Search
- Page Path
- HOME > Search
- Hypothalamus and pituitary gland
- Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
- Jung Heo, Yeon-Lim Suh, Se Hoon Kim, Doo-Sik Kong, Do-Hyun Nam, Won-Jae Lee, Sung Tae Kim, Sang Duk Hong, Sujin Ryu, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Kyu Yeon Hur
- Endocrinol Metab. 2024;39(2):387-396. Published online February 5, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1877
- 855 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
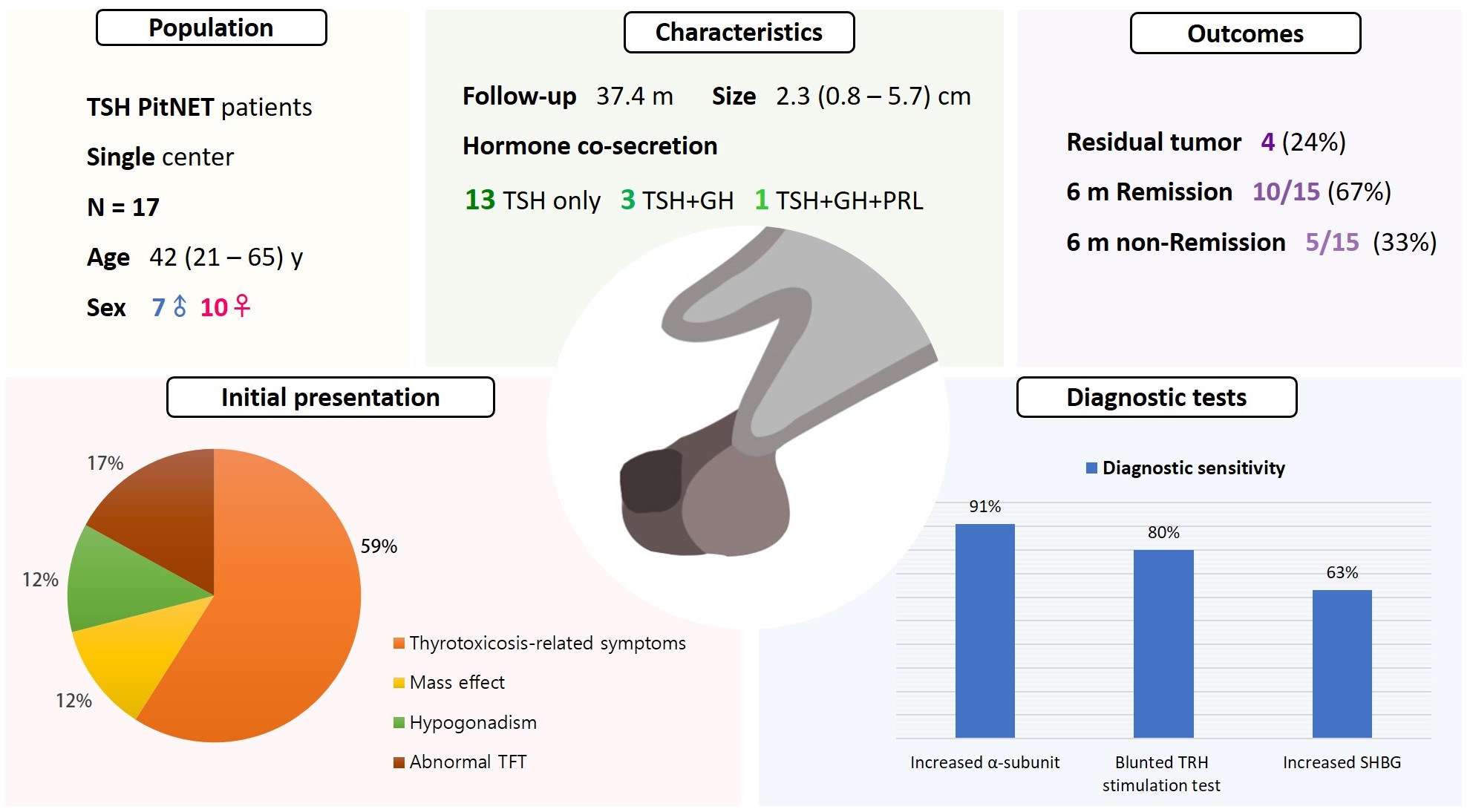
Thyroid-stimulating hormone (TSH)-secreting pituitary neuroendocrine tumor (TSH PitNET) is a rare subtype of PitNET. We investigated the comprehensive characteristics and outcomes of TSH PitNET cases from a single medical center. Also, we compared diagnostic methods to determine which showed superior sensitivity.
