Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Treatment of Hypoparathyroidism by Re-Establishing the Effects of Parathyroid Hormone
- Lars Rejnmark
- Endocrinol Metab. 2024;39(2):262-266. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1916

- 403 View
- 50 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The conventional treatment of hypoparathyroidism (HypoPT) includes active vitamin D and calcium. Despite normalization of calcium levels, the conventional treatment is associated with fluctuations in calcium levels, hypercalciuria, renal impairment, and decreased quality of life (QoL). Replacement therapy with parathyroid hormone (PTH)(1-84) is an option in some countries. However, convincing beneficial effects have not been demonstrated, which may be due to the short duration of action of this treatment. Recently, palopegteriparatide (also known as TransCon PTH) has been marketed in Europe and is expected also to be approved in other countries. Palopegteriparatide is a prodrug with sustained release of PTH(1-34) designed to provide stable physiological PTH levels for 24 hours/day. A phase 3 study demonstrated maintenance of normocalcemia in patients with chronic HypoPT, with no need for conventional therapy. Furthermore, this treatment lowers urinary calcium and improves QoL. Another long-acting PTH analog with effects on the parathyroid hormone receptor (eneboparatide) is currently being tested in a phase 3 trial. Furthermore, the treatment of autosomal dominant hypocalcemia type 1 with a calcilytic (encaleret) is also being tested. All in all, improved treatment options are on the way that will likely take the treatment of HypoPT to the next level.

- Calcium & bone metabolism
- Protein Signatures of Parathyroid Adenoma according to Tumor Volume and Functionality
- Sung Hye Kong, Jeong Mo Bae, Jung Hee Kim, Sang Wan Kim, Dohyun Han, Chan Soo Shin
- Endocrinol Metab. 2024;39(2):375-386. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1827

- 402 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Parathyroid adenoma (PA) is a common endocrine disease linked to multiple complications, but the pathophysiology of the disease remains incompletely understood. The study aimed to identify the key regulator proteins and pathways of PA according to functionality and volume through quantitative proteomic analyses.
Methods
We conducted a retrospective study of 15 formalin-fixed, paraffin-embedded PA samples from tertiary hospitals in South Korea. Proteins were extracted, digested, and the resulting peptides were analyzed using liquid chromatography-tandem mass spectrometry. Pearson correlation analysis was employed to identify proteins significantly correlated with clinical variables. Canonical pathways and transcription factors were analyzed using Ingenuity Pathway Analysis.
Results
The median age of the participants was 52 years, and 60.0% were female. Among the 8,153 protein groups analyzed, 496 showed significant positive correlations with adenoma volume, while 431 proteins were significantly correlated with parathyroid hormone (PTH) levels. The proteins SLC12A9, LGALS3, and CARM1 were positively correlated with adenoma volume, while HSP90AB2P, HLA-DRA, and SCD5 showed negative correlations. DCPS, IRF2BPL, and FAM98A were the main proteins that exhibited positive correlations with PTH levels, and SLITRK4, LAP3, and AP4E1 had negative correlations. Canonical pathway analysis demonstrated that the RAN and sirtuin signaling pathways were positively correlated with both PTH levels and adenoma volume, while epithelial adherence junction pathways had negative correlations.
Conclusion
Our study identified pivotal proteins and pathways associated with PA, offering potential therapeutic targets. These findings accentuate the importance of proteomics in understanding disease pathophysiology and the need for further research.

- Calcium & bone metabolism
- New Insights into Calorie Restriction Induced Bone Loss
- Linyi Liu, Clifford J. Rosen
- Endocrinol Metab. 2023;38(2):203-213. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1673

- 3,301 View
- 176 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Caloric restriction (CR) is now a popular lifestyle choice due to its ability in experimental animals to improve lifespan, reduce body weight, and lessen oxidative stress. However, more and more emerging evidence suggests this treatment requires careful consideration because of its detrimental effects on the skeletal system. Experimental and clinical studies show that CR can suppress bone growth and raise the risk of fracture, but the specific mechanisms are poorly understood. Reduced mechanical loading has long been thought to be the primary cause of weight loss-induced bone loss from calorie restriction. Despite fat loss in peripheral depots with calorie restriction, bone marrow adipose tissue (BMAT) increases, and this may play a significant role in this pathological process. Here, we update recent advances in our understanding of the effects of CR on the skeleton, the possible pathogenic role of BMAT in CR-induced bone loss, and some strategies to mitigate any potential side effects on the skeletal system.
-
Citations
Citations to this article as recorded by- Obesity, diabetes and risk of bone fragility: How BMAT behavior is affected by metabolic disturbances and its influence on bone health
Gregório Corrêa Guimarães, João Bosco Costa Coelho, João Gabriel Oliveira Silva, Ana Carolina Chalfun de Sant’Ana, Cássia Alves Carrilho de Sá, Júlia Marques Moreno, Lívia Marçal Reis, Camila Souza de Oliveira Guimarães
Osteoporosis International.2024; 35(4): 575. CrossRef - Bone Marrow Adipose Tissue Is Not Required for Reconstitution of the Immune System Following Irradiation in Male Mice
Jessica A. Keune, Carmen P. Wong, Adam J. Branscum, Scott A. Menn, Urszula T. Iwaniec, Russell T. Turner
International Journal of Molecular Sciences.2024; 25(4): 1980. CrossRef - Dietary restriction plus exercise change gene expression of Cxcl12 abundant reticular cells in female mice
Aoi Ikedo, Yuuki Imai
Journal of Bone and Mineral Metabolism.2024;[Epub] CrossRef
- Obesity, diabetes and risk of bone fragility: How BMAT behavior is affected by metabolic disturbances and its influence on bone health

