Search
- Page Path
- HOME > Search
- Miscellaneous
- Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
- Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
- Endocrinol Metab. 2023;38(6):619-630. Published online November 21, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1814
- 2,457 View
- 111 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
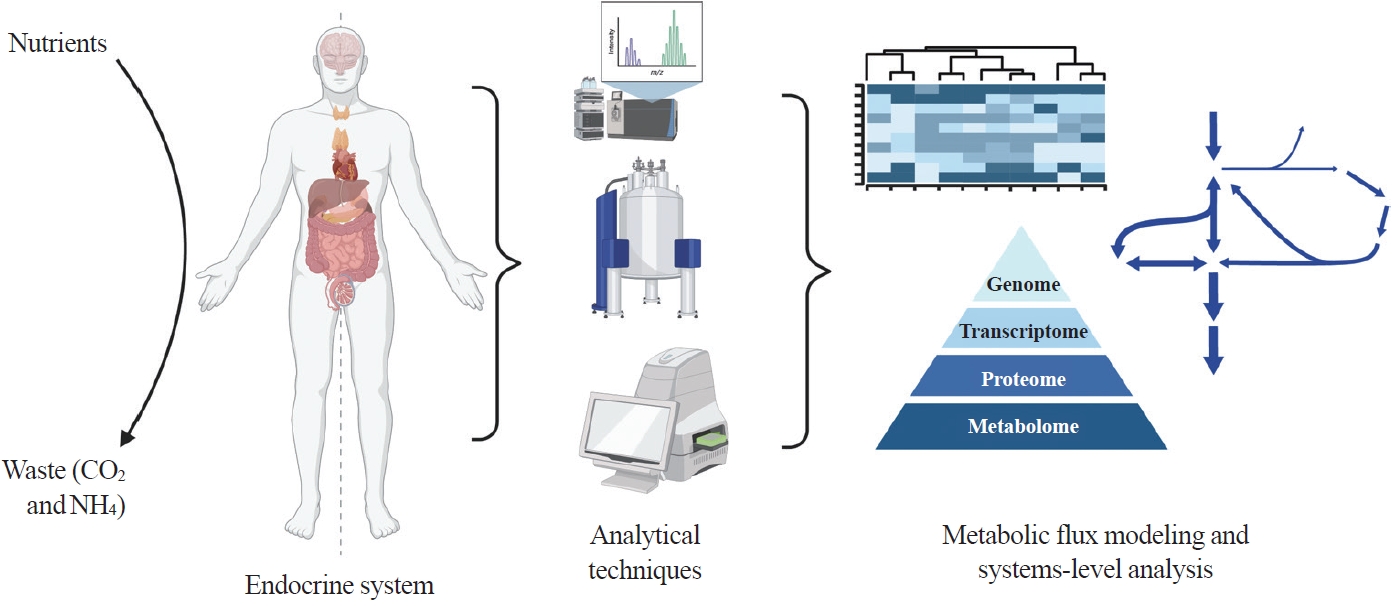
ePub - Metabolism is a dynamic network of biochemical reactions that support systemic homeostasis amidst changing nutritional, environmental, and physical activity factors. The circulatory system facilitates metabolite exchange among organs, while the endocrine system finely tunes metabolism through hormone release. Endocrine disorders like obesity, diabetes, and Cushing’s syndrome disrupt this balance, contributing to systemic inflammation and global health burdens. They accompany metabolic changes on multiple levels from molecular interactions to individual organs to the whole body. Understanding how metabolic fluxes relate to endocrine disorders illuminates the underlying dysregulation. Cancer is increasingly considered a systemic disorder because it not only affects cells in localized tumors but also the whole body, especially in metastasis. In tumorigenesis, cancer-specific mutations and nutrient availability in the tumor microenvironment reprogram cellular metabolism to meet increased energy and biosynthesis needs. Cancer cachexia results in metabolic changes to other organs like muscle, adipose tissue, and liver. This review explores the interplay between the endocrine system and systems-level metabolism in health and disease. We highlight metabolic fluxes in conditions like obesity, diabetes, Cushing’s syndrome, and cancers. Recent advances in metabolomics, fluxomics, and systems biology promise new insights into dynamic metabolism, offering potential biomarkers, therapeutic targets, and personalized medicine.
-
Citations
Citations to this article as recorded by- Editorial: Tumor metabolism and programmed cell death
Dan-Lan Pu, Qi-Nan Wu
Frontiers in Endocrinology.2024;[Epub] CrossRef
- Editorial: Tumor metabolism and programmed cell death

- Adrenal Gland
- Clinical and Molecular Characteristics of PRKACA L206R Mutant Cortisol-Producing Adenomas in Korean Patients
- Insoon Jang, Su-jin Kim, Ra-Young Song, Kwangsoo Kim, Seongmin Choi, Jang-Seok Lee, Min-Kyeong Gwon, Moon Woo Seong, Kyu Eun Lee, Jung Hee Kim
- Endocrinol Metab. 2021;36(6):1287-1297. Published online December 2, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1217

- 3,888 View
- 127 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
An activating mutation (c.617A>C/p.Lys206Arg, L206R) in protein kinase cAMP-activated catalytic subunit alpha (PRKACA) has been reported in 35% to 65% of cases of cortisol-producing adenomas (CPAs). We aimed to compare the clinical characteristics and transcriptome analysis between PRKACA L206R mutants and wild-type CPAs in Korea.
Methods
We included 57 subjects with CPAs who underwent adrenalectomy at Seoul National University Hospital. Sanger sequencing for PRKACA was conducted in 57 CPA tumor tissues. RNA sequencing was performed in 13 fresh-frozen tumor tissues.
Results
The prevalence of the PRKACA L206R mutation was 51% (29/57). The mean age of the study subjects was 42±12 years, and 87.7% (50/57) of the patients were female. Subjects with PRKACA L206R mutant CPAs showed smaller adenoma size (3.3±0.7 cm vs. 3.8±1.2 cm, P=0.059) and lower dehydroepiandrosterone sulfate levels (218±180 ng/mL vs. 1,511±3,307 ng/mL, P=0.001) than those with PRKACA wild-type CPAs. Transcriptome profiling identified 244 differentially expressed genes (DEGs) between PRKACA L206R mutant (n=8) and wild-type CPAs (n=5), including five upregulated and 239 downregulated genes in PRKACA L206R mutant CPAs (|fold change| ≥2, P<0.05). Among the upstream regulators of DEGs, CTNNB1 was the most significant transcription regulator. In several pathway analyses, the Wnt signaling pathway was downregulated and the steroid biosynthesis pathway was upregulated in PRKACA mutants. Protein-protein interaction analysis also showed that PRKACA downregulates Wnt signaling and upregulates steroid biosynthesis.
Conclusion
The PRKACA L206R mutation in CPAs causes high hormonal activity with a limited proliferative capacity, as supported by transcriptome profiling.

