Search
- Page Path
- HOME > Search
Review Article
- Thyroid
- Thyroid Function across the Lifespan: Do Age-Related Changes Matter?
- John P. Walsh
- Endocrinol Metab. 2022;37(2):208-219. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1463
- 6,095 View
- 340 Download
- 12 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
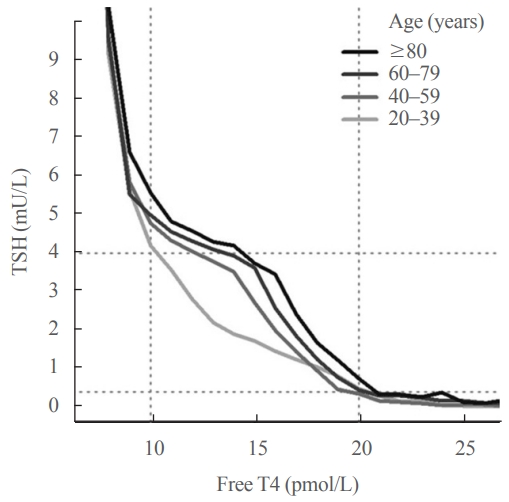
ePub - Circulating concentrations of thyrotropin (TSH) and thyroxine (T4) are tightly regulated. Each individual has setpoints for TSH and free T4 which are genetically determined, and subject to environmental and epigenetic influence. Pituitary-thyroid axis setpoints are probably established in utero, with maturation of thyroid function continuing until late gestation. From neonatal life (characterized by a surge of TSH and T4 secretion) through childhood and adolescence (when free triiodothyronine levels are higher than in adults), thyroid function tests display complex, dynamic patterns which are sexually dimorphic. In later life, TSH increases with age in healthy older adults without an accompanying fall in free T4, indicating alteration in TSH setpoint. In view of this, and evidence that mild subclinical hypothyroidism in older people has no health impact, a strong case can be made for implementation of age-related TSH reference ranges in adults, as is routine in children.
-
Citations
Citations to this article as recorded by- The ageing thyroid: implications for longevity and patient care
Diana van Heemst
Nature Reviews Endocrinology.2024; 20(1): 5. CrossRef - Incidence and Determinants of Spontaneous Normalization of Subclinical Hypothyroidism in Older Adults
Evie van der Spoel, Nicolien A van Vliet, Rosalinde K E Poortvliet, Robert S Du Puy, Wendy P J den Elzen, Terence J Quinn, David J Stott, Naveed Sattar, Patricia M Kearney, Manuel R Blum, Heba Alwan, Nicolas Rodondi, Tinh-Hai Collet, Rudi G J Westendorp,
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1167. CrossRef - Multi-trait analysis characterizes the genetics of thyroid function and identifies causal associations with clinical implications
Rosalie B. T. M. Sterenborg, Inga Steinbrenner, Yong Li, Melissa N. Bujnis, Tatsuhiko Naito, Eirini Marouli, Tessel E. Galesloot, Oladapo Babajide, Laura Andreasen, Arne Astrup, Bjørn Olav Åsvold, Stefania Bandinelli, Marian Beekman, John P. Beilby, Jette