- Bone Metabolism
- Normocalcemic Primary Hyperparathyroidism: Need for a Standardized Clinical Approach
- Guido Zavatta, Bart L. Clarke
- Endocrinol Metab. 2021;36(3):525-535. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1061
- 6,257 View
- 377 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
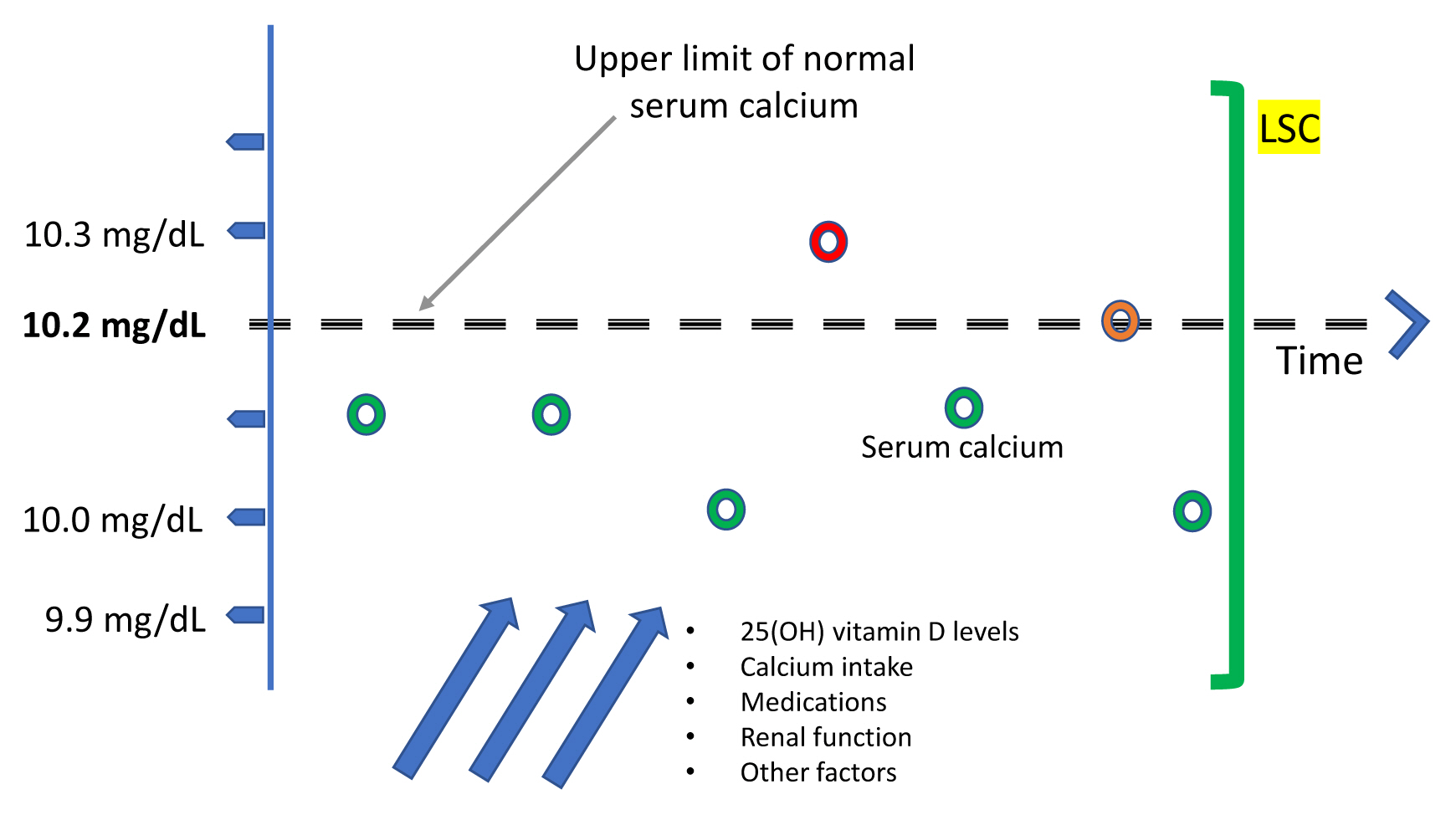
ePub - Since normocalcemic primary hyperparathyroidism (NHPT) was first defined at the Third International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism in 2008, many papers have been published describing its prevalence and possible complications. Guidelines for the management of this condition are still lacking, and making the diagnosis requires fulfillment of strict criteria. Recent studies have shown that intermittent oscillations of serum calcium just below and slightly above the normal limits are very frequent, therefore challenging the assumption that serum calcium must be consistently normal to make the diagnosis. There is debate if these variations in serum calcium outside the normal range should be included under the rubric of NHPT or, rather, a milder form of classical primary hyperparathyroidism. Innovative approaches to define NHPT have been proposed that still need to be validated in prospective studies. Non-classical complications, especially cardiovascular complications, have been associated with NHPT, indicating that hyperparathyroidism may be a cardiovascular risk factor. New associations between parathyroid hormone (PTH) and several other comorbidities have also been reported from observational studies, suggesting that excessive PTH secretion might cause tissue dysfunction independent of serum calcium. Heterogeneous studies using different definitions of NHPT, however, make it difficult to draw definitive conclusions regarding the role of PTH excess when complications other than osteoporosis or kidney stones are described. This review will focus on clinical aspects and suggest an approach to NHPT.
-
Citations
Citations to this article as recorded by- Surgery for Normocalcemic Hyperparathyroidism
Pallavi Kulkarni, David Goldenberg
Otolaryngologic Clinics of North America.2024; 57(1): 111. CrossRef - Linea guida sulla gestione terapeutica dell’iperparatiroidismo primario sporadico nell’adulto
Fabio Vescini, Marco Boniardi, Marina Carotti, Elena Castellano, Cristiana Cipriani, Cristina Eller-Vainicher, Sandro Giannini, Maurizio Iacobone, Francesca Pace, Antonio Stefano Salcuni, Federica Saponaro, Stefano Spiezia, Annibale Versari, Guido Zavatta
L'Endocrinologo.2024; 25(2): 222. CrossRef - DXA-based bone strain index in normocalcemic primary hyperparathyroidism
Gaia Tabacco, Anda Mihaela Naciu, Carmelo Messina, Gianfranco Sanson, Luca Rinaudo, Roberto Cesareo, Stefania Falcone, Nicola Napoli, Fabio Massimo Ulivieri, Andrea Palermo
Osteoporosis International.2023; 34(5): 999. CrossRef - Iperparatiroidismo primario normocalcemico
Silvia Egiddi, Luigi Bonifazi Meffe, Anda Mihaela Naciu, Gaia Tabacco, Nicola Napoli, Andrea Palermo
L'Endocrinologo.2023; 24(3): 249. CrossRef - The Russian registry of primary hyperparathyroidism, latest update
Natalia G. Mokrysheva, Anna K. Eremkina, Alina R. Elfimova, Elena V. Kovaleva, Anastasiia P. Miliutina, Ekaterina E. Bibik, Anna M. Gorbacheva, Ekaterina A. Dobreva, Irina S. Maganeva, Julia A. Krupinova, Rustam H. Salimkhanov, Lizaveta A. Aboishava, Elen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Incidental Normocalcemic Primary Hyperparathyroidism Presenting With Symptomatic Hypophosphatemia: A Case Report
Omar Tabbikha, Joanne Chamy, Michael El Khoury
Cureus.2023;[Epub] CrossRef - Long-term effects of hypercalcemia in kidney transplant recipients with persistent hyperparathyroidism
Juan Carlos Ramirez-Sandoval, Lluvia Marino, Gabriel Cojuc-Konigsberg, Estefania Reul-Linares, Nathalie Desire Pichardo-Cabrera, Cristino Cruz, Elisa Naomi Hernández-Paredes, Nathan Berman-Parks, Vanessa Vidal-Ruíz, Jonathan Mauricio Estrada-Linares, Alfr
Journal of Nephrology.2023;[Epub] CrossRef - Evaluating Patients for Secondary Causes of Osteoporosis
E. Michael Lewiecki
Current Osteoporosis Reports.2022; 20(1): 1. CrossRef - Preoperative Thoracic Muscle Mass Predicts Bone Density Change After Parathyroidectomy in Primary Hyperparathyroidism
Seung Won Burm, Namki Hong, Seunghyun Lee, Gi Jeong Kim, Sang Hyun Hwang, Jongju Jeong, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2474. CrossRef - Applications of Metabolomics in Calcium Metabolism Disorders in Humans
Beata Podgórska, Marta Wielogórska-Partyka, Joanna Godzień, Julia Siemińska, Michał Ciborowski, Małgorzata Szelachowska, Adam Krętowski, Katarzyna Siewko
International Journal of Molecular Sciences.2022; 23(18): 10407. CrossRef - Serum Calcium/Phosphorus Ratio in Biochemical Screening of Primary Hyperparathyroidism
Nagihan Bestepe, Fatma Neslihan Cuhaci, Burcak Polat, Berna Evranos Ogmen, Didem Ozdemir, Reyhan Ersoy, Bekir Cakir
Revista da Associação Médica Brasileira.2022; 68(12): 1668. CrossRef
- Surgery for Normocalcemic Hyperparathyroidism