- Adrenal Gland
- Metabolic Subtyping of Adrenal Tumors: Prospective Multi-Center Cohort Study in Korea
- Eu Jeong Ku, Chaelin Lee, Jaeyoon Shim, Sihoon Lee, Kyoung-Ah Kim, Sang Wan Kim, Yumie Rhee, Hyo-Jeong Kim, Jung Soo Lim, Choon Hee Chung, Sung Wan Chun, Soon-Jib Yoo, Ohk-Hyun Ryu, Ho Chan Cho, A Ram Hong, Chang Ho Ahn, Jung Hee Kim, Man Ho Choi
- Endocrinol Metab. 2021;36(5):1131-1141. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1149
- 5,100 View
- 209 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
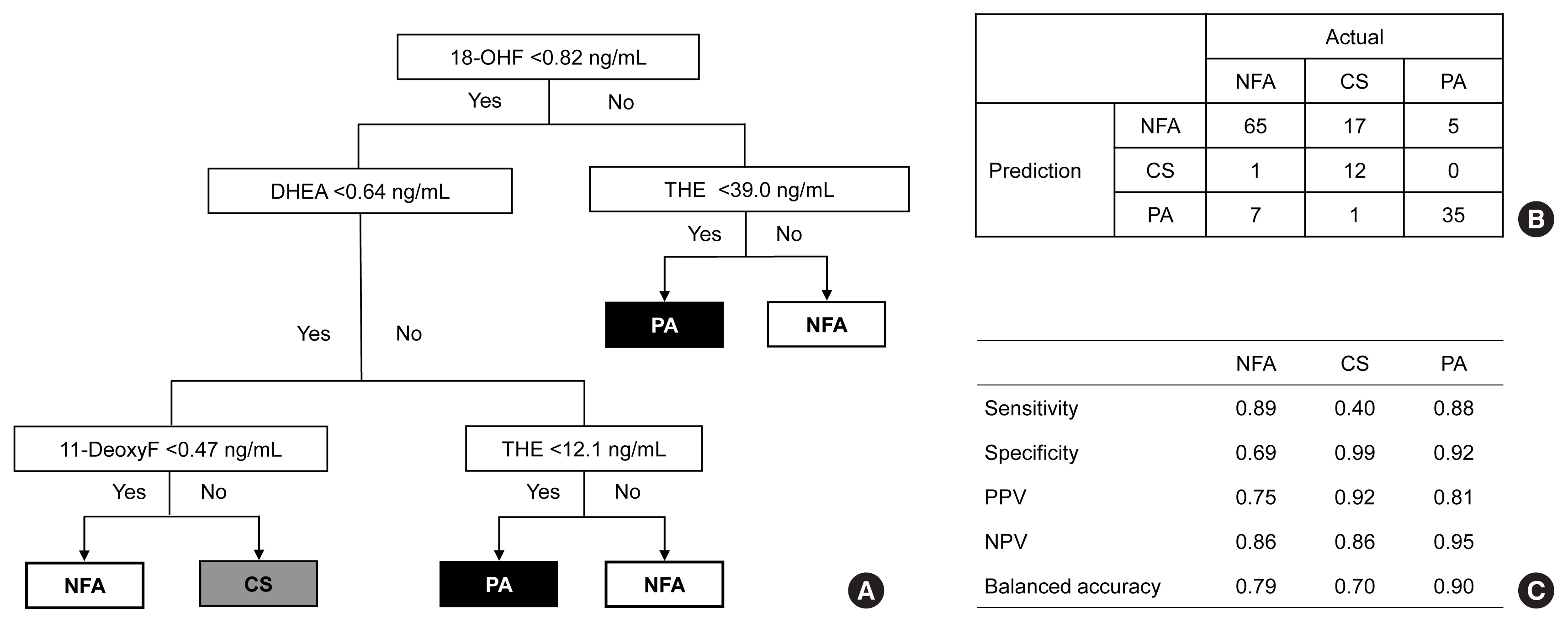
Conventional diagnostic approaches for adrenal tumors require multi-step processes, including imaging studies and dynamic hormone tests. Therefore, this study aimed to discriminate adrenal tumors from a single blood sample based on the combination of liquid chromatography-mass spectrometry (LC-MS) and machine learning algorithms in serum profiling of adrenal steroids.
Methods
The LC-MS-based steroid profiling was applied to serum samples obtained from patients with nonfunctioning adenoma (NFA, n=73), Cushing’s syndrome (CS, n=30), and primary aldosteronism (PA, n=40) in a prospective multicenter study of adrenal disease. The decision tree (DT), random forest (RF), and extreme gradient boost (XGBoost) were performed to categorize the subtypes of adrenal tumors.
Results
The CS group showed higher serum levels of 11-deoxycortisol than the NFA group, and increased levels of tetrahydrocortisone (THE), 20α-dihydrocortisol, and 6β-hydroxycortisol were found in the PA group. However, the CS group showed lower levels of dehydroepiandrosterone (DHEA) and its sulfate derivative (DHEA-S) than both the NFA and PA groups. Patients with PA expressed higher serum 18-hydroxycortisol and DHEA but lower THE than NFA patients. The balanced accuracies of DT, RF, and XGBoost for classifying each type were 78%, 96%, and 97%, respectively. In receiver operating characteristics (ROC) analysis for CS, XGBoost, and RF showed a significantly greater diagnostic power than the DT. However, in ROC analysis for PA, only RF exhibited better diagnostic performance than DT.
Conclusion
The combination of LC-MS-based steroid profiling with machine learning algorithms could be a promising one-step diagnostic approach for the classification of adrenal tumor subtypes. -
Citations
Citations to this article as recorded by- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks
Nathan Mullen, James Curneen, Padraig T Donlon, Punit Prakash, Irina Bancos, Mark Gurnell, Michael C Dennedy
Endocrine Reviews.2024; 45(1): 125. CrossRef - Steroid profiling in adrenal disease
Danni Mu, Dandan Sun, Xia Qian, Xiaoli Ma, Ling Qiu, Xinqi Cheng, Songlin Yu
Clinica Chimica Acta.2024; 553: 117749. CrossRef - Serum and hair steroid profiles in patients with nonfunctioning pituitary adenoma undergoing surgery: A prospective observational study
Seung Shin Park, Yong Hwy Kim, Ho Kang, Chang Ho Ahn, Dong Jun Byun, Man Ho Choi, Jung Hee Kim
The Journal of Steroid Biochemistry and Molecular Biology.2023; 230: 106276. CrossRef - Recent Updates on the Management of Adrenal Incidentalomas
Seung Shin Park, Jung Hee Kim
Endocrinology and Metabolism.2023; 38(4): 373. CrossRef - LC-MS based simultaneous profiling of adrenal hormones of steroids, catecholamines, and metanephrines
Jongsung Noh, Chaelin Lee, Jung Hee Kim, Seung Woon Myung, Man Ho Choi
Journal of Lipid Research.2023; 64(11): 100453. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef - Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
Endocrinology and Metabolism.2023; 38(6): 619. CrossRef - Prevalence and Characteristics of Adrenal Tumors in an Unselected Screening Population
Ying Jing, Jinbo Hu, Rong Luo, Yun Mao, Zhixiao Luo, Mingjun Zhang, Jun Yang, Ying Song, Zhengping Feng, Zhihong Wang, Qingfeng Cheng, Linqiang Ma, Yi Yang, Li Zhong, Zhipeng Du, Yue Wang, Ting Luo, Wenwen He, Yue Sun, Fajin Lv, Qifu Li, Shumin Yang
Annals of Internal Medicine.2022; 175(10): 1383. CrossRef
- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks

- Miscellanenous
- Cushing Syndrome Associated Myopathy: It Is Time for a Change
- Martin Reincke
- Endocrinol Metab. 2021;36(3):564-571. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1069
- 4,781 View
- 174 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
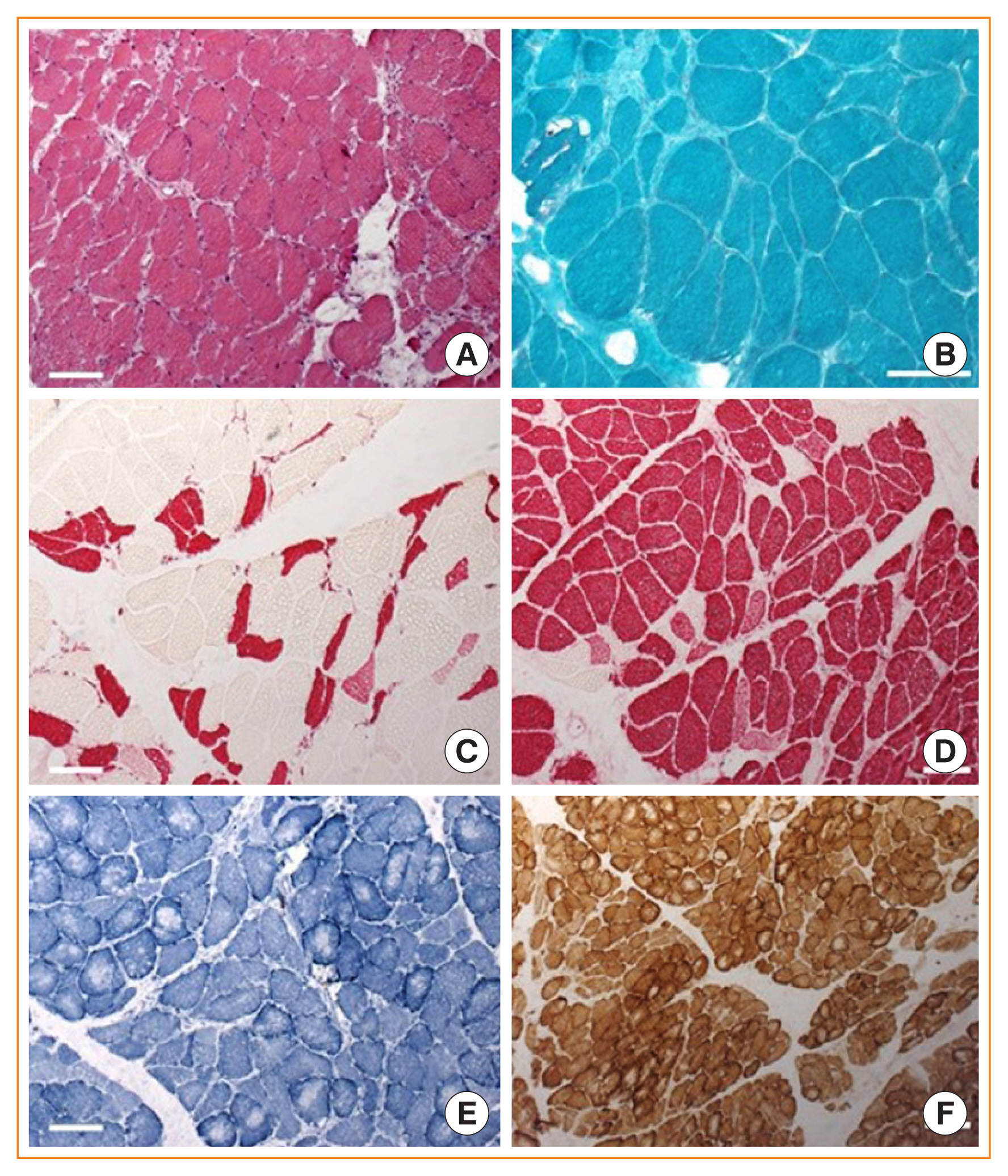
ePub - Cushing syndrome is the result of excessive levels of glucocorticoids. Endogenous Cushing syndrome is rare with an incidence of two to three cases per million per year. Clinically, the presentation consists of a characteristic phenotype including skin symptoms and metabolic manifestations. A frequent co-morbidity with high impact on quality of life is Cushing syndrome associated myopathy. It characteristically affects the proximal myopathy, impairing stair climbing and straightening up. The pathophysiology is complex and involves protein degradation via the forkhead box O3 (FOXO3) pathway, intramuscular fat accumulation, and inactivity-associated muscle atrophy. Surgical remission of Cushing syndrome is the most important step for recovery of muscle function. Restoration depends on age, co-morbidities and postoperative insulin-like growth factor concentrations. At average, functionality remains impaired during the long-term compared to age and sex matched control persons. Growth hormone therapy in individuals with impaired growth hormone secretion could be an option but has not been proved in a randomized trial.
-
Citations
Citations to this article as recorded by- Long-Term Consequences of Cushing Syndrome: A Systematic Literature Review
Soraya Puglisi, Anna Maria Elena Perini, Cristina Botto, Francesco Oliva, Massimo Terzolo
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e901. CrossRef - The Link between Mitochondrial Dysfunction and Sarcopenia: An Update Focusing on the Role of Pyruvate Dehydrogenase Kinase 4
Min-Ji Kim, Ibotombi Singh Sinam, Zerwa Siddique, Jae-Han Jeon, In-Kyu Lee
Diabetes & Metabolism Journal.2023; 47(2): 153. CrossRef - Intelligent Systems for Muscle Tracking: A Review on Sensor‐Algorithm Synergy
Arjun Putcha, Tien Nguyen, Regina Smith, Rachel Choffin, Wubin Bai
Advanced Intelligent Systems.2023;[Epub] CrossRef - Sarcopenia in youth
Han Na Jung, Chang Hee Jung, You-Cheol Hwang
Metabolism.2023; 144: 155557. CrossRef - Cushing Syndrome
Martin Reincke, Maria Fleseriu
JAMA.2023; 330(2): 170. CrossRef - Musculoskeletal complications of Cushing syndrome
Dorota Leszczyńska, Alicja Szatko, Lucyna Papierska, Wojciech Zgliczyński, Piotr Glinicki
Rheumatology.2023; 61(4): 271. CrossRef - Circulating myomiRNAs as biomarkers in patients with Cushing’s syndrome
C. Pivonello, R. Patalano, C. Simeoli, T. Montò, M. Negri, F. Amatrudo, N. Di Paola, A. Larocca, E. M. Crescenzo, R. Pirchio, D. Solari, C. de Angelis, R. S. Auriemma, L. M. Cavallo, A. Colao, R. Pivonello
Journal of Endocrinological Investigation.2023; 47(3): 655. CrossRef - Low-grade inflammation during the glucocorticoid withdrawal phase in patients with Cushing's syndrome
Frederick Vogel, Leah Braun, Stephanie Zopp, Elisabeth Nowak, Jochen Schreiner, Irina Benz, German Rubinstein, Heike Künzel, Katrin Ritzel, Matthias Kroiss, Jürgen Honegger, Felix Beuschlein, Katharina Schilbach, Daniel Teupser, Martin Bidlingmaier, Marti
European Journal of Endocrinology.2023; 188(4): 375. CrossRef - An odd case of immune-mediated necrotizing myopathy, complicated with sagittal, transverse and sigmoid sinus thrombosis
Andreea Trandafir, Violeta Claudia Bonjincă, Delia Tulba, Gelu Onose
Balneo and PRM Research Journal.2023; 14(Vol.14, no): 630. CrossRef - Morbidität und Mortalität beim Cushing-Syndrom
Frederick Vogel, Leah Braun, Martin Reincke
Der Internist.2022; 63(1): 34. CrossRef - Pathophysiology of Mild Hypercortisolism: From the Bench to the Bedside
Vittoria Favero, Arianna Cremaschi, Chiara Parazzoli, Alberto Falchetti, Agostino Gaudio, Luigi Gennari, Alfredo Scillitani, Fabio Vescini, Valentina Morelli, Carmen Aresta, Iacopo Chiodini
International Journal of Molecular Sciences.2022; 23(2): 673. CrossRef - Long‐term morbidity and mortality in patients with Cushing's syndrome
Leah T. Braun, Frederick Vogel, Martin Reincke
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Clinical presentation and etiology of Cushing's syndrome: Data from ERCUSYN
Elena Valassi
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Pyruvate dehydrogenase kinase 4 promotes ubiquitin–proteasome system‐dependent muscle atrophy
Ibotombi Singh Sinam, Dipanjan Chanda, Themis Thoudam, Min‐Ji Kim, Byung‐Gyu Kim, Hyeon‐Ji Kang, Jung Yi Lee, Seung‐Hoon Baek, Shin‐Yoon Kim, Bum Jin Shim, Dongryeol Ryu, Jae‐Han Jeon, In‐Kyu Lee
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(6): 3122. CrossRef - Consensus on diagnosis and management of Cushing's disease: a guideline update
Maria Fleseriu, Richard Auchus, Irina Bancos, Anat Ben-Shlomo, Jerome Bertherat, Nienke R Biermasz, Cesar L Boguszewski, Marcello D Bronstein, Michael Buchfelder, John D Carmichael, Felipe F Casanueva, Frederic Castinetti, Philippe Chanson, James Findling
The Lancet Diabetes & Endocrinology.2021; 9(12): 847. CrossRef
- Long-Term Consequences of Cushing Syndrome: A Systematic Literature Review