Nature Communications.2024;[Epub] CrossRef - Evaluation of multiple organophosphate insecticide exposure in relation to altered thyroid hormones in NHANES 2007‐2008 adult population
Massira Ousseni Diawara, Songtao Li, Mingzhi Zhang, Francis Manyori Bigambo, Xu Yang, Xu Wang, Tianyu Dong, Di Wu, Chenghao Yan, Yankai Xia
Ecotoxicology and Environmental Safety.2024; 273: 116139. CrossRef - Thyroid-function reference ranges in the diagnosis of thyroid dysfunction in adults
Salman Razvi
Nature Reviews Endocrinology.2024; 20(5): 253. CrossRef - Association between exposure to chemical mixtures and epigenetic ageing biomarkers: Modifying effects of thyroid hormones and physical activity
Wanying Shi, Jianlong Fang, Huimin Ren, Peijie Sun, Juan Liu, Fuchang Deng, Shuyi Zhang, Qiong Wang, Jiaonan Wang, Shilu Tong, Song Tang, Xiaoming Shi
Journal of Hazardous Materials.2024; 469: 134009. CrossRef - DNA Methylation in Autoimmune Thyroid Disease
Nicole Lafontaine, Scott G Wilson, John P Walsh
The Journal of Clinical Endocrinology & Metabolism.2023; 108(3): 604. CrossRef - A Causality between Thyroid Function and Bone Mineral Density in Childhood: Abnormal Thyrotropin May Be Another Pediatric Predictor of Bone Fragility
Dongjin Lee, Moon Ahn
Metabolites.2023; 13(3): 372. CrossRef - Serum Lipidomic Analysis Reveals Biomarkers and Metabolic Pathways of Thyroid Dysfunction
Hua Dong, Wenjie Zhou, Xingxu Yan, Huan Zhao, Honggang Zhao, Yan Jiao, Guijiang Sun, Yubo Li, Zuncheng Zhang
ACS Omega.2023; 8(11): 10355. CrossRef - Developmental and environmental modulation of fecal thyroid hormone levels in wild Assamese macaques (Macaca assamensis)
Verena Behringer, Michael Heistermann, Suchinda Malaivijitnond, Oliver Schülke, Julia Ostner
American Journal of Primatology.2023;[Epub] CrossRef - Prevalence of Functional Alterations and the Effects of Thyroid
Autoimmunity on the Levels of TSH in an Urban Population of Colombia:
A Population-Based Study
Hernando Vargas-Uricoechea, Valentina Agredo-Delgado, Hernando David Vargas-Sierra, María V. Pinzón-Fernández
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(6): 857. CrossRef - Genetic determinants of thyroid function in children
Tessa A Mulder, Purdey J Campbell, Peter N Taylor, Robin P Peeters, Scott G Wilson, Marco Medici, Colin Dayan, Vincent V W Jaddoe, John P Walsh, Nicholas G Martin, Henning Tiemeier, Tim I M Korevaar