- Clinical Study
- Radioactive Parathyroid Adenomas on Sestamibi Scans: Low Parathyroid Hormone Secretory Potential and Large Volume
- Sung Hye Kong, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
- Endocrinol Metab. 2021;36(2):351-358. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.823
- 3,350 View
- 123 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We investigated the clinical characteristics of parathyroid adenomas according to radioactivity on 99mTc-methoxyisobutylisonitrile (99mTc-MIBI) single-photon emission computed tomography/computed tomography (SPECT/CT) in primary hyperparathyroidism (PHPT) patients.
Methods
The study included 217 patients diagnosed with PHPT from 2000 to 2019 at Seoul National University Hospital who underwent 99mTc-MIBI SPECT/CT scans. On SPECT/CT, the radioactivity of parathyroid adenomas was measured as the ratio of the mean radioactivity count of the parathyroid adenoma to that of the contralateral thyroid.
Results
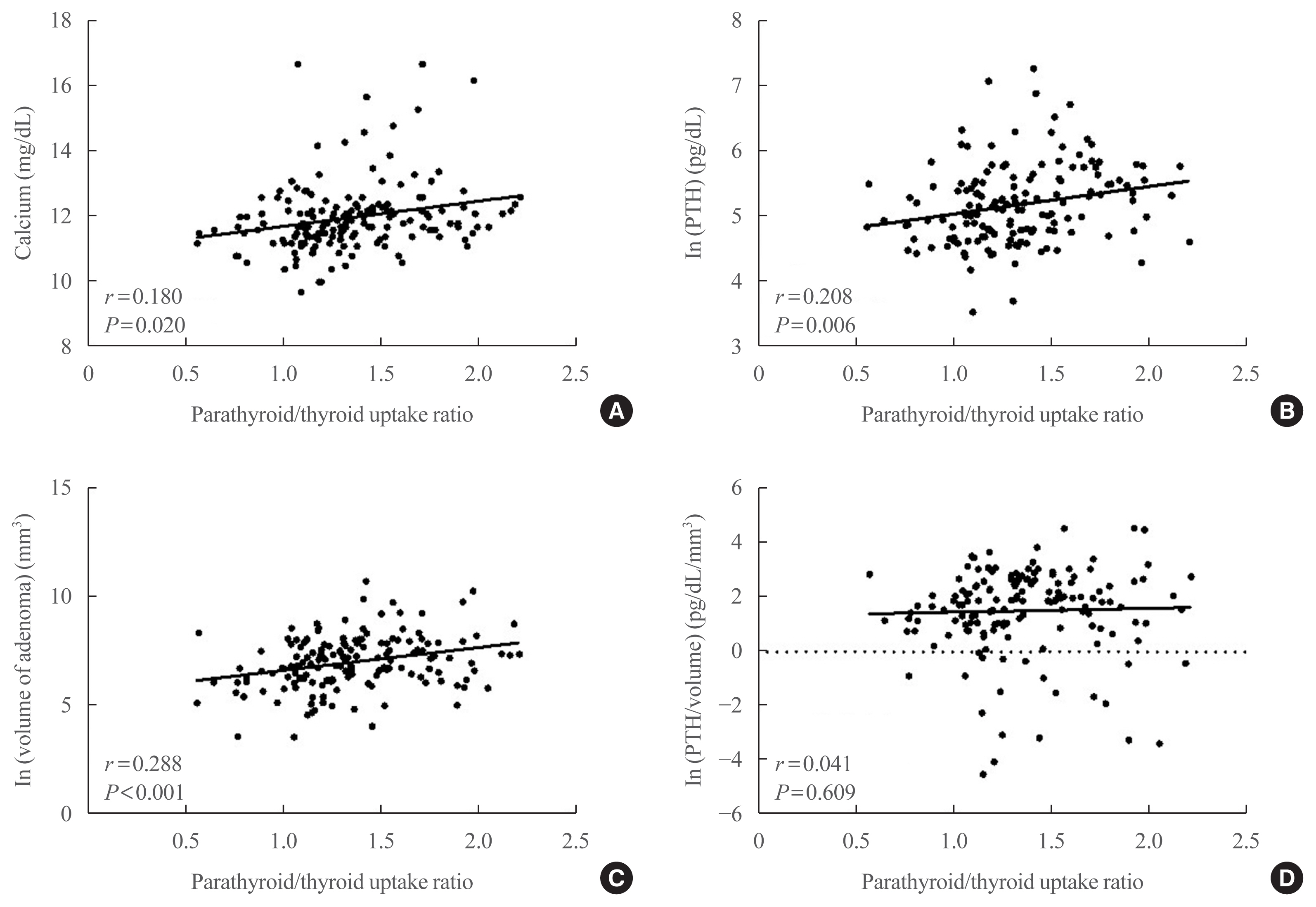
Tumors were localized by MIBI scans in 190 patients (MIBI [+] group) and by ultrasound or parathyroid four-dimensional CT in 27 patients (MIBI [–] group). The mean age was 55 years, and mean body mass index was 23.4 kg/m2. Patients in the MIBI (+) group had higher parathyroid hormone (iPTH) and lower 25-hydroxy vitamin D levels than those in the MIBI (–) group (168.0 pg/mL [interquartile range, IQR, 111.0 to 250.7] vs. 134.7 pg/mL [IQR, 98.2 to 191.2], P=0.049; 15.4 ng/mL [IQR, 11.1 to 20.8] vs. 21.2 ng/mL [IQR, 13.9 to 24.8], P=0.012, respectively). Patients in the MIBI (+) group had larger tumor volumes, but lower iPTH/volume ratios than those in the MIBI (–) group (1,216.66 [IQR, 513.40 to 2,663.02], 499.82 mm3 [IQR, 167.77 to 1,229.80], P=0.002; 0.18 [IQR, 0.08 to 0.46], 0.40 pg/mL/mm3 [IQR, 0.16 to 1.29], P=0.016, respectively). Adenoma radioactivity was positively correlated with calcium, iPTH, and volume (r=0.180, P=0.020; r=0.208, P=0.006; r=0.288, P<0.001, respectively), but not with iPTH/volume.
Conclusion
Parathyroid adenomas with positive MIBI scans had larger volumes and higher iPTH than adenomas with negative scans, but lower iPTH per unit volume. -
Citations
Citations to this article as recorded by- Atypical parathyroid tumor: clinical and parathyroid hormone response to surgical treatment
Antonio Giulio Napolitano, Massimo Monacelli, Valeria Liparulo, Eleonora Coviello, Domenico Pourmolkara, Stefano Avenia, Andrea Polistena
Annals of Surgical Treatment and Research.2023; 105(2): 76. CrossRef - The Relationship between Planar and SPECT/CT Parameters and Functional Markers in Primary Hyperparathyroidism
Guler Silov, Serpil Erdogan Ozbodur
Diagnostics.2023; 13(20): 3182. CrossRef
- Atypical parathyroid tumor: clinical and parathyroid hormone response to surgical treatment

- Miscellaneous
- Rare PTH Gene Mutations Causing Parathyroid Disorders: A Review
- Joon-Hyop Lee, Munkhtugs Davaatseren, Sihoon Lee
- Endocrinol Metab. 2020;35(1):64-70. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.64
- 5,069 View
- 107 Download
- 8 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
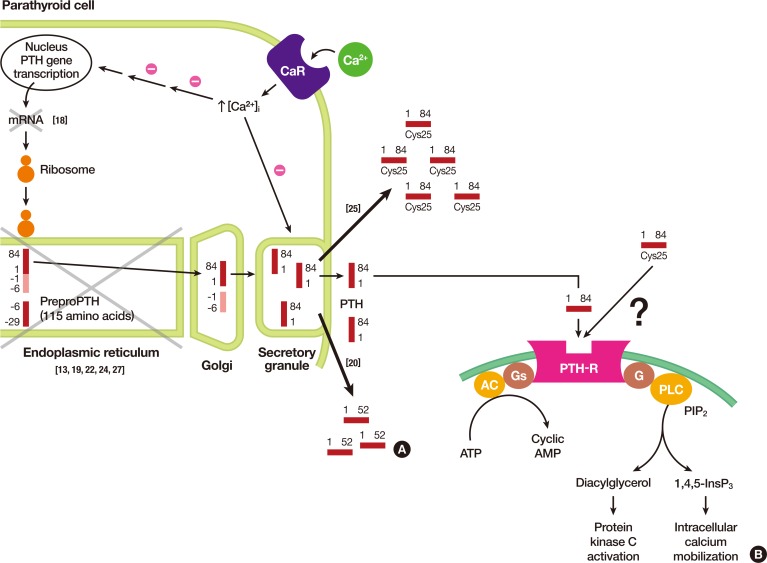
ePub Since parathyroid hormone (PTH) was first isolated and its gene (
PTH ) was sequenced, only eightPTH mutations have been discovered. The C18R mutation inPTH , discovered in 1990, was the first to be reported. This autosomal dominant mutation induces endoplasmic reticulum stress and subsequent apoptosis in parathyroid cells. The next mutation, which was reported in 1992, is associated with exon skipping. The substitution of G with C in the first nucleotide of the second intron results in the exclusion of the second exon; since this exon includes the initiation codon, translation initiation is prevented. An S23P mutation and an S23X mutation at the same residue were reported in 1999 and 2012, respectively. Both mutations resulted in hypoparathyroidism. In 2008, a somatic R83X mutation was detected in a parathyroid adenoma tissue sample collected from a patient with hyperparathyroidism. In 2013, a heterozygous p.Met1_Asp6del mutation was incidentally discovered in a case-control study. Two years later, the R56C mutation was reported; this is the only reported hypoparathyroidism-causing mutation in the mature bioactive part ofPTH . In 2017, another heterozygous mutation, M14K, was detected. The discovery of these eight mutations in thePTH gene has provided insights into its function and broadened our understanding of the molecular mechanisms underlying mutation progression. Further attempts to detect other such mutations will help elucidate the functions of PTH in a more sophisticated manner.-
Citations
Citations to this article as recorded by- Molecular and Clinical Spectrum of Primary Hyperparathyroidism
Smita Jha, William F Simonds
Endocrine Reviews.2023; 44(5): 779. CrossRef - Rare cause of persistent hypocalcaemia in infancy due to PTH gene mutation
Savita Khadse, Vrushali Satish Takalikar, Radha Ghildiyal, Nikhil Shah
BMJ Case Reports.2023; 16(9): e256358. CrossRef - Homozygous Ser-1 to Pro-1 mutation in parathyroid hormone identified in hypocalcemic patients results in secretion of a biologically inactive pro-hormone
Patrick Hanna, Ashok Khatri, Shawn Choi, Severine Brabant, Matti L. Gild, Marie L. Piketty, Bruno Francou, Dominique Prié, John T. Potts, Roderick J. Clifton-Bligh, Agnès Linglart, Thomas J. Gardella, Harald Jüppner
Proceedings of the National Academy of Sciences.2023;[Epub] CrossRef - Genetics of monogenic disorders of calcium and bone metabolism
Paul J. Newey, Fadil M. Hannan, Abbie Wilson, Rajesh V. Thakker
Clinical Endocrinology.2022; 97(4): 483. CrossRef - Homozygous missense variant of PTH (c.166C>T, p.(Arg56Cys)) as the cause of familial isolated hypoparathyroidism in a three-year-old child
Stine Linding Andersen, Anja Lisbeth Frederiksen, Astrid Bruun Rasmussen, Mette Madsen, Ann-Margrethe Rønholt Christensen
Journal of Pediatric Endocrinology and Metabolism.2022; 35(5): 691. CrossRef - Novel PTH Gene Mutations Causing Isolated Hypoparathyroidism
Colin P Hawkes, Jamal M Al Jubeh, Dong Li, Susan E Tucker, Tara Rajiyah, Michael A Levine
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2449. CrossRef
- Molecular and Clinical Spectrum of Primary Hyperparathyroidism