- Adrenal gland
- Is Follow-up of Adrenal Incidentalomas Always Mandatory?
- Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
- Endocrinol Metab. 2020;35(1):26-35. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.26
- 6,472 View
- 250 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
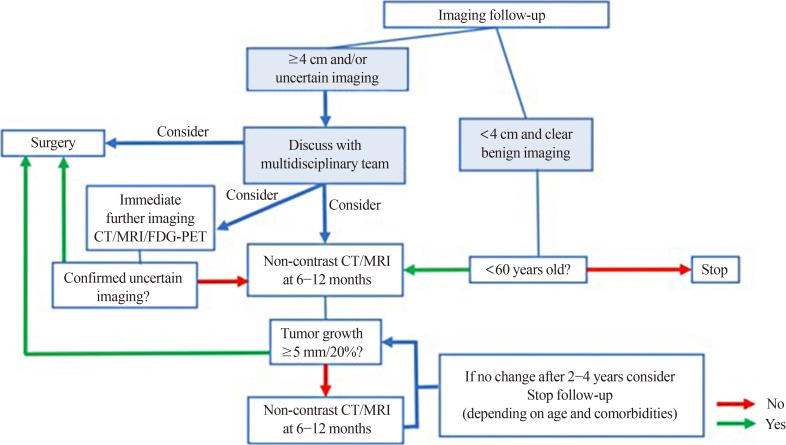
ePub Adrenal masses are mainly detected unexpectedly by an imaging study performed for reasons unrelated to any suspect of adrenal diseases. Such masses are commonly defined as “adrenal incidentalomas” and represent a public health challenge because they are increasingly recognized in current medical practice. Management of adrenal incidentalomas is currently matter of debate. Although there is consensus on the need of a multidisciplinary expert team evaluation and surgical approach in patients with significant hormonal excess and/or radiological findings suspicious of malignancy demonstrated at the diagnosis or during follow-up, the inconsistency between official guidelines and the consequent diffuse uncertainty on management of small adrenal incidentalomas still represents a considerable problem in terms of clinical choices in real practice. The aim of the present work is to review the proposed strategies on how to manage patients with adrenal incidentalomas that are not candidates to immediate surgery. The recent European Society of Endocrinology/European Network for the Study of Adrenal Tumors guidelines have supported the view to avoid surveillance in patients with clear benign adrenal lesions <4 cm and/or without any hormonal secretion; however, newer prospective studies are needed to confirm safety of this strategy, in particular in younger patients.
-
Citations
Citations to this article as recorded by- Adrenal Incidentaloma—Innocent Bystander or Intruder?
Laurence Amar, Inga Harbuz-Miller, Adina F Turcu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1303. CrossRef - Diagnosing and managing adrenal incidentalomas
Justine Herndon, Irina Bancos
JAAPA.2023; 36(5): 12. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - The Role of Biomarkers in Adrenocortical Carcinoma: A Review of Current Evidence and Future Perspectives
Maja Mizdrak, Tina Tičinović Kurir, Joško Božić
Biomedicines.2021; 9(2): 174. CrossRef - An Adrenocortical Carcinoma Evolving After Nine Years of Latency From a Small Adrenal Incidentaloma
Harpreet S Kohli, Sukesh Manthri, Shikha Jain, Rahul Kashyap, Sheng Chen, Thoyaja Koritala, Aysun Tekin, Ramesh Adhikari, Raghavendra Tirupathi, Aram Barbaryan, Simon Zec, Hanyin Wang, Stephanie Welle, Pavan Devulapally, Mack Sheraton, Manpreet Kaur, Vish
Cureus.2021;[Epub] CrossRef - Diagnostic algorithm of the subclinical forms of adrenal neoplasms
Sofya G. Blyumina, Pavel N. Romashchenko, Igor S. Zheleznyak
Bulletin of the Russian Military Medical Academy.2021; 23(3): 67. CrossRef
- Adrenal Incidentaloma—Innocent Bystander or Intruder?

- Adrenal gland
- An Ectopic Cortisol-Producing Adrenocortical Adenoma Masquerading as a Liposarcoma in the Pararenal Space
- Sunyoung Kang, Seung Shin Park, Jae Hyun Bae, Kyu Eun Lee, Jung Hee Kim, Chan Soo Shin
- Endocrinol Metab. 2018;33(3):423-424. Published online August 14, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.423
- 2,834 View
- 43 Download