European Journal of Endocrinology.2023; 189(2): 164. CrossRef - Relationship between Thyroid CT Density, Volume, and Future TSH Elevation: A 5-Year Follow-Up Study
Tomohiro Kikuchi, Shouhei Hanaoka, Takahiro Nakao, Yukihiro Nomura, Takeharu Yoshikawa, Md Ashraful Alam, Harushi Mori, Naoto Hayashi
Life.2023; 13(12): 2303. CrossRef - Thyroid Stimulating Hormone and Thyroid Hormones (Triiodothyronine and Thyroxine): An American Thyroid Association-Commissioned Review of Current Clinical and Laboratory Status
Katleen Van Uytfanghe, Joel Ehrenkranz, David Halsall, Kelly Hoff, Tze Ping Loh, Carole A. Spencer, Josef Köhrle
Thyroid®.2023; 33(9): 1013. CrossRef - Blood hormones and suicidal behaviour: A systematic review and meta-analysis
Xue-Lei Fu, Xia Li, Jia-Mei Ji, Hua Wu, Hong-Lin Chen
Neuroscience & Biobehavioral Reviews.2022; 139: 104725. CrossRef
- The ageing thyroid: implications for longevity and patient care

Original Articles
- Diabetes, Obesity and Metabolism
- Reference Values for Skeletal Muscle Mass at the Third Lumbar Vertebral Level Measured by Computed Tomography in a Healthy Korean Population
- Ja Kyung Yoon, Sunyoung Lee, Kyoung Won Kim, Ji Eun Lee, Jeong Ah Hwang, Taeyong Park, Jeongjin Lee
- Endocrinol Metab. 2021;36(3):672-677. Published online June 8, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1041
- 4,319 View
- 158 Download
- 13 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
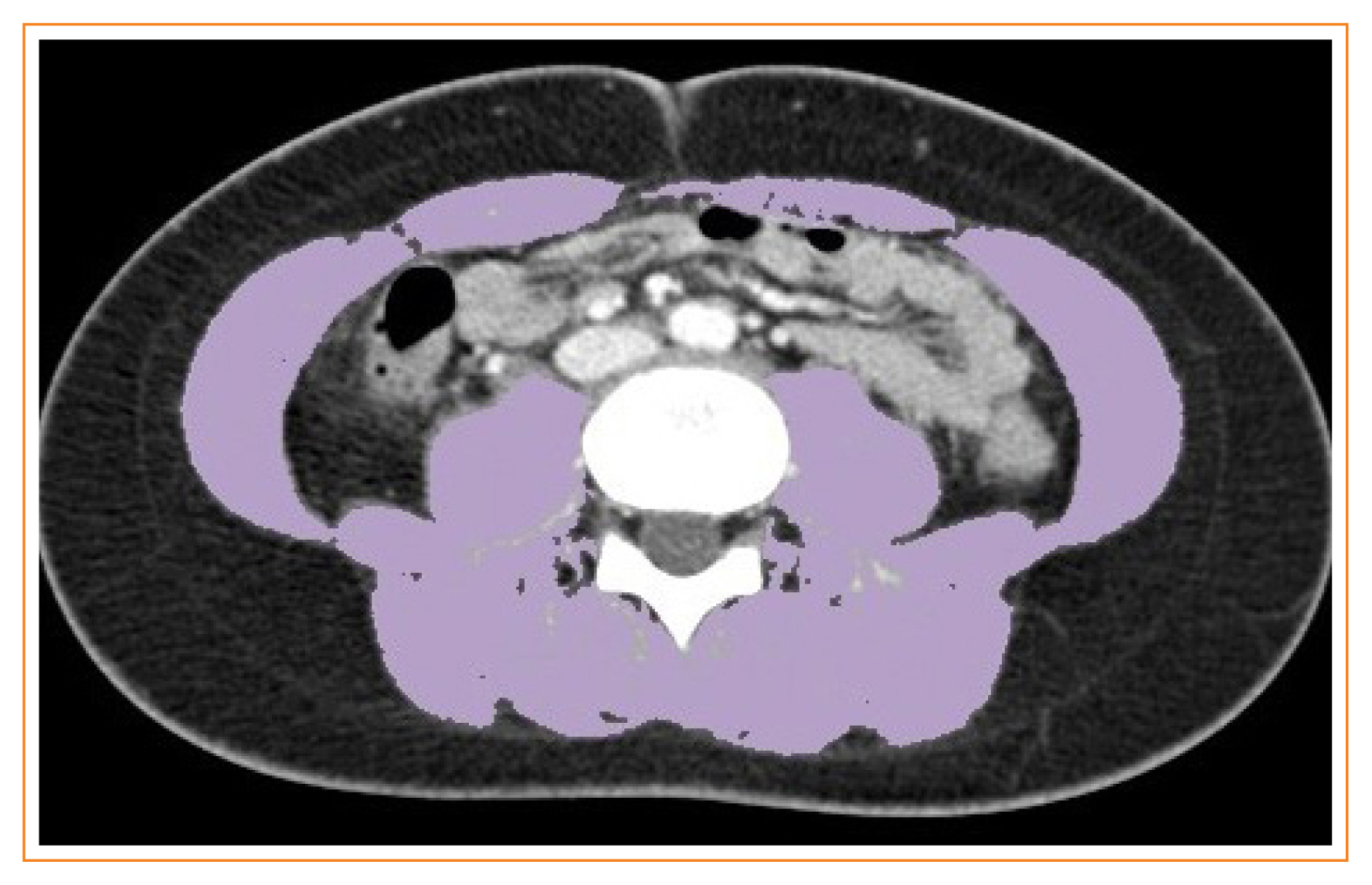
Sarcopenia is defined as the loss of skeletal muscle mass and is associated with negative clinical outcomes. This study aimed to establish sex-specific cutoff values for the skeletal muscle area (SMA) and skeletal muscle index (SMI) at the third lumbar vertebral (L3) level using computed tomography (CT) imaging to identify sarcopenia in healthy Korean liver donors.
Methods
This retrospective study included 659 healthy liver donors (408 men and 251 women) aged 20 to 60 years who had undergone abdominal CT examinations between January 2017 and December 2018. Assessment of body composition was performed with an automated segmentation technique using a deep-learning system. Sex-specific SMA and SMI distributions were assessed, and cutoff values for determining sarcopenia were defined as values at either two standard deviations (SDs) below the mean reference value or below the fifth percentile.