- Miscellaneous
- Intraoperative Parathyroid Hormone Monitoring in the Surgical Management of Sporadic Primary Hyperparathyroidism
- Zahra F. Khan, John I. Lew
- Endocrinol Metab. 2019;34(4):327-339. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.327
- 5,405 View
- 119 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Intraoperative parathyroid hormone monitoring (IPM) has been shown to be a useful adjunct during parathyroidectomy to ensure operative success at many specialized medical centers worldwide. Using the Miami or “>50% intraoperative PTH drop” criterion, IPM confirms the complete excision of all hyperfunctioning parathyroid tissue before the operation is finished, and helps guide the surgeon to identify additional hyperfunctioning parathyroid glands that may necessitate further extensive neck exploration when intraoperative parathyroid hormone (PTH) levels do not drop sufficiently. The intraoperative PTH assay is also used to differentiate parathyroid from non-parathyroid tissues during operations using fine needle aspiration samples and to lateralize the side of the neck harboring the hypersecreting parathyroid through differential jugular venous sampling when preoperative localization studies are negative or equivocal. The use of IPM underscores the recognition and understanding of sporadic primary hyperparathyroidism (SPHPT) as a disease of function rather than form, where the surgeon is better equipped to treat such patients with quantitative instead of qualitative information for durable long-term operative success. There has been a significant paradigm shift over the last 2 decades from conventional to focused parathyroidectomy guided by IPM. This approach has proven to be a safe and rapid operation requiring minimal dissection performed in an ambulatory setting for the treatment of SPHPT.
-
Citations
Citations to this article as recorded by- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy
Phillip Staibano, Kevin Um, Sheila Yu, Mohit Bhandari, Michael K. Gupta, Michael Au, JEM (Ted) Young, Han Zhang
Frontiers in Surgery.2024;[Epub] CrossRef - Primary Hyperparathyroidism
Saba Kurtom, Sally E. Carty
Surgical Clinics of North America.2024;[Epub] CrossRef - Parathyroidectomy for primary hyperparathyroidism: A retrospective analysis of localization, surgical characteristics, and treatment outcomes
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Asian Journal of Surgery.2023; 46(2): 788. CrossRef - Magnitude of parathyroid hormone elevation in primary hyperparathyroidism: Does time of day matter?
C. Corbin Frye, Janessa Sullivan, Sai Anusha Sanka, Jingxia Liu, L. Michael Brunt, William Gillanders, Taylor C. Brown, T.K. Pandian
Surgery.2023; 173(3): 659. CrossRef - Analysis of intraoperative laboratory measurements and imaging techniques such as Tc-99 m-MIBI SPECT/CT, 18F-fluorocholine PET/CT and ultrasound in patients operated with prediagnosis of parathyroid adenoma
Nurullah Bilen, Mehmet Avni Gokalp, Latif Yilmaz, Alper Aytekin, Ilyas Baskonus
Irish Journal of Medical Science (1971 -).2023; 192(4): 1695. CrossRef - Intraoperative Parathyroid Hormone Monitoring Is of Limited Usefulness in Guiding Autotransplantation in Reoperative or Subtotal Parathyroidectomy for Primary Hyperparathyroidism
Bradley A. Richards, Robert A. Vierkant, Benzon M. Dy, Trenton R. Foster, Travis J. McKenzie, Melanie L. Lyden
The American Surgeon™.2023; 89(12): 5421. CrossRef - Does 18F-Fluorocholine PET/CT add value to positive parathyroid scintigraphy in the presurgical assessment of primary hyperparathyroidism?
Alessio Imperiale, Jacob Bani, Gianluca Bottoni, Adrien Latgé, Céline Heimburger, Ugo Catrambone, Michel Vix, Giorgio Treglia, Arnoldo Piccardo
Frontiers in Medicine.2023;[Epub] CrossRef - Intraoperative Identification of Thyroid and Parathyroid Tissues During Human Endocrine Surgery Using the MasSpec Pen
Rachel J. DeHoog, Mary E. King, Michael F. Keating, Jialing Zhang, Marta Sans, Clara L. Feider, Kyana Y. Garza, Alena Bensussan, Anna Krieger, John Q. Lin, Sunil Badal, Elizabeth Alore, Christopher Pirko, Kirtan Brahmbhatt, Wendong Yu, Raymon Grogan, Livi
JAMA Surgery.2023; 158(10): 1050. CrossRef - A Rare Case of Recurrent Parathyroid Adenomas After Initial Parathyroidectomy
Grant N Schalet, Luke Vincent, Carl Eguez, Gerardo Diaz, Mark S Shachner
Cureus.2023;[Epub] CrossRef - Surgical treatment of tertiary hyperparathyroidism: does one fit for all?
Claudio Casella, Claudio Guarneri, Manuela Campanile, Xavier Adhoute, Pier Paolo Gelera, Riccardo Morandi
Frontiers in Endocrinology.2023;[Epub] CrossRef - A >50% Intraoperative Parathyroid Hormone Decrease Into Normal Reference Range Predicts Complete Excision of Malignancy in Patients With Parathyroid Carcinoma
Valerie L. Armstrong, Tanaz M. Vaghaiwalla, Cima Saghira, Cheng-Bang Chen, Yujie Wang, Johan Anantharaj, Mehmet Ackin, John I. Lew
Journal of Surgical Research.2023;[Epub] CrossRef - Variation in parathyroid adenoma size in patients with sporadic, primary hyperparathyroidism: small gland size does not preclude single gland disease
Sophie Dream, Tina W. F. Yen, Kara Doffek, Douglas B. Evans, Tracy S. Wang
Langenbeck's Archives of Surgery.2022; 407(5): 2067. CrossRef - Role and Recent Trend of Intraoperative Parathyroid Hormone Monitoring During Parathyroidectomy in Patients With Primary Hyperparathyroidism
Dongbin Ahn, Ji Hye Kwak
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2022; 65(5): 253. CrossRef - Parathyroid Adenoma: Rare Cause of Acute Recurrent Pancreatitis
Shikha Mahajan, Alka Kumar, Vivek Aggarwal, Vikas Jain, Vipul Baweja, Ajay Ajmani, Diplomate CBNC, Fellow EBNM LNU
Annals of Pediatric Gastroenterology and Hepatology.2022; 2(3-4): 9. CrossRef - Long-term outcome of surgical techniques for sporadic primary hyperparathyroidism in a tertiary referral center in Belgium
Klaas Van Den Heede, Amélie Bonheure, Nele Brusselaers, Sam Van Slycke
Langenbeck's Archives of Surgery.2022; 407(7): 3045. CrossRef - Contribution of intraoperative parathyroid hormone monitoring to the surgical success in minimal invasive parathyroidectomy
Ismail Ethem Akgün, Mehmet Taner Ünlü, Nurcihan Aygun, Mehmet Kostek, Mehmet Uludag
Frontiers in Surgery.2022;[Epub] CrossRef - Surgery for primary hyperparathyroidism
Murilo Catafesta das Neves, Rodrigo Oliveira Santos, Monique Nakayama Ohe
Archives of Endocrinology and Metabolism.2022; 66(5): 678. CrossRef - Використання інтраопераційного моніторингу рівня паратиреоїдного гормону в мінімально інвазивній хірургії щитоподібної та паращитоподібних залоз
S.V. Chernyshov, A.V. Tymkiv, A.V. Vovkanych, I.I. Komisarenko
Endokrynologia.2022; 27(4): 311. CrossRef - Diagnostic Values of Intraoperative (1-84) Parathyroid Hormone Levels are Superior to Intact Parathyroid Hormone for Successful Parathyroidectomy in Patients With Chronic Kidney Disease
Fangyan Xu, Yaoyu Huang, Ming Zeng, Lina Zhang, Wenkai Ren, Hanyang Qian, Ying Cui, Guang Yang, Wenbin Zhou, Shui Wang, Hui Huang, Huimin Chen, Yujie Xiao, Xueyan Gao, Zhanhui Gao, Jing Wang, Cuiping Liu, Jing Zhang, Baiqiao Zhao, Anning Bian, Fan Li, Hui
Endocrine Practice.2021; 27(11): 1065. CrossRef - Delayed Calcium Normalization after Successful Parathyroidectomy in Primary Hyperparathyroidism
Iván Emilio de la Cruz Rodríguez, Elsy Sarahí García Montesinos, María Fernanda Rodríguez-Delgado, Guadalupe Vargas Ortega, Lourdes Balcázar Hernández, Victoria Mendoza Zubieta, Victor Hernández Avendaño, Baldomero González Virla, Micha�l R. Laurent
Case Reports in Endocrinology.2021; 2021: 1. CrossRef - Parathyroid Surgery
Aditya S. Shirali, Uriel Clemente-Gutierrez, Nancy D. Perrier
Neuroimaging Clinics of North America.2021; 31(3): 397. CrossRef - Focused parathyroidectomy without intraoperative parathyroid hormone measurement in primary hyperparathyroidism: Still a valid approach?
Shelby Holt
Surgery.2021; 170(6): 1860. CrossRef - Response to the Comment on “Risk Factors of Redo Surgery After Unilateral Focused Parathyroidectomy – Conclusions From a Comprehensive Nationwide Database of 13,247 Interventions Over 6 Years”
Robert Caiazzo, Camille Marciniak, Francois Pattou
Annals of Surgery.2021; 274(6): e861. CrossRef
- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy

- Adrenal gland
- Effects of Altered Calcium Metabolism on Cardiac Parameters in Primary Aldosteronism
- Jung Soo Lim, Namki Hong, Sungha Park, Sung Il Park, Young Taik Oh, Min Heui Yu, Pil Yong Lim, Yumie Rhee
- Endocrinol Metab. 2018;33(4):485-492. Published online November 30, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.4.485
- 4,062 View
- 43 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Increasing evidence supports interplay between aldosterone and parathyroid hormone (PTH), which may aggravate cardiovascular complications in various heart diseases. Negative structural cardiovascular remodeling by primary aldosteronism (PA) is also suspected to be associated with changes in calcium levels. However, to date, few clinical studies have examined how changes in calcium and PTH levels influence cardiovascular outcomes in PA patients. Therefore, we investigated the impact of altered calcium homeostasis caused by excessive aldosterone on cardiovascular parameters in patients with PA.
Methods Forty-two patients (mean age 48.8±10.9 years; 1:1, male:female) whose plasma aldosterone concentration/plasma renin activity ratio was more than 30 were selected among those who had visited Severance Hospital from 2010 to 2014. All patients underwent adrenal venous sampling with complete access to both adrenal veins.
Results The prevalence of unilateral adrenal adenoma (54.8%) was similar to that of bilateral adrenal hyperplasia. Mean serum corrected calcium level was 8.9±0.3 mg/dL (range, 8.3 to 9.9). The corrected calcium level had a negative linear correlation with left ventricular end-diastolic diameter (LVEDD, ρ=−0.424,
P =0.031). Moreover, multivariable regression analysis showed that the corrected calcium level was marginally associated with the LVEDD and corrected QT (QTc) interval (β=−0.366,P =0.068 and β=−0.252,P =0.070, respectively).Conclusion Aldosterone-mediated hypercalciuria and subsequent hypocalcemia may be partly involved in the development of cardiac remodeling as well as a prolonged QTc interval, in subjects with PA, thereby triggering deleterious effects on target organs additively.
-
Citations
Citations to this article as recorded by- Bone and mineral metabolism in patients with primary aldosteronism: A systematic review and meta-analysis
Anning Wang, Yuhan Wang, Hongzhou Liu, Xiaodong Hu, Jiefei Li, Huaijin Xu, Zhimei Nie, Lingjing Zhang, Zhaohui Lyu
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Bone and mineral metabolism in patients with primary aldosteronism: A systematic review and meta-analysis

- Miscellaneous
- Novel Mutation in PTHLH Related to Brachydactyly Type E2 Initially Confused with Unclassical Pseudopseudohypoparathyroidism
- Jihong Bae, Hong Seok Choi, So Young Park, Do-Eun Lee, Sihoon Lee
- Endocrinol Metab. 2018;33(2):252-259. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.252
- 4,422 View
- 65 Download
- 10 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Autosomal-dominant brachydactyly type E is a congenital abnormality characterized by small hands and feet, which is a consequence of shortened metacarpals and metatarsals. We recently encountered a young gentleman exhibiting shortening of 4th and 5th fingers and toes. Initially, we suspected him having pseudopseudohypoparathyroidism (PPHP) because of normal biochemical parameters, including electrolyte, Ca, P, and parathyroid hormone (PTH) levels; however, his mother and maternal grandmother had the same conditions in their hands and feet. Furthermore, his mother showed normal biochemical parameters. To the best of our knowledge, PPHP is inherited via a mutated paternal allele, owing to the paternal imprinting of GNAS (guanine nucleotide binding protein, alpha stimulating) in the renal proximal tubule. Therefore, we decided to further analyze the genetic background in this family.
Methods Whole exome sequencing was performed using genomic DNA from the affected mother, son, and the unaffected father as a negative control.
Results We selected the intersection between 45,490 variants from the mother and 45,646 variants from the son and excluded 27,512 overlapping variants identified from the father. By excluding homogenous and compound heterozygous variants and removing all previously reported variants, 147 variants were identified to be shared by the mother and son. Variants that had least proximities among species were excluded and finally 23 variants remained.
Conclusion Among them, we identified a defect in parathyroid hormone like hormone (
PTHLH ), encoding the PTH-related protein, to be disease-causative. Herein, we report a family affected with brachydactyly type E2 caused by a novelPTHLH mutation, which was confused with PPHP with unclassical genetic penetrance.-
Citations
Citations to this article as recorded by- A novel heterozygous mutation in PTHLH causing autosomal dominant brachydactyly type E complicated with short stature
Jian Sun, Nian Yang, Zhengquan Xu, Hongbo Cheng, Xiangxin Zhang
Molecular Genetics & Genomic Medicine.2024;[Epub] CrossRef - A novel mutation in PTHLH in a family with a variable phenotype with brachydactyly, short stature, oligodontia and developmental delay
Mirjam E.A. Scheffer-Rath, Hermine E. Veenstra-Knol, Annemieke M. Boot
Bone Reports.2023; 19: 101699. CrossRef - Bioactive phytoconstituents as potent inhibitors of casein kinase-2: dual implications in cancer and COVID-19 therapeutics
Farah Anjum, Md Nayab Sulaimani, Alaa Shafie, Taj Mohammad, Ghulam Md. Ashraf, Anwar L. Bilgrami, Fahad A. Alhumaydhi, Suliman A. Alsagaby, Dharmendra Kumar Yadav, Md. Imtaiyaz Hassan
RSC Advances.2022; 12(13): 7872. CrossRef - Characterization and expression profiling of G protein-coupled receptors (GPCRs) in Spodoptera litura (Lepidoptera: Noctuidae)
Yanxiao Li, Han Gao, Hui Zhang, Runnan Yu, Fan Feng, Jing Tang, Bin Li
Comparative Biochemistry and Physiology Part D: Genomics and Proteomics.2022; 44: 101018. CrossRef - Genes with specificity for expression in the round cell layer of the growth plate are enriched in genomewide association study (GWAS) of human height
Nora E. Renthal, Priyanka Nakka, John M. Baronas, Henry M. Kronenberg, Joel N. Hirschhorn
Journal of Bone and Mineral Research.2020; 36(12): 2300. CrossRef - Search for Novel Mutational Targets in Human Endocrine Diseases
So Young Park, Myeong Han Seo, Sihoon Lee
Endocrinology and Metabolism.2019; 34(1): 23. CrossRef - A Heterozygous Splice-Site Mutation in PTHLH Causes Autosomal Dominant Shortening of Metacarpals and Metatarsals
Monica Reyes, Bert Bravenboer, Harald Jüppner
Journal of Bone and Mineral Research.2019; 34(3): 482. CrossRef - A 3.06-Mb interstitial deletion on 12p11.22-12.1 caused brachydactyly type E combined with pectus carinatum
Jia Huang, Hong-Yan Liu, Rong-Rong Wang, Hai Xiao, Dong Wu, Tao Li, Ying-Hai Jiang, Xue Zhang
Chinese Medical Journal.2019; 132(14): 1681. CrossRef - Parathyroid Hormone-Related Protein in the Hand or Out of Hand?
Sang Wan Kim
Endocrinology and Metabolism.2018; 33(2): 202. CrossRef
- A novel heterozygous mutation in PTHLH causing autosomal dominant brachydactyly type E complicated with short stature