- Adrenal gland
- Recent Updates on the Diagnosis and Management of Cushing's Syndrome
- Lynnette K. Nieman
- Endocrinol Metab. 2018;33(2):139-146. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.139
- 11,980 View
- 742 Download
- 50 Web of Science
- 48 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Cushing's syndrome, a potentially lethal disorder characterized by endogenous hypercortisolism, may be difficult to recognize, especially when it is mild and the presenting features are common in the general population. However, there is a need to identify the condition at an early stage, as it tends to progress, accruing additional morbidity and increasing mortality rates. Once a clinical suspicion is raised, screening tests involve timed measurement of urine, serum or salivary cortisol at baseline or after administration of dexamethasone, 1 mg. Each test has caveats, so that the choice of tests must be individualized for each patient. Once the diagnosis is established, and the cause is determined, surgical resection of abnormal tumor/tissue is the optimal treatment. When this cannot be achieved, medical treatment (or bilateral adrenalectomy) must be used to normalize cortisol production. Recent updates in screening for and treating Cushing's syndrome are reviewed here.
-
Citations
Citations to this article as recorded by- Steroid as a Saviour and Culprit in Pemphigus Vulgaris Therapy: A Rare
Case Series
Deepthi Avvaru, Raushan Kumar Chaudhary, Bhavana Doshi, Ramesh Bhandari
Current Drug Therapy.2024; 19(3): 360. CrossRef - Considerations for cutaneous physiologic changes of pregnancy that fail to resolve postpartum
Madison J. Anzelc, Mark A. Bechtel
International Journal of Dermatology.2023; 62(2): 190. CrossRef - Hypertension in Turner syndrome: a review of proposed mechanisms, management and new directions
Lily Jones, Joanne Blair, Daniel B. Hawcutt, Gregory Y.H. Lip, Alena Shantsila
Journal of Hypertension.2023; 41(2): 203. CrossRef - Methyl-Prednisolone and Betamethasone Induced Iatrogenic Cushing Syndrome - A Rare Case Report
Faaiz Khan, Jumana Hakeem, Mitta Raghavendra, Sushanta Kumar Das, Vallala Venakata Rajesham, Tadikonda Rama Rao
International Journal of Pharmaceutical Research and Allied Sciences.2023; 12(2): 40. CrossRef - Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
Endocrinology and Metabolism.2023; 38(6): 619. CrossRef - Metabolic profile differences in ACTH‐dependent and ACTH‐independent Cushing syndrome
Zhengyang Li, Chen Zhang, Chong Geng, Yongfeng Song
Chronic Diseases and Translational Medicine.2022; 8(1): 36. CrossRef - Stressing the need for validated measures of cortisol in HIV research: A scoping review
Shayda A. Swann, Elizabeth M. King, Hélène C. F. Côté, Melanie C. M. Murray
HIV Medicine.2022; 23(8): 880. CrossRef - Concomitant coexistence of ACTH‐dependent and independent Cushing syndrome
Ach Taieb, Saad Ghada, Gorchène Asma, Ben Abdelkrim Asma, Kacem Maha, Ach Koussay
Clinical Case Reports.2022;[Epub] CrossRef - Incretin Response to Mixed Meal Challenge in Active Cushing’s Disease and after Pasireotide Therapy
Mattia Barbot, Alessandro Mondin, Daniela Regazzo, Valentina Guarnotta, Daniela Basso, Carla Giordano, Carla Scaroni, Filippo Ceccato
International Journal of Molecular Sciences.2022; 23(9): 5217. CrossRef - Intermittent Blurry Vision: An Unexpected Presentation of Cushing’s Syndrome Due to Primary Bilateral Macronodular Adrenal Hyperplasia (PBMAH)
Christopher Fernandez, Smriti Bhatia, Ariana Rucker, Lee Celio
Cureus.2022;[Epub] CrossRef - Recurrent Metatarsal Fractures in a Patient With Cushing Disease: A Case Report
Jose Iturregui, Glenn Shi
Cureus.2022;[Epub] CrossRef - Recognising and diagnosing Cushing’s syndrome in primary care: challenging but not impossible
Kate Scoffings, Damian Morris, Andrew Pullen, Sharon Temple, Anna Trigell, Mark Gurnell
British Journal of General Practice.2022; 72(721): 399. CrossRef - Recurrent Cushing Syndrome From Metastatic Adrenocortical Carcinoma With Fumarate Hydratase Allelic Variant
Emily Silverman, Noor Addasi, Muaataz Azzawi, Ernesto Martinez Duarte, Dali Huang, Benjamin Swanson, Apar Kishor Ganti, Gwen Reiser, Abbey L. Fingeret, Anupam Kotwal
AACE Clinical Case Reports.2022; 8(6): 259. CrossRef - Multiple Bone Fractures in a Patient With Difficult-to-Treat Cushing’s Disease
Sara Correia, Diogo Ramalho, Gustavo Rocha, Maria J Oliveira
Cureus.2022;[Epub] CrossRef - Management of patients on systemic steroids: An oral surgery perspective
Vikash Patel, Shrina Nathwani, Naomi Rahman
Dental Update.2022; 49(9): 749. CrossRef - Importancia del cateterismo de senos petrosos inferiores en el diagnóstico de síndrome de Cushing, a propósito de un caso
Clara Jiménez García, Paula Sirera Sirera, María Eugenia Torregrosa Quesada, Victoria González Bueno, Rocío Alfayate Guerra
Advances in Laboratory Medicine / Avances en Medicina de Laboratorio.2022; 3(4): 411. CrossRef - Cushing's Syndrome Behind Hypokalemia and Severe Infection: A Case Report
Catarina Elias, Diana Oliveira, Maria Manuel Silva, Patrícia Lourenço
Cureus.2022;[Epub] CrossRef - Relevance of inferior petrosal sinus sampling in the diagnosis of Cushing’s syndrome: a case report
Clara Jiménez García, Paula Sirera Sirera, María Eugenia Torregrosa Quesada, Victoria González Bueno, Rocío Alfayate Guerra
Advances in Laboratory Medicine / Avances en Medicina de Laboratorio.2022; 3(4): 407. CrossRef - Proximal muscle weakness as the sole manifestation of Cushing’s disease, misdiagnosed as dermatomyositis: a case report
Marjan Jeddi, Mesbah Shams
Journal of Medical Case Reports.2022;[Epub] CrossRef - Differences in outcomes of bilateral adrenalectomy in patients with ectopic ACTH producing tumor of known and unknown origin
Thomas Szabo Yamashita, Alaa Sada, Irina Bancos, William F. Young, Benzon M Dy, David R. Farley, Melanie L. Lyden, Geoffrey B. Thompson, Travis J. McKenzie
The American Journal of Surgery.2021; 221(2): 460. CrossRef - A key role for conservative treatment in the management of pituitary apoplexy
Claire Marx, Muriel Rabilloud, Françoise Borson Chazot, Caroline Tilikete, Emmanuel Jouanneau, Gerald Raverot
Endocrine.2021; 71(1): 168. CrossRef - 7-T Magnetic Resonance Imaging in the Management of Brain Tumors
Melanie A. Morrison, Janine M. Lupo
Magnetic Resonance Imaging Clinics of North America.2021; 29(1): 83. CrossRef - Medical therapy in severe hypercortisolism
Júlia Vieira Oberger Marques, Cesar Luiz Boguszewski
Best Practice & Research Clinical Endocrinology & Metabolism.2021; 35(2): 101487. CrossRef - Metabolic changes in serum steroids for diagnosing and subtyping Cushing’s syndrome
Chang Ho Ahn, Chaelin Lee, Jaeyoon Shim, Sung Hye Kong, Su-jin Kim, Yong Hwy Kim, Kyu Eun Lee, Chan Soo Shin, Jung Hee Kim, Man Ho Choi
The Journal of Steroid Biochemistry and Molecular Biology.2021; 210: 105856. CrossRef - Method-Specific Cortisol and Dexamethasone Thresholds Increase Clinical Specificity of the Dexamethasone Suppression Test for Cushing Syndrome
Nora Vogg, Max Kurlbaum, Timo Deutschbein, Benedict Gräsl, Martin Fassnacht, Matthias Kroiss
Clinical Chemistry.2021; 67(7): 998. CrossRef - Untargeted Plasma Metabolomics Unravels a Metabolic Signature for Tissue Sensitivity to Glucocorticoids in Healthy Subjects: Its Implications in Dietary Planning for a Healthy Lifestyle
Nicolas C. Nicolaides, Maria-Konstantina Ioannidi, Eleni Koniari, Ifigeneia Papageorgiou, Anastasia Bartzeliotou, Amalia Sertedaki, Maria I. Klapa, Evangelia Charmandari
Nutrients.2021; 13(6): 2120. CrossRef - Endocrine hypertension secondary to adrenal tumors: clinical course and predictive factors of clinical remission
Uriel Clemente-Gutiérrez, Rafael H. Pérez-Soto, Juan D. Hernández-Acevedo, Nicole M. Iñiguez-Ariza, Enrique Casanueva-Pérez, Juan Pablo Pantoja-Millán, Mauricio Sierra-Salazar, Miguel F. Herrera, David Velázquez-Fernández
Langenbeck's Archives of Surgery.2021; 406(6): 2027. CrossRef - Development of 68Ga DOTA-CRH for PET/CT Imaging of ACTH-Dependent Cushing's Disease: Initial Study
Jaya Shukla, Rakhee Vatsa, Rama Walia, Anupriya Chhabra, Nivedita Rana, Harmandeep Singh, Rajender Kumar, Bhagwant Rai Mittal
Cancer Biotherapy and Radiopharmaceuticals.2021; 36(8): 642. CrossRef - Cushing Syndrome Associated Myopathy: It Is Time for a Change
Martin Reincke
Endocrinology and Metabolism.2021; 36(3): 564. CrossRef - Cushing’s disease presenting with psychosis
Ahmed Saeed Mubarak Mohamed, Ahmed Iqbal, Suveera Prasad, Nigel Hoggard, Daniel Blackburn
Practical Neurology.2021; 21(4): 351. CrossRef - ACTH-independent Cushing's syndrome due to bilateral adrenocortical adenoma: A case report
Majd Sharaf, Rama Al-Saqqa, Mouhammad Kourabi
Radiology Case Reports.2021; 16(11): 3168. CrossRef - A New Clinical Model to Estimate the Pre-Test Probability of Cushing’s Syndrome: The Cushing Score
Mirko Parasiliti-Caprino, Fabio Bioletto, Tommaso Frigerio, Valentina D’Angelo, Filippo Ceccato, Francesco Ferraù, Rosario Ferrigno, Marianna Minnetti, Carla Scaroni, Salvatore Cannavò, Rosario Pivonello, Andrea Isidori, Fabio Broglio, Roberta Giordano, M
Frontiers in Endocrinology.2021;[Epub] CrossRef - Bilateral Adrenalectomy: Differences between Cushing Disease and Ectopic ACTH-Producing Tumors
Thomas Szabo Yamashita, Alaa Sada, Irina Bancos, William F. Young, Benzon M. Dy, David R. Farley, Melanie L. Lyden, Geoffrey B. Thompson, Travis J. McKenzie
Annals of Surgical Oncology.2020; 27(10): 3851. CrossRef - Decision-Making in Artificial Intelligence: Is It Always Correct?
Hun-Sung Kim
Journal of Korean Medical Science.2020;[Epub] CrossRef - Cushing's syndrome: Overview of clinical presentation, diagnostic tools and complications
Mattia Barbot, Marialuisa Zilio, Carla Scaroni
Best Practice & Research Clinical Endocrinology & Metabolism.2020; 34(2): 101380. CrossRef - Cortisol Measurements in Cushing’s Syndrome: Immunoassay or Mass Spectrometry?
Gregori Casals, Felicia Alexandra Hanzu
Annals of Laboratory Medicine.2020; 40(4): 285. CrossRef - Cardiopatías de origen endocrino: una etiología frecuentemente olvidada
Laura Duque-González, Luis Miguel Ruiz-Velásquez, José Luis Torres-Grajales, Mauricio Duque-Ramírez
Medicina y Laboratorio.2020; 24(3): 207. CrossRef - Reference ranges of late-night salivary cortisol and cortisone measured by LC–MS/MS and accuracy for the diagnosis of Cushing’s syndrome
F. Ponzetto, F. Settanni, M. Parasiliti-Caprino, F. Rumbolo, A. Nonnato, M. Ricciardo, E. Amante, G. Priolo, S. Vitali, L. Anfossi, E. Arvat, E. Ghigo, R. Giordano, G. Mengozzi
Journal of Endocrinological Investigation.2020; 43(12): 1797. CrossRef - Assessment of 1 mg Dexamethasone Suppression Test in Patients with Obesity Before Bariatric Surgery
Dilek Gogas Yavuz, Tugce Apaydin, Hatice Gizem Gunhan, Meliha Melin Uygur
Obesity Surgery.2020; 30(12): 4981. CrossRef - Prospective Evaluation of Late-Night Salivary Cortisol and Cortisone by EIA and LC-MS/MS in Suspected Cushing Syndrome
Joshua Kannankeril, Ty Carroll, James W Findling, Bradley Javorsky, Ian L Gunsolus, Jonathan Phillips, Hershel Raff
Journal of the Endocrine Society.2020;[Epub] CrossRef - Infantile Iatrogenic Cushing Syndrome due to Topical Steroids
Lulwah Alkhuder, Horia Mawlawi
Case Reports in Pediatrics.2019; 2019: 1. CrossRef - Synchronous bilateral adrenalectomy in ACTH-dependent hypercortisolism: predictors, biomarkers and outcomes
S. Chiloiro, A. Giampietro, M. Raffaelli, G. D’Amato, C. Bima, L. Lauretti, C. Anile, C. P. Lombardi, G. Rindi, R. Bellantone, L. De Marinis, A. Pontecorvi, A. Bianchi
Endocrine.2019; 66(3): 642. CrossRef - Low-dose etomidate for the management of severe hypercortisolaemia in different clinical scenarios: a case series and review of the literature
Agnieszka Łebek-Szatańska, Karolina M. Nowak, Wojciech Zgliczyński, Elżbieta Baum, Agnieszka Żyłka, Lucyna Papierska
Therapeutic Advances in Endocrinology and Metabolism.2019; 10: 204201881982554. CrossRef - Drug design strategies for Cushing’s syndrome
S. A. Usanov, A. V. Kliuchenovich, N. V. Strushkevich
Expert Opinion on Drug Discovery.2019; 14(2): 143. CrossRef - Pharmacological and analytical interference in hormone assays for diagnosis of adrenal incidentaloma
Antoine-Guy Lopez, François Fraissinet, Herve Lefebvre, Valéry Brunel, Frédéric Ziegler
Annales d'Endocrinologie.2019; 80(4): 250. CrossRef - Emerging Role of USP8, HMGA, and Non-Coding RNAs in Pituitary Tumorigenesis
Daniela D’Angelo, Marco De Martino, Claudio Arra, Alfredo Fusco
Cancers.2019; 11(9): 1302. CrossRef - Glucocorticoid Receptor Antagonist Administration Prevents Adrenal Gland Atrophy in an ACTH-Independent Cushing’s Syndrome Rat Model
Atsushi Yasuda, Toshiro Seki, Yoshie Kametani, Masahiro Koizumi, Natsumi Kitajima, Masayuki Oki, Masami Seki, Takatoshi Kakuta, Masafumi Fukagawa
International Journal of Endocrinology.2019; 2019: 1. CrossRef - Cushing’s Disease
Nishioka, Yamada
Journal of Clinical Medicine.2019; 8(11): 1951. CrossRef
- Steroid as a Saviour and Culprit in Pemphigus Vulgaris Therapy: A Rare
Case Series