Results
Using the SD definition, cutoff values for SMA and SMI were 117.04 cm2 and 39.33 cm2/m2, respectively, in men and 71.39 cm2 and 27.77 cm2/m2, respectively, in women. Using the fifth percentile definition, cutoff values for SMA and SMI were 126.88 cm2 and 40.96 cm2/m2, respectively, in men and 78.85 cm2 and 30.60 cm2/m2, respectively, in women.
Conclusion
Our data provide sex-specific cutoff values for the SMA and SMI at the L3 level measured by CT imaging in a healthy Korean population, which may be applicable for identifying sarcopenia in this population. -
Citations
Citations to this article as recorded by- Myosteatosis is associated with poor survival after kidney transplantation: a large retrospective cohort validation
Jie Chen, Yue Li, Chengjie Li, Turun Song
Abdominal Radiology.2024; 49(4): 1210. CrossRef - The effect of biological agent on body composition in patients with Crohn’s disease
Eun Jeong Choi, Dong Hoon Baek, Hong Sub Lee, Geun Am Song, Tae Oh Kim, Yong Eun Park, Chang Min Lee, Jong Hoon Lee
BMC Gastroenterology.2023;[Epub] CrossRef - The Association between the L3 Skeletal Muscle Index Derived from Computed Tomography and Clinical Outcomes in Patients with Urinary Tract Infection in the Emergency Department
Jinjoo An, Seung Pill Choi, Jae Hun Oh, Jong Ho Zhu, Sung Wook Kim, Soo Hyun Kim
Journal of Clinical Medicine.2023; 12(15): 5024. CrossRef - Validity of computed tomography defined body composition as a prognostic factor for functional outcome after kidney transplantation
Tim D. A. Swaab, Evelien E. Quint, Lisa B. Westenberg, Marcel Zorgdrager, Dorry L. Segev, Mara A. McAdams‐DeMarco, Stephan J. L. Bakker, Alain R. Viddeleer, Robert A. Pol
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(6): 2532. CrossRef - Assessment of the Diaphragm Thickness Decrease in Critically Ill COVID-19 Patients: Could Computed Tomography Be of Aid Regarding Diaphragm Muscle Mass?
Oana-Elena Branea, Sanda Maria Copotoiu, Diana Andreea Becica, AnaMaria Romina Budeanu, Razvan Gabriel Budeanu, Mihai Emanuel Becica, Dragos Constantin Cucoranu, Septimiu Voidazan, Monica Chis, Alexandra Elena Lazar
Cureus.2023;[Epub] CrossRef - Clinical implication of thoracic skeletal muscle volume as a predictor of ventilation-weaning failure in brain-injured patients: A retrospective observational study
Jimi Oh, Hyun Lim, Chang Won Jeong, Min Su Kim, Jinseok Lee, Wu Seong Kang, Ui Ri An, Joo Un Park, Youngick Ahn, Youe Ree Kim, Chul Park
Medicine.2023; 102(43): e35847. CrossRef - Estimation of Muscle Mass Using Creatinine/Cystatin C Ratio in Japanese Community-Dwelling Older People
Hiroshi Kusunoki, Yasuharu Tabara, Shotaro Tsuji, Yosuke Wada, Kayoko Tamaki, Koutatsu Nagai, Masako Itoh, Kyoko Sano, Manabu Amano, Hatsuo Maeda, Hideyuki Sugita, Yoko Hasegawa, Hiromitsu Kishimoto, Soji Shimomura, Michiya Igase, Ken Shinmura
Journal of the American Medical Directors Association.2022; 23(5): 902.e21. CrossRef - Defining reference values for low skeletal muscle index at the L3 vertebra level based on computed tomography in healthy adults: A multicentre study