Methods
A total of 17 patients diagnosed with TSH PitNET after surgery between 2002 and 2022 in Samsung Medical Center was retrospectively reviewed. Data on comprehensive characteristics and treatment outcomes were collected. The sensitivities of diagnostic methods were compared.
Results
Seven were male (41%), and the median age at diagnosis was 42 years (range, 21 to 65); the median follow-up duration was 37.4 months. The most common (59%) initial presentation was hyperthyroidism-related symptoms. Hormonal co-secretion was present in four (23%) patients. Elevated serum alpha-subunit (α-SU) showed the greatest diagnostic sensitivity (91%), followed by blunted response at thyrotropin-releasing hormone (TRH) stimulation (80%) and elevated sex hormone binding globulin (63%). Fourteen (82%) patients had macroadenoma, and a specimen of one patient with heavy calcification was negative for TSH. Among 15 patients who were followed up for more than 6 months, 10 (67%) achieved hormonal and structural remission within 6 months postoperatively. A case of growth hormone (GH)/TSH/prolactin (PRL) co-secreting mixed gangliocytoma-pituitary adenoma (MGPA) was discovered.
Conclusion
The majority of the TSH PitNET cases was macroadenoma, and 23% showed hormone co-secretion. A rare case of GH/TSH/PRL co-secreting MGPA was discovered. Serum α-SU and TRH stimulation tests showed great diagnostic sensitivity. Careful consideration is needed in diagnosing TSH PitNET. Achieving remission requires complete tumor resection. In case of nonremission, radiotherapy or medical therapy can improve the long-term remission rate.

- Thyroid
- Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
- Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
- Endocrinol Metab. 2023;38(4):381-391. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1778
- 3,046 View
- 462 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
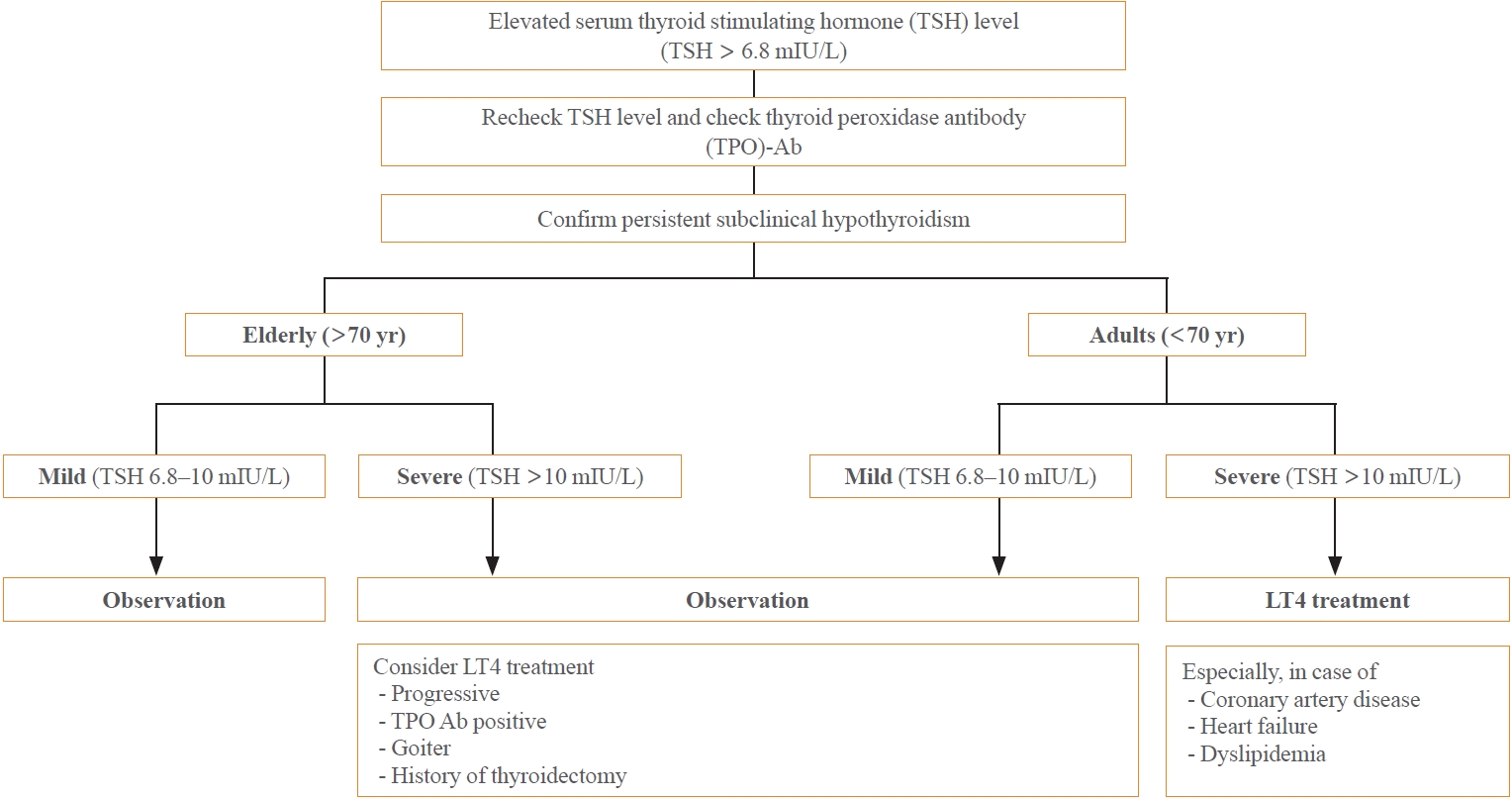
ePub - Subclinical hypothyroidism (SCH) is characterized by elevated thyroid-stimulating hormone (TSH) and normal free thyroxine levels. The Korean Thyroid Association recently issued a guideline for managing SCH, which emphasizes Korean-specific TSH diagnostic criteria and highlights the health benefits of levothyroxine (LT4) treatment. A serum TSH level of 6.8 mIU/L is presented as the reference value for diagnosing SCH. SCH can be classified as mild (TSH 6.8 to 10.0 mIU/L) or severe (TSH >10.0 mIU/L), and patients can be categorized as adults (age <70 years) or elderly (age ≥70 years), depending on the health effects of LT4 treatment. An initial increase in serum TSH levels should be reassessed with a subsequent measurement, including a thyroid peroxidase antibody test, preferably 2 to 3 months after the initial assessment. While LT4 treatment is not generally recommended for mild SCH in adults, it is necessary for severe SCH in patients with underlying coronary artery disease or heart failure and it may be considered for those with concurrent dyslipidemia. Conversely, LT4 treatment is generally not recommended for elderly patients, regardless of SCH severity. For those SCH patients who are prescribed LT4 treatment, the dosage should be personalized, and serum TSH levels should be regularly monitored to maintain the optimal LT4 regimen.