- Adrenal gland
- Bone Health in Adrenal Disorders
- Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
- Endocrinol Metab. 2018;33(1):1-8. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.1
- 5,018 View
- 52 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Secondary osteoporosis resulting from specific clinical disorders may be potentially reversible, and thus continuous efforts to find and adequately treat the secondary causes of skeletal fragility are critical to ameliorate fracture risk and to avoid unnecessary treatment with anti-osteoporotic drugs. Among the hyperfunctional adrenal masses, Cushing's syndrome, pheochromocytoma, and primary aldosteronism are receiving particularly great attention due to their high morbidity and mortality mainly by increasing cardiovascular risk. Interestingly, there is accumulating experimental and clinical evidence that adrenal hormones may have direct detrimental effects on bone metabolism as well. Thus, the present review discusses the possibility of adrenal disorders, especially focusing on pheochromocytoma and primary aldosteronism, as secondary causes of osteoporosis.
-
Citations
Citations to this article as recorded by- High Risk of Fractures Within 7 Years of Diagnosis in Asian Patients With Inflammatory Bowel Diseases
Hyung Jin Ahn, Ye-Jee Kim, Ho-Su Lee, Jin Hwa Park, Sung Wook Hwang, Dong-Hoon Yang, Byong Duk Ye, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang, Beom-Jun Kim, Sang Hyoung Park
Clinical Gastroenterology and Hepatology.2022; 20(5): e1022. CrossRef - Change of Computed Tomography-Based Body Composition after Adrenalectomy in Patients with Pheochromocytoma
Yousun Ko, Heeryoel Jeong, Seungwoo Khang, Jeongjin Lee, Kyung Won Kim, Beom-Jun Kim
Cancers.2022; 14(8): 1967. CrossRef - Bone and mineral metabolism in patients with primary aldosteronism: A systematic review and meta-analysis
Anning Wang, Yuhan Wang, Hongzhou Liu, Xiaodong Hu, Jiefei Li, Huaijin Xu, Zhimei Nie, Lingjing Zhang, Zhaohui Lyu
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Entity of Connshing Syndrome: Primary Aldosteronism with Autonomous Cortisol Secretion
Mara Carsote
Diagnostics.2022; 12(11): 2772. CrossRef - Elemental profiling of adrenal adenomas in solid tissue and blood samples by ICP-MS and ICP-OES
Jovana Jagodić, Branislav Rovčanin, Đurđa Krstić, Ivan Paunović, Vladan Živaljević, Dragan Manojlović, Aleksandar Stojsavljević
Microchemical Journal.2021; 165: 106194. CrossRef - Aldosterone Inhibits In Vitro Myogenesis by Increasing Intracellular Oxidative Stress via Mineralocorticoid Receptor
Jin Young Lee, Da Ae Kim, Eunah Choi, Yun Sun Lee, So Jeong Park, Beom-Jun Kim
Endocrinology and Metabolism.2021; 36(4): 865. CrossRef - Epidemiology and Prognosis of Pheochromocytoma/Paraganglioma in Korea: A Nationwide Study Based on the National Health Insurance Service
Jung Hee Kim, Hyemi Moon, Junghyun Noh, Juneyoung Lee, Sin Gon Kim
Endocrinology and Metabolism.2020; 35(1): 157. CrossRef - Pheochromocytoma and paraganglioma: An emerging cause of secondary osteoporosis
Maki Yokomoto-Umakoshi, Hironobu Umakoshi, Tazuru Fukumoto, Yayoi Matsuda, Hiromi Nagata, Masatoshi Ogata, Hisaya Kawate, Takashi Miyazawa, Ryuichi Sakamoto, Yoshihiro Ogawa
Bone.2020; 133: 115221. CrossRef - Spironolactone reduces biochemical markers of bone turnover in postmenopausal women with primary aldosteronism
Christian Adolf, Leah T. Braun, Carmina T. Fuss, Stefanie Hahner, Heike Künzel, Laura Handgriff, Lisa Sturm, Daniel A. Heinrich, Holger Schneider, Martin Bidlingmaier, Martin Reincke
Endocrine.2020; 69(3): 625. CrossRef - Primary Aldosteronism and Bone Metabolism: A Systematic Review and Meta-Analysis
Shaomin Shi, Chunyan Lu, Haoming Tian, Yan Ren, Tao Chen
Frontiers in Endocrinology.2020;[Epub] CrossRef - Understanding and managing secondary osteoporosis
Luciano Colangelo, Federica Biamonte, Jessica Pepe, Cristiana Cipriani, Salvatore Minisola
Expert Review of Endocrinology & Metabolism.2019; 14(2): 111. CrossRef - Evaluation of bone health in patients with adrenal tumors
Shobana Athimulam, Irina Bancos
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(3): 125. CrossRef
- High Risk of Fractures Within 7 Years of Diagnosis in Asian Patients With Inflammatory Bowel Diseases