Ming Kong, Nan Geng, Ying Zhou, Ning Lin, Wenyan Song, Manman Xu, Shanshan Li, Yuetong Piao, Zuoqing Han, Rong Guo, Chao Yang, Nan Luo, Zhong Wang, Mengyuan Jiang, Lili Wang, Wanchun Qiu, Junfeng Li, Daimeng Shi, Rongkuan Li, Eddie C. Cheung, Yu Chen, Zho
Clinical Nutrition.2022; 41(2): 396. CrossRef - The Value of Artificial Intelligence-Assisted Imaging in Identifying Diagnostic Markers of Sarcopenia in Patients with Cancer
Ying-Tzu Huang, Yi-Shan Tsai, Peng-Chan Lin, Yu-Min Yeh, Ya-Ting Hsu, Pei-Ying Wu, Meng-Ru Shen, Zhongjie Shi
Disease Markers.2022; 2022: 1. CrossRef - Assessment of Muscle Quantity, Quality and Function
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 9. CrossRef - Computed Tomography-Derived Skeletal Muscle Radiodensity Is an Early, Sensitive Marker of Age-Related Musculoskeletal Changes in Healthy Adults
Yeon Woo Jung, Namki Hong, Joon Chae Na, Woong Kyu Han, Yumie Rhee
Endocrinology and Metabolism.2021; 36(6): 1201. CrossRef
- Myosteatosis is associated with poor survival after kidney transplantation: a large retrospective cohort validation

- Clinical Study
- Gender-Dependent Reference Range of Serum Calcitonin Levels in Healthy Korean Adults
- Eyun Song, Min Ji Jeon, Hye Jin Yoo, Sung Jin Bae, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Hong-Kyu Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(2):365-373. Published online April 7, 2021
- DOI: https://doi.org/10.3803/EnM.2020.939

- 5,069 View
- 152 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Serum calcitonin measurement contains various clinical and methodological aspects. Its reference level is wide and unclear despite sensitive calcitonin kits are available. This study aimed to identify the specific reference range in the healthy Korean adults.
Methods
Subjects were ≥20 years with available calcitonin (measured by a two-site immunoradiometric assay) data by a routine health checkup. Three groups were defined as all eligible subjects (group 1, n=10,566); subjects without self or family history of thyroid disease (group 2, n=5,152); and subjects without chronic kidney disease, autoimmune thyroid disease, medication of proton pump inhibitor/H2 blocker/steroid, or other malignancies (group 3, n=4,638).
Results
This study included 6,341 male and 4,225 female subjects. Males had higher mean calcitonin than females (2.3 pg/mL vs. 1.9 pg/mL, P<0.001) in group 1. This gender difference remained similar in groups 2 and 3. Calcitonin according to age or body mass index was not significant in both genders. Higher calcitonin in smoking than nonsmoking men was observed but not in women. Sixty-nine subjects had calcitonin higher than the upper reference limit (10 pg/mL) and 64 of them had factors associated with hypercalcitoninemia besides medullary thyroid cancer. Our study suggests the reference intervals for men who were non, ex-, current smokers, and women (irrespective of smoking status) as <5.7, <7.1, <7.9, and <3.6 pg/mL, respectively.
Conclusion
Specific calcitonin reference range should be provided considering for sex and smoking status. Taking account for several factors known to induce hypercalcitoninemia can help interpret the gray zone of moderately elevated calcitonin. -