-
Citations
Citations to this article as recorded by- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism
Won Sang Yoo
Endocrinology and Metabolism.2024; 39(1): 188. CrossRef
- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism

- Thyroid
- Thyroid Hormone Reference Intervals among Healthy Individuals In Lanzhou, China
- Yan Lu, Wen-Xia Zhang, De-Hong Li, Lian-Hua Wei, Yu-Jun Zhang, Fu-Na Shi, Shen Zhou
- Endocrinol Metab. 2023;38(3):347-356. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1638
- 2,010 View
- 120 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
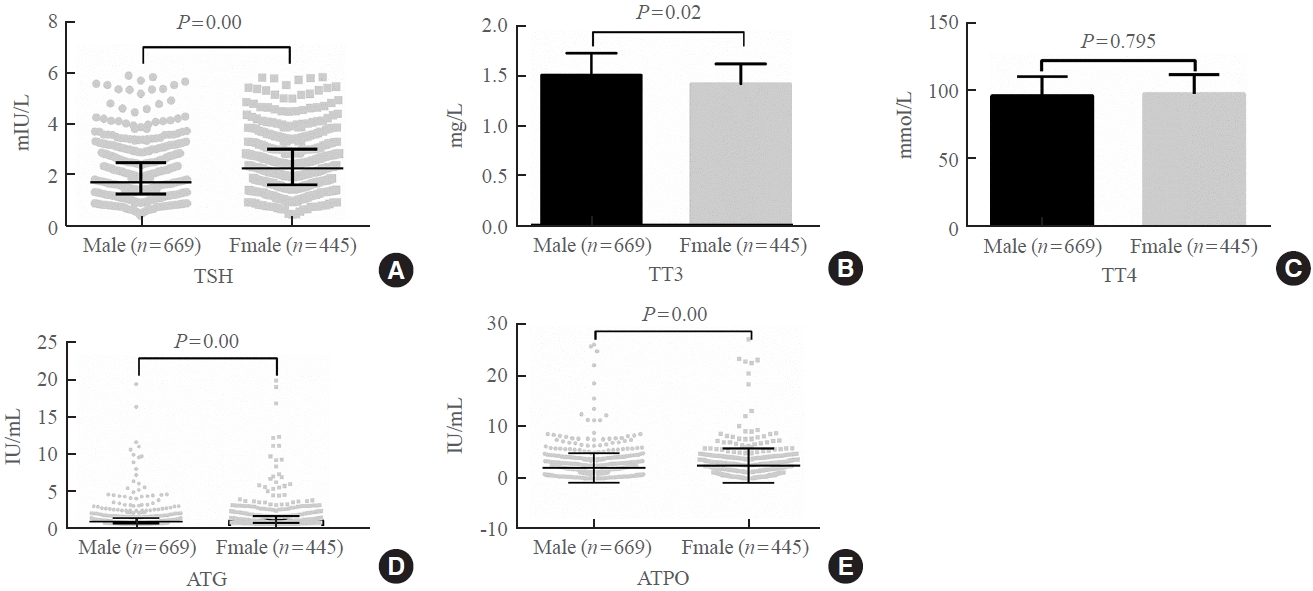
The common reference intervals (RIs) for thyroid hormones currently used in China are provided by equipment manufacturers. This study aimed to establish thyroid hormone RIs in the population of Lanzhou, a city in the subplateau region of northwest China, and compare them with previous reports and manufacturer-provided values.
Methods
In total, 3,123 individuals (1,680 men, 1,443 women) from Lanzhou, an iodine-adequate area of China, perceived as healthy were selected. The Abbott Architect analyzer was used to determine the serum concentration of thyroid hormones. The 95% RI was estimated using the 2.5th and 97.5th percentiles as the lower and upper reference limits, respectively.
Results
The serum levels of thyroid-stimulating hormone (TSH), total triiodothyronine (TT3), antithyroglobulin (ATG) antibody, and antithyroid peroxidase (ATPO) antibody levels were significantly correlated with sex (P<0.05). TSH, total thyroxine (TT4), and ATPO levels were significantly correlated with age (P<0.05). The serum levels of TSH, ATG, and ATPO in men were significantly lower than in women; in contrast, the serum TT3 level was significantly higher in men than in women (P<0.05). Serum TSH, TT3, TT4, and ATG levels differed across age groups (P<0.05), but no such variation was observed for ATG levels (P>0.05). The established RIs of TSH, ATG, and ATPO in this study differed between sexes (P<0.05). The thyroid hormone RIs established herein were inconsistent with the manufacturer-provided values.