- Miscellaneous
- Effects of Serum Albumin, Calcium Levels, Cancer Stage and Performance Status on Weight Loss in Parathyroid Hormone-Related Peptide Positive or Negative Patients with Cancer
- Ji-Yeon Lee, Namki Hong, Hye Ryun Kim, Byung Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
- Endocrinol Metab. 2018;33(1):97-104. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.97
- 4,428 View
- 45 Download
- 8 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background A recent animal study showed that parathyroid hormone-related peptide (PTHrP) is associated with cancer cachexia by promoting adipose tissue browning, and we previously demonstrated that PTHrP predicts weight loss (WL) in patients with cancer. In this study, we investigated whether prediction of WL by PTHrP is influenced by clinical factors such as serum albumin, corrected calcium levels, cancer stage, and performance status (PS).
Methods A cohort of 219 patients with cancer whose PTHrP level was measured was enrolled and followed for body weight (BW) changes. Subjects were divided into two groups by serum albumin (cutoff value, 3.7 g/dL), corrected calcium (cutoff value, 10.5 mg/dL), cancer stage (stage 1 to 3 or 4), or PS (Eastern Cooperative Oncology Group 0 to 1 or 2 to 4), respectively. Clinically significant WL was defined as either percent of BW change (% BW) <−5% or % BW <−2% plus body mass index (BMI) <20 kg/m2.
Results After a median follow-up of 327 days, 74 patients (33.8%) experienced clinically significant WL. A positive PTHrP level was associated with a 2-fold increased risk of WL after adjusting for age, baseline BMI, serum albumin, corrected calcium level, cancer stage, and PS. The effect of PTHrP on WL remained significant in patients with low serum albumin, stage 4 cancer, and good PS. Regardless of calcium level, the effect of PTHrP on WL was maintained, although there was an additive effect of higher calcium and PTHrP levels.
Conclusion Early recognition of patients with advanced cancer who are PTHrP positive with hypercalcemia or hypoalbuminemia is needed for their clinical management.
-
Citations
Citations to this article as recorded by- Can Patients with Electrolyte Disturbances Be Safely and Effectively Treated in a Hospital-at-Home, Telemedicine-Controlled Environment? A Retrospective Analysis of 267 Patients
Cohn May, Gueron Or, Segal Gad, Zubli Daniel, Hakim Hila, Fizdel Boris, Liber Pninit, Amir Hadar, Barkai Galia
Journal of Clinical Medicine.2024; 13(5): 1409. CrossRef - Parathyroid hormone related protein (PTHrP) in patients with pancreatic carcinoma and overt signs of disease progression and host tissue wasting
Britt-Marie Iresjö, Serkan Kir, Kent Lundholm
Translational Oncology.2023; 36: 101752. CrossRef - Development and Characterization of a Cancer Cachexia Rat Model Transplanted with Cells of the Rat Lung Adenocarcinoma Cell Line Sato Lung Cancer (SLC)
Eiji Kasumi, Miku Chiba, Yoshie Kuzumaki, Hiroyuki Kuzuoka, Norifumi Sato, Banyu Takahashi
Biomedicines.2023; 11(10): 2824. CrossRef - Inhibition of epidermal growth factor receptor suppresses parathyroid hormone‐related protein expression in tumours and ameliorates cancer‐associated cachexia
Bahar Zehra Camurdanoglu Weber, Samet Agca, Aylin Domaniku, Sevval Nur Bilgic, Dilsad H. Arabaci, Serkan Kir
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(3): 1582. CrossRef - Metabolic Reprogramming in Adipose Tissue During Cancer Cachexia
Bahar Zehra Camurdanoglu Weber, Dilsad H. Arabaci, Serkan Kir
Frontiers in Oncology.2022;[Epub] CrossRef
- Can Patients with Electrolyte Disturbances Be Safely and Effectively Treated in a Hospital-at-Home, Telemedicine-Controlled Environment? A Retrospective Analysis of 267 Patients

- Site-Specific Difference of Bone Geometry Indices in Hypoparathyroid Patients
- Hye-Sun Park, Da Hea Seo, Yumie Rhee, Sung-Kil Lim
- Endocrinol Metab. 2017;32(1):68-76. Published online February 6, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.68
- 3,300 View
- 32 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypoparathyroid patients often have a higher bone mineral density (BMD) than the general population. However, an increase in BMD does not necessarily correlate with a solid bone microstructure. This study aimed to evaluate the bone microstructure of hypoparathyroid patients by using hip structure analysis (HSA).
Methods Ninety-five hypoparathyroid patients >20 years old were enrolled and 31 of them had eligible data for analyzing bone geometry parameters using HSA. And among the control data, we extracted sex-, age-, and body mass index-matched three control subjects to each patient. The BMD data were reviewed retrospectively and the bone geometry parameters of the patients were analyzed by HSA.
Results The mean Z-scores of hypoparathyroid patients at the lumbar spine, femoral neck, and total hip were above zero (0.63±1.17, 0.48±1.13, and 0.62±1.10, respectively). The differences in bone geometric parameters were site specific. At the femoral neck and intertrochanter, the cross-sectional area (CSA) and cortical thickness (C.th) were higher, whereas the buckling ratio (BR) was lower than in controls. However, those trends were opposite at the femoral shaft; that is, the CSA and C.th were low and the BR was high.
Conclusion Our study shows the site-specific effects of hypoparathyroidism on the bone. Differences in bone components, marrow composition, or modeling based bone formation may explain these findings. However, further studies are warranted to investigate the mechanism, and its relation to fracture risk.
-
Citations
Citations to this article as recorded by- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism
S. Saha, V. Mannar, D. Kandasamy, V. Sreenivas, R. Goswami
Journal of Endocrinological Investigation.2022; 45(9): 1777. CrossRef - Epidemiology and Financial Burden of Adult Chronic Hypoparathyroidism
Sigridur Bjornsdottir, Steven Ing, Deborah M Mitchell, Tanja Sikjaer, Line Underbjerg, Zaki Hassan-Smith, Jad Sfeir, Neil J Gittoes, Bart L Clarke L
Journal of Bone and Mineral Research.2020; 37(12): 2602. CrossRef - Effect of Endogenous Parathyroid Hormone on Bone Geometry and Skeletal Microarchitecture
A Ram Hong, Ji Hyun Lee, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
Calcified Tissue International.2019; 104(4): 382. CrossRef - Bone responses to chronic treatment of adult hypoparathyroid patients with PTH peptides
Sofie Malmstroem, Lars Rejnmark, Dolores M. Shoback
Current Opinion in Endocrine and Metabolic Research.2018; 3: 51. CrossRef
- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism

- Adrenal gland
- Hypoparathyroidism: Replacement Therapy with Parathyroid Hormone
- Lars Rejnmark, Line Underbjerg, Tanja Sikjaer
- Endocrinol Metab. 2015;30(4):436-442. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.436
- 3,471 View
- 39 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hypoparathyroidism (HypoPT) is characterized by low serum calcium levels caused by an insufficient secretion of parathyroid hormone (PTH). Despite normalization of serum calcium levels by treatment with activated vitamin D analogues and calcium supplementation, patients are suffering from impaired quality of life (QoL) and are at increased risk of a number of comorbidities. Thus, despite normalization of calcium levels in response to conventional therapy, this should only be considered as an apparent normalization, as patients are suffering from a number of complications and calcium-phosphate homeostasis is not normalized in a physiological manner. In a number of recent studies, replacement therapy with recombinant human PTH (rhPTH(1-84)) as well as therapy with the N-terminal PTH fragment (rhPTH(1-34)) have been investigated. Both drugs have been shown to normalize serum calcium while reducing needs for activated vitamin D and calcium supplements. However, once a day injections cause large fluctuations in serum calcium. Twice a day injections diminish fluctuations, but don't restore the normal physiology of calcium homeostasis. Recent studies using pump-delivery have shown promising results on maintaining normocalcemia with minimal fluctuations in calcium levels. Further studies are needed to determine whether this may improve QoL and lower risk of complications. Such data are needed before replacement with the missing hormone can be recommended as standard therapy.
-
Citations
Citations to this article as recorded by- Point-of-Care Peptide Hormone Production Enabled by Cell-Free Protein Synthesis
Madison A. DeWinter, Ariel Helms Thames, Laura Guerrero, Weston Kightlinger, Ashty S. Karim, Michael C. Jewett
ACS Synthetic Biology.2023; 12(4): 1216. CrossRef - Comparing laser speckle contrast imaging and indocyanine green angiography for assessment of parathyroid perfusion
Emmanuel A. Mannoh, Naira Baregamian, Giju Thomas, Carmen C. Solόrzano, Anita Mahadevan-Jansen
Scientific Reports.2023;[Epub] CrossRef - Effects of Multi-stage Procurement on the Viability and Function of Human Donor Parathyroid Glands
Yvonne M. Kelly, Casey Ward, Run Zhang, Shareef Syed, Peter G. Stock, Quan-Yang Duh, Julie A. Sosa, James Koh
Journal of Surgical Research.2022; 276: 404. CrossRef - Kidney Complications and Hospitalization in Patients With Chronic Hypoparathyroidism: A Cohort Study in Sweden
Oskar Swartling, Marie Evans, Tim Spelman, Wafa Kamal, Olle Kämpe, Michael Mannstadt, Ylva Trolle Lagerros, Sigridur Björnsdottir
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4098. CrossRef - Hypocalcaemia
Zaki Hassan-Smith, Neil Gittoes
Medicine.2021; 49(9): 562. CrossRef - Safety and Efficacy of 5 Years of Treatment With Recombinant Human Parathyroid Hormone in Adults With Hypoparathyroidism
Michael Mannstadt, Bart L Clarke, John P Bilezikian, Henry Bone, Douglas Denham, Michael A Levine, Munro Peacock, Jeffrey Rothman, Dolores M Shoback, Mark L Warren, Nelson B Watts, Hak-Myung Lee, Nicole Sherry, Tamara J Vokes
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5136. CrossRef - Management of Endocrine Emergencies in the ICU
Judith Jacobi
Journal of Pharmacy Practice.2019; 32(3): 314. CrossRef - Microencapsulated parathyroid allotransplantation in the omental tissue
Emrah Yucesan, Harun Basoglu, Beyza Goncu, Fahri Akbas, Yeliz Emine Ersoy, Erhan Aysan
Artificial Organs.2019; 43(10): 1022. CrossRef - Die HypAus-Studie
Maximilian Zach, Adelina Tmava-Berisha, Stefan Schatzl, Michael Lehner, Greisa Vila, Karin Amrein
Journal für Klinische Endokrinologie und Stoffwechsel.2018; 11(2): 45. CrossRef -
Sustained release of parathyroid hormone via
in situ
cross‐linking gelatin hydrogels improves the therapeutic potential of tonsil‐derived mesenchymal stem cells for hypoparathyroidism
Yoon Shin Park, Yunki Lee, Yoon Mi Jin, Gyungah Kim, Sung Chul Jung, Yoon Jeong Park, Ki Dong Park, Inho Jo
Journal of Tissue Engineering and Regenerative Medicine.2018;[Epub] CrossRef - Hypocalcaemia
Zaki Hassan-Smith, Neil Gittoes
Medicine.2017; 45(9): 555. CrossRef
- Point-of-Care Peptide Hormone Production Enabled by Cell-Free Protein Synthesis