Citations
Citations to this article as recorded by- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma
Pierpaolo Trimboli, Giuseppe Peloni, Dorotea Confalonieri, Elena Gamarra, Tommaso Piticchio, Francesco Frasca, Petra Makovac, Arnoldo Piccardo, Lorenzo Ruinelli
Frontiers in Oncology.2024;[Epub] CrossRef - Surgical treatment of solid variant of papillary thyroid carcinoma: Fifteen-year experience of a tertiary center
Katarina Tausanović, Marina Stojanović, Milan Jovanović, Boban Stepanović, Jovan Ilić, Sara Ivaniš, Vladan Živaljević
Medicinska istrazivanja.2024; 57(1): 121. CrossRef - Some genetic differences in patients with rheumatoid arthritis
Hosam M. Ahmad, Zaki M. Zaki, Asmaa S. Mohamed, Amr E. Ahmed
BMC Research Notes.2023;[Epub] CrossRef - Presence or severity of Hashimoto’s thyroiditis does not influence basal calcitonin levels: observations from CROHT biobank
M. Cvek, A. Punda, M. Brekalo, M. Plosnić, A. Barić, D. Kaličanin, L. Brčić, M. Vuletić, I. Gunjača, V. Torlak Lovrić, V. Škrabić, V. Boraska Perica
Journal of Endocrinological Investigation.2022; 45(3): 597. CrossRef - Environmental Factors That Affect Parathyroid Hormone and Calcitonin Levels
Mirjana Babić Leko, Nikolina Pleić, Ivana Gunjača, Tatijana Zemunik
International Journal of Molecular Sciences.2021; 23(1): 44. CrossRef
- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma

Brief Reports
- Hypothalamus and Pituitary gland
- Reference Ranges of Serum Insulin-Like Growth Factor-I and Insulin-Like Growth Factor Binding Protein-3: Results from a Multicenter Study in Healthy Korean Adults
- In-Kyung Jeong, Jong Kyu Byun, Junghyun Noh, Sang Wan Kim, Yoon-Sok Chung, Tae Sun Park, Sung-Woon Kim
- Endocrinol Metab. 2020;35(4):954-959. Published online December 1, 2020
- DOI: https://doi.org/10.3803/EnM.2020.785
- 4,450 View
- 125 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
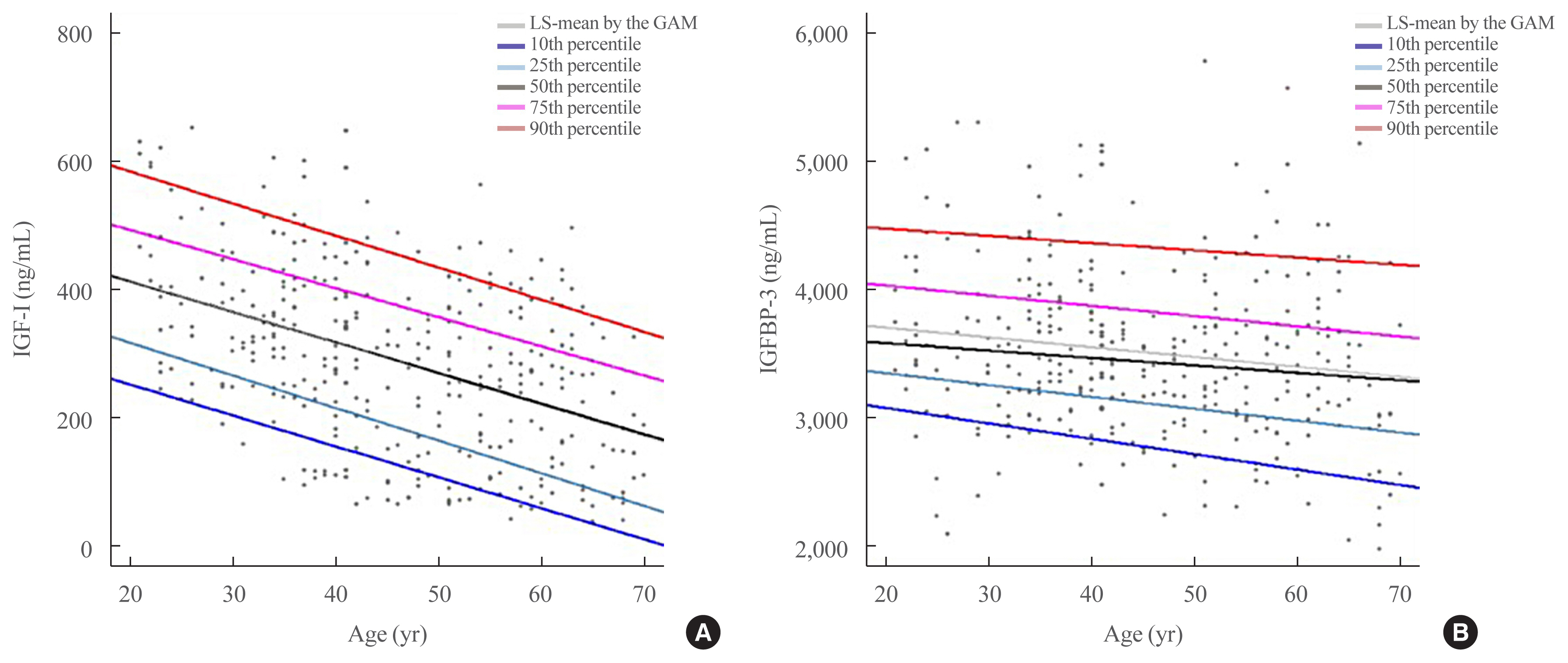
ePub - Insulin-like growth factor-I (IGF-I) plays a pivotal role in the diagnosis and treatment of growth hormone (GH) excess or deficiency. The GH study group of the Korean Endocrine Society aims to establish the Korean reference ranges of serum IGF-I and insulin-like growth factor binding protein-3 (IGFBP-3) and assess the relationship between IGF-I and IGFBP-3 and clinical parameters. Fasting serum was collected from healthy Korean adults at health promotion centers of five hospitals nationwide. Serum IGF-I and IGFBP-3 were measured via an immunoradiometric assay using a DSL kit (Diagnostic Systems Laboratories). Serum samples from 354 subjects (180 male, 174 female) were analyzed based on sex at 10-year intervals from 21 to 70 years. IGF-I levels were inversely correlated with age. After adjustment of age, the IGF-I/IGFBP-3 ratio was significantly negatively associated with blood pressure and free thyroxine and positively associated with weight, hemoglobin, creatinine, alanine transferase, fasting glucose, and thyroid stimulating hormone. Therefore, age- and sex-specific reference ranges of serum IGF-I and IGFBP-3 can be efficient in evaluating GH excess or deficiency in Korean population.