Conclusion
The RIs of thyroid hormones in the healthy population of Lanzhou were inconsistent with those in the manufacturer’s manual. Validated sex-specific values are required for diagnosing thyroid diseases. -
Citations
Citations to this article as recorded by- Burden of non-alcoholic fatty liver disease in subclinical hypothyroidism
Mahmood Dhahir Al-Mendalawi
Journal of Clinical and Scientific Research.2024; 13(1): 68. CrossRef
- Burden of non-alcoholic fatty liver disease in subclinical hypothyroidism

- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
- Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
- Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1664
- 1,748 View
- 102 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
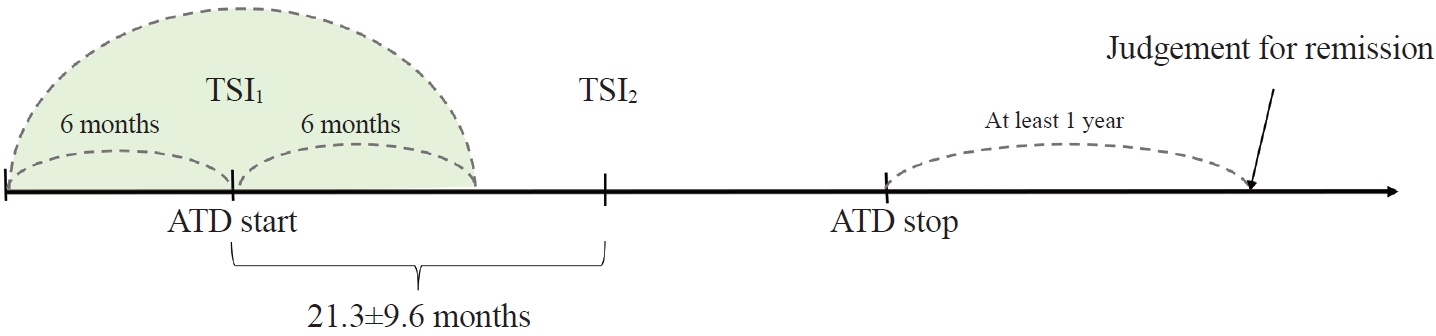
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII,P =0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis. -
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

- Thyroid
- Efficacy and Safety of Long-Term Methimazole versus Radioactive Iodine in the Treatment of Toxic Multinodular Goiter
- Fereidoun Azizi, Navid Saadat, Mir Alireza Takyar, Hengameh Abdi, Ladan Mehran, Atieh Amouzegar
- Endocrinol Metab. 2022;37(6):861-869. Published online November 23, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1476

- 3,935 View
- 375 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study compared the degree of sustained control of hyperthyroidism in patients with toxic multinodular goiter (TMNG) treated with long-term methimazole (LT-MMI) or radioactive iodine (RAI).
Methods
In this clinical trial, 130 untreated patients with TMNG were randomized to either LT-MMI or RAI treatment. Both groups were followed for 108 to 148 months, with median follow-up durations of 120 and 132 months in the LT-MMI and RAI groups, respectively. Both groups of patients were followed every 1 to 3 months in the first year and every 6 months thereafter.
Results
After excluding patients in whom the treatment modality was changed and those who were lost to follow-up, 53 patients in the LT-MMI group and 54 in the RAI group completed the study. At the end of the study period, 50 (96%) and 25 (46%) patients were euthyroid, and two (4%) and 25 (46%) were hypothyroid in LT-MMI and RAI groups, respectively. In the RAI group, four (8%) patients had subclinical hyperthyroidism. The mean time to euthyroidism was 4.3±1.3 months in LT-MMI patients and 16.3± 15.0 months in RAI recipients (P<0.001). Patients treated with LT-MMI spent 95.8%±5.9% of the 12-year study period in a euthyroid state, whereas this proportion was 72.4%±14.8% in the RAI-treated patients (P<0.001). No major treatment-related adverse events were observed in either group.