- Clinical Study
- The Eosinophil Count Tends to Be Negatively Associated with Levels of Serum Glucose in Patients with Adrenal Cushing Syndrome
- Younghak Lee, Hyon-Seung Yi, Hae Ri Kim, Kyong Hye Joung, Yea Eun Kang, Ju Hee Lee, Koon Soon Kim, Hyun Jin Kim, Bon Jeong Ku, Minho Shong
- Endocrinol Metab. 2017;32(3):353-359. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.353
- 7,666 View
- 46 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cushing syndrome is characterized by glucose intolerance, cardiovascular disease, and an enhanced systemic inflammatory response caused by chronic exposure to excess cortisol. Eosinopenia is frequently observed in patients with adrenal Cushing syndrome, but the relationship between the eosinophil count in peripheral blood and indicators of glucose level in patients with adrenal Cushing syndrome has not been determined.
Methods A retrospective study was undertaken of the clinical and laboratory findings of 40 patients diagnosed with adrenal Cushing syndrome at Chungnam National University Hospital from January 2006 to December 2016. Clinical characteristics, complete blood cell counts with white blood cell differential, measures of their endocrine function, description of imaging studies, and pathologic findings were obtained from their medical records.
Results Eosinophil composition and count were restored by surgical treatment of all of the patients with adrenal Cushing disease. The eosinophil count was inversely correlated with serum and urine cortisol, glycated hemoglobin, and inflammatory markers in the patients with adrenal Cushing syndrome.
Conclusion Smaller eosinophil populations in patients with adrenal Cushing syndrome tend to be correlated with higher levels of blood sugar and glycated hemoglobin. This study suggests that peripheral blood eosinophil composition or count may be associated with serum glucose levels in patients with adrenal Cushing syndrome.
-
Citations
Citations to this article as recorded by- Association between Eosinophil Count and Cortisol Concentrations in Equids Admitted in the Emergency Unit with Abdominal Pain
María Villalba-Orero, María Dolores Contreras-Aguilar, Jose Joaquín Cerón, Beatriz Fuentes-Romero, Marta Valero-González, María Martín-Cuervo
Animals.2024; 14(1): 164. CrossRef - Inverse relationship between eosinophil profiles and serum glucose concentration in dogs with naturally occurring hypercortisolism
Jimin Oh, Dohee Lee, Taesik Yun, Yoonhoi Koo, Yeon Chae, Mhan-Pyo Yang, Byeong-Teck Kang, Hakhyun Kim
Domestic Animal Endocrinology.2022; 80: 106727. CrossRef - Serum Cortisol and Its Correlation with Leucocyte Profile and Circulating Lipids in Donkeys (Equus asinus)
Daniela Alberghina, Alessandra Statelli, Vincenzo Monteverde, Irene Vazzana, Giuseppe Cascone, Michele Panzera
Animals.2022; 12(7): 841. CrossRef - Changes in leukocytes and CRP in different stages of major depression
Deepti Singh, Paul C. Guest, Henrik Dobrowolny, Veronika Vasilevska, Gabriela Meyer-Lotz, Hans-Gert Bernstein, Katrin Borucki, Alexandra Neyazi, Bernhard Bogerts, Roland Jacobs, Johann Steiner
Journal of Neuroinflammation.2022;[Epub] CrossRef - HIF1α is a direct regulator of steroidogenesis in the adrenal gland
Deepika Watts, Johanna Stein, Ana Meneses, Nicole Bechmann, Ales Neuwirth, Denise Kaden, Anja Krüger, Anupam Sinha, Vasileia Ismini Alexaki, Luis Gustavo Perez-Rivas, Stefan Kircher, Antoine Martinez, Marily Theodoropoulou, Graeme Eisenhofer, Mirko Peitz
Cellular and Molecular Life Sciences.2021; 78(7): 3577. CrossRef - The Immune System in Cushing’s Syndrome
Valeria Hasenmajer, Emilia Sbardella, Francesca Sciarra, Marianna Minnetti, Andrea M. Isidori, Mary Anna Venneri
Trends in Endocrinology & Metabolism.2020; 31(9): 655. CrossRef
- Association between Eosinophil Count and Cortisol Concentrations in Equids Admitted in the Emergency Unit with Abdominal Pain

- Clinical Study
- The Recovery of Hypothalamic-Pituitary-Adrenal Axis Is Rapid in Subclinical Cushing Syndrome
- Hee Kyung Kim, Jee Hee Yoon, Yun Ah Jeong, Ho-Cheol Kang
- Endocrinol Metab. 2016;31(4):592-597. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.592
- 3,664 View
- 45 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background In subclinical Cushing syndrome (SC), it is assumed that glucocorticoid production is insufficient to cause a clinically recognizable syndrome. Differences in hormonal levels or recovery time of the hypothalamic-pituitary-adrenocortical (HPA) axis after adrenalectomy between patients with overt Cushing syndrome (OC) and SC remain unknown.
Methods Thirty-six patients (10 with OC and 26 with SC) with adrenal Cushing syndrome who underwent adrenalectomy from 2004 to 2014 were reviewed retrospectively. Patients were treated with glucocorticoid after adrenalectomy and were reevaluated every 1 to 6 months using a rapid adrenocorticotropic hormone (ACTH) stimulation test.
Results Levels of basal 24-hour urine free cortisol (UFC), serum cortisol after an overnight dexamethasone suppression test (DST), and serum cortisol and 24-hour UFC after low-dose DST and high-dose DST were all significantly lower in patients with SC compared with OC. Basal ACTH levels showed significantly higher in patients with SC compared with OC. The probability of recovering adrenal function during follow-up differed significantly between patients with OC and SC (
P =0.001), with significant correlations with the degree of preoperative cortisol excess. Patients with OC required a longer duration of glucocorticoid replacement to recover a normal ACTH stimulation test compared with patients with SC (median 17.0 months vs. 4.0 months,P <0.001).Conclusion The HPA axis recovery time after adrenalectomy in patients with SC is rapid and is dependent on the degree of cortisol excess. More precise definition of SC is necessary to achieve a better management of patients and to avoid the risk of under- or over-treatment of SC patients.
-
Citations
Citations to this article as recorded by- Hypothalamic–pituitary–adrenal axis recovery after treatment of Cushing's syndrome
Annemarie Balasko, Karin Zibar Tomsic, Darko Kastelan, Tina Dusek
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Early assessment of postoperative adrenal function is necessary after adrenalectomy for mild autonomous cortisol secretion
Trenton Foster, Irina Bancos, Travis McKenzie, Benzon Dy, Geoffrey Thompson, Melanie Lyden
Surgery.2021; 169(1): 150. CrossRef - Is Prophylactic Steroid Treatment Mandatory for Subclinical Cushing Syndrome After Unilateral Laparoscopic Adrenalectomy?
Dong Wang, Han-zhong Li, Yu-shi Zhang, Liang Wang, Zhi-gang Ji
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2019; 29(1): 31. CrossRef - When to Intervene for Subclinical Cushing's Syndrome
Lily B. Hsieh, Erin Mackinney, Tracy S. Wang
Surgical Clinics of North America.2019; 99(4): 747. CrossRef - Serum Cortisol Levels via Radioimmunoassay vs Liquid Chromatography Mass Spectrophotometry in Healthy Control Subjects and Patients With Adrenal Incidentalomas
Martha K P Huayllas, Brian C Netzel, Ravinder J Singh, Claudio E Kater
Laboratory Medicine.2018;[Epub] CrossRef - Contralateral adrenal width predicts the duration of prolonged post‐surgical steroid replacement for subclinical Cushing syndrome
Masahiro Sugiura, Yusuke Imamura, Koji Kawamura, Satoshi Yamamoto, Tomokazu Sazuka, Kazuyoshi Nakamura, Shinichi Sakamoto, Hidekazu Nagano, Hisashi Koide, Tomoaki Tanaka, Takashi Imamoto, Akira Komiya, Tomohiko Ichikawa
International Journal of Urology.2018; 25(6): 583. CrossRef - Predictability of hypoadrenalism occurrence and duration after adrenalectomy for ACTH-independent hypercortisolism
V. Morelli, L. Minelli, C. Eller-Vainicher, S. Palmieri, E. Cairoli, A. Spada, M. Arosio, I. Chiodini
Journal of Endocrinological Investigation.2018; 41(4): 485. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Hypothalamic–pituitary–adrenal axis recovery after treatment of Cushing's syndrome