-
Citations
Citations to this article as recorded by- Capillary blood as a complementary matrix for doping control purposes. Application to the definition of the individual longitudinal profile of IGF-1
Carlotta Stacchini, Francesco Botrè, Xavier de la Torre, Monica Mazzarino
Journal of Pharmaceutical and Biomedical Analysis.2023; 227: 115274. CrossRef
- Capillary blood as a complementary matrix for doping control purposes. Application to the definition of the individual longitudinal profile of IGF-1

- Hypothalamus and Pituitary gland
- Establishment of Reference Intervals for Serum Insulin-Like Growth Factor I in Korean Adult Population
- Boyeon Kim, Yonggeun Cho, Cheol Ryong Ku, Sang-Guk Lee, Kyung-A Lee, Jeong-Ho Kim
- Endocrinol Metab. 2020;35(4):960-964. Published online November 20, 2020
- DOI: https://doi.org/10.3803/EnM.2020.732

- 4,809 View
- 107 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Appropriate reference intervals of serum insulin-like growth factor I (IGF-I) is important for diagnosing and monitoring patients with growth hormone-related diseases. To establish reference intervals, adult individuals (n=1,334, 680 men and 654 women) were divided into six age groups (20–29, 30–39, 40–49, 50–59, 60–69, ≥70). Serum IGF-I was measured by chemiluminescence immunoassay (Liaison). Concordance of patient classification based on reference intervals, manufacturer’s intervals, and standard deviation score (SDS) was evaluated. New reference intervals had higher upper and lower limits than those specified by the manufacturer. The agreement between classification using new reference interval and the manufacturer’s reference interval, and that using new reference interval and SDS was 75.0% (weighted kappa, 0.17), 91.9% (weighted kappa, 0.51) in men and 91.0% (weighted kappa, 0.41), 92.5% (weighted kappa, 0.53) in women, respectively. Reference intervals should be established not only based on age and sex, but also on ethnicity and assay method.
-
Citations
Citations to this article as recorded by- Challenges of insulin-like growth factor-1 testing
Rongrong Huang, Junyan Shi, Ruhan Wei, Jieli Li
Critical Reviews in Clinical Laboratory Sciences.2024; : 1. CrossRef - Male idiopathic hypogonadotropic hypogonadism: Serum insulin-like growth factor-1 and oestradiol levels
Nastaran Salehisedeh, Amir Parhizkar, Parichehreh Yaghmaei, Marjan Sabbaghian
Journal of Human Reproductive Sciences.2022; 15(4): 351. CrossRef - Revisiting the Role of Insulin-like Growth Factor-1 Measurement After Surgical Treatment of Acromegaly
In-Ho Jung, Seonah Choi, Cheol Ryong Ku, Sang-Guk Lee, Eun Jig Lee, Sun Ho Kim, Eui Hyun Kim
The Journal of Clinical Endocrinology & Metabolism.2021; 106(7): e2589. CrossRef
- Challenges of insulin-like growth factor-1 testing


 KES
KES

 First
First Prev
Prev