Conclusion
In patients with TMNG, LT-MMI therapy is superior to RAI treatment, as shown by the earlier achievement of euthyroidism and the longer duration of sustained normal serum thyrotropin. -
Citations
Citations to this article as recorded by- Mechanism of Huatan Sanjie Fang in improving goiter in Graves' disease mice based on the Hippo signaling pathway
Huimin Yuan, Wenxin Ma, Yifei Song, Hang Wang, Shuxin Yan, Silan Hao, Xiaoyun Zhu, Yang Tang
Journal of Traditional Chinese Medical Sciences.2023; 10(3): 289. CrossRef
- Mechanism of Huatan Sanjie Fang in improving goiter in Graves' disease mice based on the Hippo signaling pathway

- Hypothalamus and Pituitary Gland
- Independent Skeletal Actions of Pituitary Hormones
- Se-Min Kim, Farhath Sultana, Funda Korkmaz, Daria Lizneva, Tony Yuen, Mone Zaidi
- Endocrinol Metab. 2022;37(5):719-731. Published online September 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1573
- 3,669 View
- 235 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
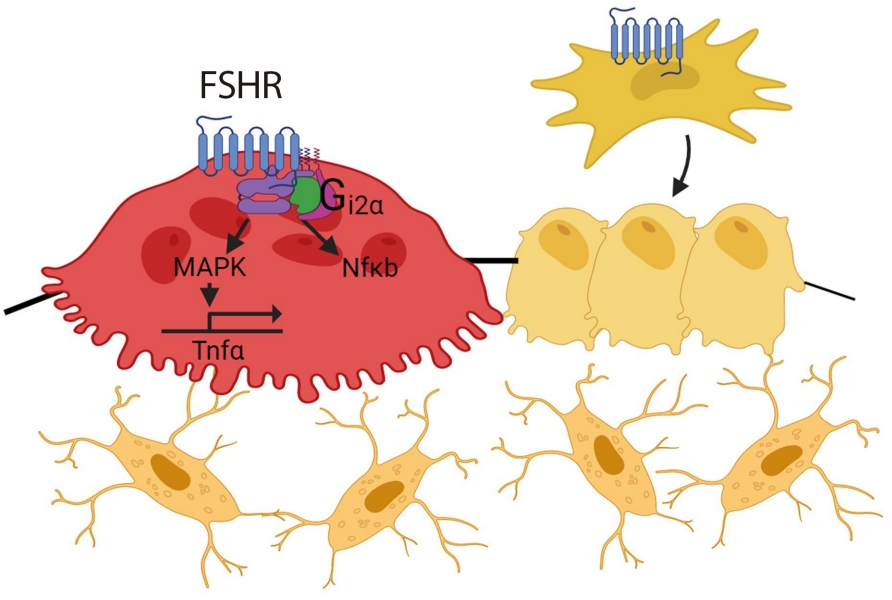
ePub - Over the past years, pituitary hormones and their receptors have been shown to have non-traditional actions that allow them to bypass the hypothalamus-pituitary-effector glands axis. Bone cells—osteoblasts and osteoclasts—express receptors for growth hormone, follicle stimulating hormone (FSH), thyroid stimulating hormone (TSH), adrenocorticotrophic hormone (ACTH), prolactin, oxytocin, and vasopressin. Independent skeletal actions of pituitary hormones on bone have been studied using genetically modified mice with haploinsufficiency and by activating or inactivating the receptors pharmacologically, without altering systemic effector hormone levels. On another front, the discovery of a TSH variant (TSH-βv) in immune cells in the bone marrow and skeletal action of FSHβ through tumor necrosis factor α provides new insights underscoring the integrated physiology of bone-immune-endocrine axis. Here we discuss the interaction of each pituitary hormone with bone and the potential it holds in understanding bone physiology and as a therapeutic target.