- Adrenal gland
- Bilateral Adrenocortical Masses Producing Aldosterone and Cortisol Independently
- Seung-Eun Lee, Jae Hyeon Kim, You-Bin Lee, Hyeri Seok, In Seub Shin, Yeong Hee Eun, Jung-Han Kim, Young Lyun Oh
- Endocrinol Metab. 2015;30(4):607-613. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.607
- 4,112 View
- 46 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader A 31-year-old woman was referred to our hospital with symptoms of hypertension and bilateral adrenocortical masses with no feature of Cushing syndrome. The serum aldosterone/renin ratio was elevated and the saline loading test showed no suppression of the plasma aldosterone level, consistent with a diagnosis of primary hyperaldosteronism. Overnight and low-dose dexamethasone suppression tests showed no suppression of serum cortisol, indicating a secondary diagnosis of subclinical Cushing syndrome. Adrenal vein sampling during the low-dose dexamethasone suppression test demonstrated excess secretion of cortisol from the left adrenal mass. A partial right adrenalectomy was performed, resulting in normalization of blood pressure, hypokalemia, and high aldosterone level, implying that the right adrenal mass was the main cause of the hyperaldosteronism. A total adrenalectomy for the left adrenal mass was later performed, resulting in a normalization of cortisol level. The final diagnosis was bilateral adrenocortical adenomas, which were secreting aldosterone and cortisol independently. This case is the first report of a concurrent cortisol-producing left adrenal adenoma and an aldosterone-producing right adrenal adenoma in Korea, as demonstrated by adrenal vein sampling and sequential removal of adrenal masses.
-
Citations
Citations to this article as recorded by- Different cell compositions and a novel somatic KCNJ5 variant found in a patient with bilateral adrenocortical adenomas secreting aldosterone and cortisol
Liling Zhao, Jinjing Wan, Yujun Wang, Wenjun Yang, Qi Liang, Jinrong Wang, Ping Jin
Frontiers in Endocrinology.2023;[Epub] CrossRef - Adrenal Vein Cortisol to Metanephrine Ratio for Localizing ACTH-Independent Cortisol-Producing Adenoma: A Case Report
Rishi Raj, Philip A Kern, Neelima Ghanta, Edilfavia M Uy, Kamyar Asadipooya
Journal of the Endocrine Society.2021;[Epub] CrossRef - Adrenal Venous Sampling for Subtype Diagnosis of Primary Hyperaldosteronism
Mitsuhide Naruse, Akiyo Tanabe, Koichi Yamamoto, Hiromi Rakugi, Mitsuhiro Kometani, Takashi Yoneda, Hiroki Kobayashi, Masanori Abe, Youichi Ohno, Nobuya Inagaki, Shoichiro Izawa, Masakatsu Sone
Endocrinology and Metabolism.2021; 36(5): 965. CrossRef - Hypercortisolism and primary aldosteronism caused by bilateral adrenocortical adenomas: a case report
Kaiyun Ren, Jia Wei, Qilin Liu, Yuchun Zhu, Nianwei Wu, Ying Tang, Qianrui Li, Qianying Zhang, Yerong Yu, Zhenmei An, Jing Chen, Jianwei Li
BMC Endocrine Disorders.2019;[Epub] CrossRef
- Different cell compositions and a novel somatic KCNJ5 variant found in a patient with bilateral adrenocortical adenomas secreting aldosterone and cortisol

- Clinical Study
- Subclinical Atherosclerosis in Patients with Cushing Syndrome: Evaluation with Carotid Intima-Media Thickness and Ankle-Brachial Index
- Luigi Petramala, D'Elia Lorenzo, Gino Iannucci, Antonio Concistré, Laura Zinnamosca, Cristiano Marinelli, Giuseppe De Vincentis, Antonio Ciardi, Giorgio De Toma, Claudio Letizia
- Endocrinol Metab. 2015;30(4):488-493. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.488
- 3,752 View
- 44 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cushing syndrome (CS) has been described as a killing disease due its cardiovascular complications. In fact, chronic cortisol excess leads to a constellation of complications, including hypertension, hyperglycemia, adiposity, and thromboembolism. The main vascular alteration associated with CS is atherosclerosis.
Methods Aim of this study was to analyze carotid intima-media thickness (cIMT) and ankle-brachial index (ABI), two surrogate markers of subclinical atherosclerosis in a consecutive series of CS patients, compared to patients with essential hypertension (EH) and health subjects (HS).
Results Patients with CS showed a significant increase (
P <0.05) of cIMT (0.89±0.17 mm) compared to EH (0.81±0.16 mm) and HS (0.75±0.4 mm), with a high prevalence of plaque (23%;P <0.03). Moreover, CS patients showed a mean ABI values (1.07±0.02) significantly lower respect to HS (1.12±0.11;P <0.05), and a higher percentage (20%) of pathological values of ABI (≤0.9;P <0.03).Conclusion In conclusion, we confirmed and extended the data of cIMT in CS, and showed that the ABI represent another surrogate marker of subclinical atherosclerosis in this disease.
-
Citations
Citations to this article as recorded by- Micro- and Macrovascular Effects of Inflammation in Peripheral Artery Disease—Pathophysiology and Translational Therapeutic Approaches
Michael Poledniczek, Christoph Neumayer, Christoph W. Kopp, Oliver Schlager, Thomas Gremmel, Alicja Jozkowicz, Michael E. Gschwandtner, Renate Koppensteiner, Patricia P. Wadowski
Biomedicines.2023; 11(8): 2284. CrossRef - Capillary microarchitectural changes in Cushing's syndrome
Tugce Apaydin, Yasemin Yalcinkaya, Can Ilgin, Dilek Gogas Yavuz
Microvascular Research.2022; 141: 104323. CrossRef - Glucocorticoid therapy is a risk factor for cardiovascular diseases
I. S. Dzherieva, N. I. Volkova, I. Y. Davidenko, I. B. Reshetnikov, S. S. Brovkina, S. M. Avakova, Y. V. Tishchenko
Medical Herald of the South of Russia.2022; 13(3): 93. CrossRef - Glucocorticoids: Fuelling the Fire of Atherosclerosis or Therapeutic Extinguishers?
Clare MacLeod, Patrick W. F. Hadoke, Mark Nixon
International Journal of Molecular Sciences.2021; 22(14): 7622. CrossRef - Cardiovascular and metabolic risk factors in patients with subclinical Cushing
Luigi Petramala, Federica Olmati, Antonio Concistrè, Riccardo Russo, Martina Mezzadri, Maurizio Soldini, Giuseppe De Vincentis, Gino Iannucci, Giorgio De Toma, Claudio Letizia
Endocrine.2020; 70(1): 150. CrossRef - Should Cushing's Syndrome be Considered as a Disease with High Cardiovascular Risk in Relevant Guidelines?
Goran Koracevic, Milan Stojkovic, Dragan Lovic, Milan Pavlovic, Tomislav Kostic, Marija Kutlesic, Sladjana Micic, Maja Koracevic, Milan Djordjevic
Current Vascular Pharmacology.2019; 18(1): 12. CrossRef - Markers of atherosclerosis in patients with Cushing’s syndrome: a meta-analysis of literature studies
Roberta Lupoli, Pasquale Ambrosino, Anna Tortora, Livia Barba, Gelsy Arianna Lupoli, Matteo Nicola Dario Di Minno
Annals of Medicine.2017; 49(3): 206. CrossRef
- Micro- and Macrovascular Effects of Inflammation in Peripheral Artery Disease—Pathophysiology and Translational Therapeutic Approaches

- Adrenal gland
- Limited Diagnostic Utility of Plasma Adrenocorticotropic Hormone for Differentiation between Adrenal Cushing Syndrome and Cushing Disease
- A Ram Hong, Jung Hee Kim, Eun Shil Hong, I Kyeong Kim, Kyeong Seon Park, Chang Ho Ahn, Sang Wan Kim, Chan Soo Shin, Seong Yeon Kim
- Endocrinol Metab. 2015;30(3):297-304. Published online August 4, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.3.297
- 4,804 View
- 68 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Measurement of the plasma adrenocorticotropic hormone (ACTH) level has been recommended as the first diagnostic test for differentiating between ACTH-independent Cushing syndrome (CS) and ACTH-dependent CS. When plasma ACTH values are inconclusive, a differential diagnosis of CS can be made based upon measurement of the serum dehydroepiandrosterone sulfate (DHEA-S) level and results of the high-dose dexamethasone suppression test (HDST). The aim of this study was to assess the utility of plasma ACTH to differentiate adrenal CS from Cushing' disease (CD) and compare it with that of the HDST results and serum DHEA-S level.
Methods We performed a retrospective, multicenter study from January 2000 to May 2012 involving 92 patients with endogenous CS. The levels of plasma ACTH, serum cortisol, 24-hour urine free cortisol (UFC) after the HDST, and serum DHEA-S were measured.
Results Fifty-seven patients had adrenal CS and 35 patients had CD. The area under the curve of plasma ACTH, serum DHEA-S, percentage suppression of serum cortisol, and UFC after HDST were 0.954, 0.841, 0.950, and 0.997, respectively (all
P <0.001). The cut-off values for plasma ACTH, percentage suppression of serum cortisol, and UFC after HDST were 5.3 pmol/L, 33.3%, and 61.6%, respectively. The sensitivity and specificity of plasma ACTH measurement were 84.2% and 94.3%, those of serum cortisol were 95.8% and 90.6%, and those of UFC after the HDST were 97.9% and 96.7%, respectively.Conclusion Significant overlap in plasma ACTH levels was seen between patients with adrenal CS and those with CD. The HDST may be useful in differentiating between these forms of the disease, especially when the plasma ACTH level alone is not conclusive.
-
Citations
Citations to this article as recorded by- Development of diagnostic algorithm for Cushing’s syndrome: a tertiary centre experience
A. Efthymiadis, H. Loo, B. Shine, T. James, B. Keevil, J. W. Tomlinson, A. Pal, R. Pofi
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Eurasian clinical guidelines for the diagnosis and treatment of secondary (symptomatic) forms of arterial hypertension (2022)
I. E. Chazova, N. M. Chikhladze, N. V. Blinova, Zh. E. Belaya, N. M. Danilov, E. M. Elfimova, A. Yu. Litvin, L. Ya. Rozhinskaya, N. Yu. Sviridenko, M. Yu. Shvetsov, V. A. Azizov, E. A. Grigorenko, N. P. Mit’kovskaja, I. I. Mustafaev, A. G. Polupanov, A. S
Eurasian heart journal.2023; (1): 6. CrossRef - Diagnosis and Management of Pituitary Adenomas
Nicholas A. Tritos, Karen K. Miller
JAMA.2023; 329(16): 1386. CrossRef - Distinct serum steroid profiles between adrenal Cushing syndrome and Cushing disease
Chang Gao, Li Ding, Xiaona Zhang, Menghua Yuan, Shaofang Tang, Wei Li, Yuanyuan Ye, Ming Liu, Qing He
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Importance of DHEA-S Levels in Cushing’s Syndrome; Is
There a Cut-off Value in the Differential Diagnosis?
Sema Ciftci, Ozlem Soyluk, Alev Selek, Selvinaz Erol, Zeliha Hekimsoy, Ayse Esen, Huseyin Dursun, Serdar Sahin, Gonca Oruk, Meral Mert, Huseyin Soylu, Banu Sarer Yurekli, Melek Eda Ertorer, Tulay Omma, Mehtap Evran, Mine Adas, Seher Tanrikulu, Kadriye Ayd
Hormone and Metabolic Research.2022; 54(04): 232. CrossRef - Epidemiology and Comorbidity of Adrenal Cushing Syndrome: A Nationwide Cohort Study
Chang Ho Ahn, Jung Hee Kim, Man Young Park, Sang Wan Kim
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): e1362. CrossRef - Metabolic changes in serum steroids for diagnosing and subtyping Cushing’s syndrome
Chang Ho Ahn, Chaelin Lee, Jaeyoon Shim, Sung Hye Kong, Su-jin Kim, Yong Hwy Kim, Kyu Eun Lee, Chan Soo Shin, Jung Hee Kim, Man Ho Choi
The Journal of Steroid Biochemistry and Molecular Biology.2021; 210: 105856. CrossRef - Clinical and Molecular Characteristics of PRKACA L206R Mutant Cortisol-Producing Adenomas in Korean Patients
Insoon Jang, Su-jin Kim, Ra-Young Song, Kwangsoo Kim, Seongmin Choi, Jang-Seok Lee, Min-Kyeong Gwon, Moon Woo Seong, Kyu Eun Lee, Jung Hee Kim
Endocrinology and Metabolism.2021; 36(6): 1287. CrossRef - Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas
Daham Kim, Cheol Ryong Ku, Se Hee Park, Ju Hyung Moon, Eui Hyun Kim, Sun Ho Kim, Eun Jig Lee
World Neurosurgery.2018; 115: e464. CrossRef - Cushing's syndrome: a practical approach to diagnosis and differential diagnoses
Joseph M Pappachan, Christian Hariman, Mahamood Edavalath, Julian Waldron, Fahmy W Hanna
Journal of Clinical Pathology.2017; 70(4): 350. CrossRef
- Development of diagnostic algorithm for Cushing’s syndrome: a tertiary centre experience