- Bone Metabolism
- Emerging Therapies for Osteoporosis
- Michael R. McClung
- Endocrinol Metab. 2015;30(4):429-435. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.429
- 4,367 View
- 47 Download
- 23 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Although several effective therapies are available for the treatment of osteoporosis in postmenopausal women and older men, there remains a need for the development of even more effective and acceptable drugs. Several new drugs that are in late-stage clinical development will be discussed. Abaloparatide (recombinant parathyroid hormone related peptide [PTHrP] analogue) has anabolic activity like teriparatide. Recent data from the phase 3 fracture prevention trial demonstrate that this agent is effective in reducing fracture risk. Inhibiting cathepsin K reduces bone resorption without decreasing the numbers or activity of osteoclasts, thereby preserving or promoting osteoblast function. Progressive increases in bone mineral density (BMD) have been observed over 5 years. Early data suggest that odanacatib effectively reduces fracture risk. Lastly, inhibiting sclerostin with humanized antibodies promotes rapid, substantial but transient increases in bone formation while inhibiting bone resorption. Marked increases in BMD have been observed in phase 2 studies. Fracture prevention studies are underway. The new therapies with novel and unique mechanisms of action may, alone or in combination, provide more effective treatment options for our patients.
-
Citations
Citations to this article as recorded by- The osteocyte as a signaling cell
Jesus Delgado-Calle, Teresita Bellido
Physiological Reviews.2022; 102(1): 379. CrossRef - Combining sclerostin neutralization with tissue engineering: An improved strategy for craniofacial bone repair
Sophie Maillard, Ludovic Sicard, Caroline Andrique, Coralie Torrens, Julie Lesieur, Brigitte Baroukh, Thibaud Coradin, Anne Poliard, Lotfi Slimani, Catherine Chaussain
Acta Biomaterialia.2022; 140: 178. CrossRef - Effects of sclerostin antibody on bone healing
Atsushi Mihara, Kiminori Yukata, Toshihiro Seki, Ryuta Iwanaga, Norihiro Nishida, Kenzo Fujii, Yuji Nagao, Takashi Sakai
World Journal of Orthopedics.2021; 12(9): 651. CrossRef - Combining Sclerostin Neutralization with Tissue Engineering: An Improved Strategy for Craniofacial Bone Repair
Sophie Maillard, Ludovic Sicard, Caroline Andrique, Coralie Torrens, Julie Lesieur, Brigitte Baroukh, Thibaud Coradin, Anne Poliard, Lotfi Slimani, Catherine Chaussain
SSRN Electronic Journal.2021;[Epub] CrossRef - Potential Biomarkers to Improve the Prediction of Osteoporotic Fractures
Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
Endocrinology and Metabolism.2020; 35(1): 55. CrossRef - Clinical Application of Teriparatide in Fracture Prevention
Yuehong Chen, Ronghan Liu, Aubryanna Hettinghouse, Shuya Wang, Gang Liu, Chuan-ju Liu
JBJS Reviews.2019; 7(1): e10. CrossRef - The Emerging Role of Osteocytes in Cancer in Bone
Emily G Atkinson, Jesús Delgado‐Calle
JBMR Plus.2019;[Epub] CrossRef - Osteoporosis therapies might lead to intervertebral disc degeneration via affecting cartilage endplate
Zhen Sun, Zhuo-Jing Luo
Medical Hypotheses.2019; 125: 5. CrossRef - Polymersome nanoparticles for delivery of Wnt-activating small molecules
Edoardo Scarpa, Agnieszka A Janeczek, Alethia Hailes, Maria C de Andrés, Antonio De Grazia, Richard OC Oreffo, Tracey A Newman, Nicholas D Evans
Nanomedicine: Nanotechnology, Biology and Medicine.2018; 14(4): 1267. CrossRef - Dual roles of QOA-8a in antiosteoporosis: a combination of bone anabolic and anti-resorptive effects
Jing Wu, Qi Shen, Wei Cui, Yu Zhao, Yue Huai, Yu-chao Zhang, Bei-hua Bao, Chen-xi Liu, Qing Jiang, Jian-xin Li
Acta Pharmacologica Sinica.2018; 39(2): 230. CrossRef - Abaloparatide: Recombinant human PTHrP (1–34) anabolic therapy for osteoporosis
Chee Kian Chew, Bart L. Clarke
Maturitas.2017; 97: 53. CrossRef - Dried and free flowing granules of Spinacia oleracea accelerate bone regeneration and alleviate postmenopausal osteoporosis
Sulekha Adhikary, Dharmendra Choudhary, Naseer Ahmad, Sudhir Kumar, Kapil Dev, Naresh Mittapelly, Gitu Pandey, Prabhat Ranjan Mishra, Rakesh Maurya, Ritu Trivedi
Menopause.2017; 24(6): 686. CrossRef - Romosozumab for the treatment of osteoporosis
Leonardo Bandeira, E. Michael Lewiecki, John P. Bilezikian
Expert Opinion on Biological Therapy.2017; 17(2): 255. CrossRef - The quest for new drugs to prevent osteoporosis-related fractures
T. J. de Villiers
Climacteric.2017; 20(2): 103. CrossRef - Role and mechanism of action of sclerostin in bone
Jesus Delgado-Calle, Amy Y. Sato, Teresita Bellido
Bone.2017; 96: 29. CrossRef - Biochemical Testing Relevant to Bone
Chee Kian Chew, Bart L. Clarke
Endocrinology and Metabolism Clinics of North America.2017; 46(3): 649. CrossRef - Re-Invigorating the Osteoporosis Message
Michael R. McClung
Endocrine Practice.2016; 22(9): 1130. CrossRef - Pharmacodynamics and pharmacokinetics of oral salmon calcitonin in the treatment of osteoporosis
Leonardo Bandeira, E. Michael Lewiecki, John P. Bilezikian
Expert Opinion on Drug Metabolism & Toxicology.2016; 12(6): 681. CrossRef - Osteoporosis treatment: bisphosphonates reign to continue for a few more years, at least?
Michael Pazianas, Bo Abrahamsen
Annals of the New York Academy of Sciences.2016; 1376(1): 5. CrossRef - Anti-senescence and Anti-inflammatory Effects of the C-terminal Moiety of PTHrP Peptides in OA Osteoblasts
Julia Platas, Maria Isabel Guillén, Francisco Gomar, Miguel Angel Castejón, Pedro Esbrit, Maria José Alcaraz
The Journals of Gerontology Series A: Biological Sciences and Medical Sciences.2016; : glw100. CrossRef - Osteocytic signalling pathways as therapeutic targets for bone fragility
Lilian I. Plotkin, Teresita Bellido
Nature Reviews Endocrinology.2016; 12(10): 593. CrossRef
- The osteocyte as a signaling cell

- Preoperative Localization and Intraoperative Parathyroid Hormone Assay in Korean Patients with Primary Hyperparathyroidism
- Eirie Cho, Jung Mi Chang, Seok Young Yoon, Gil Tae Lee, Yun Hyi Ku, Hong Il Kim, Myung-Chul Lee, Guk Haeng Lee, Min Joo Kim
- Endocrinol Metab. 2014;29(4):464-469. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.464
- 3,523 View
- 32 Download
- 8 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The intraoperative parathyroid hormone (IOPTH) assay is widely used in patients with primary hyperparathyroidism (PHPT). We investigated the usefulness of the IOPTH assay in Korean patients with PHPT.
Methods We retrospectively reviewed the data of 33 patients with PHPT who underwent parathyroidectomy. Neck ultrasonography (US) and 99mTc-sestamibi scintigraphy (MIBI scan) were performed preoperatively and IOPTH assays were conducted.
Results The sensitivity of neck US and MIBI scans were 91% and 94%, respectively. A 50% decrease in parathyroid hormone (PTH) levels 10 minutes after excision of the parathyroid gland was obtained in 91% (30/33) of patients and operative success was achieved in 97% (32/33) of patients. The IOPTH assay was 91% true-positive, 3% true-negative, 0% false-positive, and 6% false-negative. The overall accuracy of the IOPTH assay was 94%. In five cases with discordant neck US and MIBI scan results, a sufficient decrease in IOPTH levels helped the surgeon confirm the complete excision of the parathyroid gland with no additional neck exploration.
Conclusion The IOPTH assay is an accurate tool for localizing hyperfunctioning parathyroid glands and is helpful for evaluating cases with discordant neck US and MIBI scan results.
-
Citations
Citations to this article as recorded by- Single-Center Experience of Parathyroidectomy Using Intraoperative Parathyroid Hormone Monitoring
Seong Hoon Kim, Si Yeon Lee, Eun Ah Min, Young Mi Hwang, Yun Suk Choi, Jin Wook Yi
Medicina.2022; 58(10): 1464. CrossRef - The natural history and hip geometric changes of primary hyperparathyroidism without parathyroid surgery
Kyong Yeun Jung, A. Ram Hong, Dong Hwa Lee, Jung Hee Kim, Kyoung Min Kim, Chan Soo Shin, Seong Yeon Kim, Sang Wan Kim
Journal of Bone and Mineral Metabolism.2017; 35(3): 278. CrossRef - The utility of the radionuclide probe in parathyroidectomy for primary hyperparathyroidism
MS Lim, M Jinih, CH Ngai, NM Foley, HP Redmond
The Annals of The Royal College of Surgeons of England.2017; 99(5): 369. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Single-Center Experience of Parathyroidectomy Using Intraoperative Parathyroid Hormone Monitoring

- 1-34 PTH Could Reverse Impaired Bone Mineralization Induced By the Overdose of Bisphosphonate.
- Kyeong Hye Park, Kwang Joon Kim, Han Seok Choi, Kyoung Min Kim, Eun Young Lee, Seonhui Han, Hyun Sil Kim, Daham Kim, Hannah Seok, Eun Yeong Choe, Yumie Rhee, Sung Kil Lim
- Endocrinol Metab. 2012;27(3):247-250. Published online September 19, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.3.247
- 12,679 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Bisphosphonates are the mainstay of osteoporosis treatment. Despite the fact that bisphosphonates have a relatively good safety record and are tolerated well by the majority of patients, serious adverse events have been associated with their use. A 41-year-old man had been diagnosed with osteoporosis and had taken etidronate 200 mg/day daily for 2 years due to the judgmental error. He was referred for the management of refractory bone pain and generalized muscle ache. Serum calcium, phosphate, 25-hydroxy-vitamin D (25(OH)D), and immunoreactive parathyroid hormone (iPTH) were within normal range. Plain X-ray showed multiple fractures. Whole body bone scan confirmed multiple sites of increased bone uptakes. Tetracycline-labeled bone biopsy showed typical findings of osteomalacia. He was diagnosed with iatrogenic, etidronate-induced osteomalacia. The patient received daily parathyroid hormone (PTH) injection for 18 months. PTH effectively reverses impaired bone mineralization caused by etidronate misuse. Currently, he is doing well without bone pain. Bone mineral density significantly increased, and the increased bone uptake was almost normalized after 18 months. This case seems to suggest that human PTH (1-34) therapy, possibly in association with calcium and vitamin D, is associated with important clinical improvements in patients with impaired bone mineralization due to the side effect of bisphosphonate.


 KES
KES

 First
First Prev
Prev



