4. CONCLUSION: These results indicate that effector T cells of GD patients can be activated through the 4-1BB-mediated costimulatory signal. Elevated s4-1BB and s4-1BBL levels in the sera of GD patients may affect modulation of the clinical course in GD patients. -
Citations
Citations to this article as recorded by- Suppression of Pathogenic Autoreactive CD4+ T Cells by CD137-mediated Expansion of CD4+CD25+ Regulatory T Cells in Graves' Disease
Eun Sook Kim, Hyo Won Jung, Jung Il Choi, Il Seung Nam-Goong, Soon Hyung Hong, Young IL Kim
Journal of Korean Endocrine Society.2007; 22(5): 332. CrossRef
- Suppression of Pathogenic Autoreactive CD4+ T Cells by CD137-mediated Expansion of CD4+CD25+ Regulatory T Cells in Graves' Disease


 KES
KES

 First
First Prev
Prev