- Thyroid
- Medullary Thyroid Carcinoma with Ectopic Adrenocorticotropic Hormone Syndrome
- Hong Seok Choi, Min Joo Kim, Chae Ho Moon, Jong Ho Yoon, Ha Ra Ku, Geon Wook Kang, Im Il Na, Seung-Sook Lee, Byung-Chul Lee, Young Joo Park, Hong Il Kim, Yun Hyi Ku
- Endocrinol Metab. 2014;29(1):96-100. Published online March 14, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.1.96
- 3,698 View
- 40 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Ectopic adrenocorticotropic hormone (ACTH) syndrome is caused most frequently by a bronchial carcinoid tumor or by small cell lung cancer. Medullary thyroid carcinoma (MTC) is a rare etiology of ectopic ACTH syndrome. We describe a case of Cushing syndrome due to ectopic ACTH production from MTC in a 48-year-old male. He was diagnosed with MTC 14 years ago and underwent total thyroidectomy, cervical lymph node dissection and a series of metastasectomies. MTC was confirmed by the pathological examination of the thyroid and metastatic mediastinal lymph node tissues. Two years after his last surgery, he developed Cushingoid features, such as moon face and central obesity, accompanied by uncontrolled hypertension and new-onset diabetes. The laboratory results were compatible with ectopic ACTH syndrome. A bilateral adrenalectomy improved the clinical and laboratory findings that were associated with Cushing syndrome. This is the first confirmed case of ectopic ACTH syndrome caused by MTC in Korea.
-
Citations
Citations to this article as recorded by- Medullary Thyroid Cancer with Ectopic Cushing's Syndrome: A Case Report and Systematic Review of Detailed Cases from the Literature
Andrea Corsello, Vittoria Ramunno, Pietro Locantore, Giovanni Pacini, Esther Diana Rossi, Francesco Torino, Alfredo Pontecorvi, Carmela De Crea, Rosa Maria Paragliola, Marco Raffaelli, Salvatore Maria Corsello
Thyroid.2022; 32(11): 1281. CrossRef - Mucosal Neuroma Cues for Endocrine Emergency Treatment
Gyu Gang Choi, Hwan Jin Lee, Hyo Jin Han, Young Beom Jeong, Heung Bum Lee, Ji Hyun Park
Endocrinology and Metabolism.2021; 36(6): 1312. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Rapid response of hypercortisolism to vandetanib treatment in a patient with advanced medullary thyroid cancer and ectopic Cushing syndrome
Fabián Pitoia, Fernanda Bueno, Angélica Schmidt, Sabrina Lucas, Graciela Cross
Archives of Endocrinology and Metabolism.2015; 59(4): 343. CrossRef
- Medullary Thyroid Cancer with Ectopic Cushing's Syndrome: A Case Report and Systematic Review of Detailed Cases from the Literature

- Adrenal gland
- Adrenocorticotropic Hormone-Independent Cushing Syndrome with Bilateral Cortisol-Secreting Adenomas
- Eu Jeong Ku, A Ram Hong, Ye An Kim, Jae Hyun Bae, Mee Soo Chang, Sang Wan Kim
- Endocrinol Metab. 2013;28(2):133-137. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.133
- 3,951 View
- 44 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader A 48-year-old woman was incidentally found to have bilateral adrenal masses, 2.8 cm in diameter on the right, and 2.3 cm and 1.7 cm in diameter on the left, by abdominal computed tomography. The patient had a medical history of hypertension, which was not being controlled by carvedilol, at a dose of 25 mg daily. She presented with signs and symptoms that suggested Cushing Syndrome. We diagnosed adrenocorticotropic hormone (ACTH)-independent Cushing Syndrome based on the results of basal and dynamic hormone tests. Adrenal vein sampling (AVS) was performed to localize a functioning adrenal cortical mass. AVS results were consistent with hypersecretion of cortisol from both adrenal glands, with a cortisol lateralization ratio of 1.1. Upon bilateral laparoscopic adrenalectomy, bilateral ACTH-independent adrenal adenomas were found. The patient's signs and symptoms of Cushing Syndrome improved after surgery just as the blood pressure was normalized. After surgery, the patient was started on glucocorticoid and mineralocorticoid replacement therapy.
-
Citations
Citations to this article as recorded by- Recent Advances in the Clinical Application of Adrenal Vein Sampling
Shan Zhong, Tianyue Zhang, Minzhi He, Hanxiao Yu, Zhenjie Liu, Zhongyi Li, Xiaoxiao Song, Xiaohong Xu
Frontiers in Endocrinology.2022;[Epub] CrossRef - The role of adrenal venous sampling (AVS) in primary bilateral macronodular adrenocortical hyperplasia (PBMAH): a study of 16 patients
German Rubinstein, Andrea Osswald, Leah Theresa Braun, Frederick Vogel, Matthias Kroiss, Stefan Pilz, Sinan Deniz, Laura Aigner, Thomas Knösel, Jérôme Bertherat, Lucas Bouys, Roland Ladurner, Anna Riester, Martin Bidlingmaier, Felix Beuschlein, Martin Rei
Endocrine.2022; 76(2): 434. CrossRef - Concomitant coexistence of ACTH‐dependent and independent Cushing syndrome
Ach Taieb, Saad Ghada, Gorchène Asma, Ben Abdelkrim Asma, Kacem Maha, Ach Koussay
Clinical Case Reports.2022;[Epub] CrossRef - The Value of Adrenal Androgens for Correcting Cortisol Lateralization in Adrenal Venous Sampling in Patients with Normal Cortisol Secretion
Wenjing Zhang, Keying Zhu, Hongyun Li, Yan Zhang, Dalong Zhu, Xuebin Zhang, Ping Li
International Journal of Endocrinology.2019; 2019: 1. CrossRef - Adrenal venous sampling in patients with ACTH-independent hypercortisolism
Eleni Papakokkinou, Hugo Jakobsson, Augustinas Sakinis, Andreas Muth, Bo Wängberg, Olof Ehn, Gudmundur Johannsson, Oskar Ragnarsson
Endocrine.2019; 66(2): 338. CrossRef - ACTH-independent Cushing’s syndrome with bilateral cortisol-secreting adrenal adenomas: a case report and review of literatures
Jia Wei, Sheyu Li, Qilin Liu, Yuchun Zhu, Nianwei Wu, Ying Tang, Qianrui Li, Kaiyun Ren, Qianying Zhang, Yerong Yu, Zhenmei An, Jing Chen, Jianwei Li
BMC Endocrine Disorders.2018;[Epub] CrossRef - A case of adrenal Cushing’s syndrome with bilateral adrenal masses
Ya-Wun Guo, Chii-Min Hwu, Justin Ging-Shing Won, Chia-Huei Chu, Liang-Yu Lin
Endocrinology, Diabetes & Metabolism Case Reports.2016;[Epub] CrossRef - Bilateral Adrenocortical Masses Producing Aldosterone and Cortisol Independently
Seung-Eun Lee, Jae Hyeon Kim, You-Bin Lee, Hyeri Seok, In Seub Shin, Yeong Hee Eun, Jung-Han Kim, Young Lyun Oh
Endocrinology and Metabolism.2015; 30(4): 607. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - A Case of Bilateral ACTH-independent Adrenal Adenomas with Cushing's Syndrome Treated by Ipsilateral Total and Contralateral Partial Laparoscopic Adrenalectomy
Seung Ah Park, Dong min Jung, Soon young Kim, Nan Young Choi, Tae-jun Kim, Yong kyun Kim, Seong kyun Na, Chul Sik Kim, Seong Jin Lee, Sung-Hee Ihm, Jun Goo Kang
The Korean Journal of Obesity.2013; 22(4): 254. CrossRef
- Recent Advances in the Clinical Application of Adrenal Vein Sampling


 KES
KES

 First
First Prev
Prev