-
Citations
Citations to this article as recorded by- New tools for bone health assessment in secreting pituitary adenomas
Meliha Melin Uygur, Stefano Frara, Luigi di Filippo, Andrea Giustina
Trends in Endocrinology & Metabolism.2023; 34(4): 231. CrossRef - A Causality between Thyroid Function and Bone Mineral Density in Childhood: Abnormal Thyrotropin May Be Another Pediatric Predictor of Bone Fragility
Dongjin Lee, Moon Ahn
Metabolites.2023; 13(3): 372. CrossRef - The mechanism of oxytocin and its receptors in regulating cells in bone metabolism
Liu Feixiang, Feng Yanchen, Li Xiang, Zhang Yunke, Miao Jinxin, Wang Jianru, Lin Zixuan
Frontiers in Pharmacology.2023;[Epub] CrossRef - To investigate the mechanism of Yiwei Decoction in the treatment of premature ovarian insufficiency-related osteoporosis using transcriptomics, network pharmacology and molecular docking techniques
Weisen Fan, Yan Meng, Jing Zhang, Muzhen Li, Yingjie Zhang, Xintian Qu, Xin Xiu
Scientific Reports.2023;[Epub] CrossRef
- New tools for bone health assessment in secreting pituitary adenomas

- Thyroid
- Thyroid Function across the Lifespan: Do Age-Related Changes Matter?
- John P. Walsh
- Endocrinol Metab. 2022;37(2):208-219. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1463
- 6,015 View
- 338 Download
- 12 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
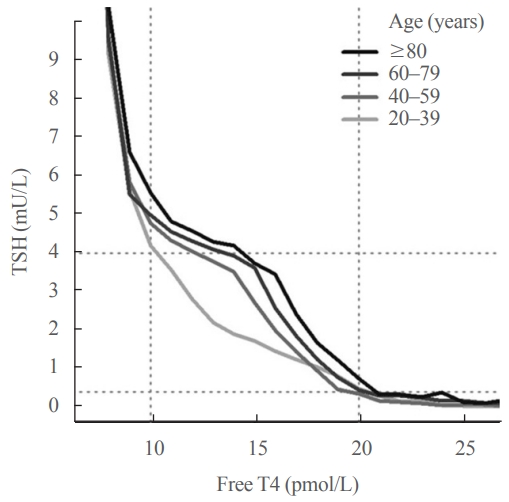
ePub - Circulating concentrations of thyrotropin (TSH) and thyroxine (T4) are tightly regulated. Each individual has setpoints for TSH and free T4 which are genetically determined, and subject to environmental and epigenetic influence. Pituitary-thyroid axis setpoints are probably established in utero, with maturation of thyroid function continuing until late gestation. From neonatal life (characterized by a surge of TSH and T4 secretion) through childhood and adolescence (when free triiodothyronine levels are higher than in adults), thyroid function tests display complex, dynamic patterns which are sexually dimorphic. In later life, TSH increases with age in healthy older adults without an accompanying fall in free T4, indicating alteration in TSH setpoint. In view of this, and evidence that mild subclinical hypothyroidism in older people has no health impact, a strong case can be made for implementation of age-related TSH reference ranges in adults, as is routine in children.
-
Citations
Citations to this article as recorded by- The ageing thyroid: implications for longevity and patient care
Diana van Heemst
Nature Reviews Endocrinology.2024; 20(1): 5. CrossRef - Incidence and Determinants of Spontaneous Normalization of Subclinical Hypothyroidism in Older Adults
Evie van der Spoel, Nicolien A van Vliet, Rosalinde K E Poortvliet, Robert S Du Puy, Wendy P J den Elzen, Terence J Quinn, David J Stott, Naveed Sattar, Patricia M Kearney, Manuel R Blum, Heba Alwan, Nicolas Rodondi, Tinh-Hai Collet, Rudi G J Westendorp,
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1167. CrossRef - Multi-trait analysis characterizes the genetics of thyroid function and identifies causal associations with clinical implications
Rosalie B. T. M. Sterenborg, Inga Steinbrenner, Yong Li, Melissa N. Bujnis, Tatsuhiko Naito, Eirini Marouli, Tessel E. Galesloot, Oladapo Babajide, Laura Andreasen, Arne Astrup, Bjørn Olav Åsvold, Stefania Bandinelli, Marian Beekman, John P. Beilby, Jette
Nature Communications.2024;[Epub] CrossRef - Evaluation of multiple organophosphate insecticide exposure in relation to altered thyroid hormones in NHANES 2007‐2008 adult population
Massira Ousseni Diawara, Songtao Li, Mingzhi Zhang, Francis Manyori Bigambo, Xu Yang, Xu Wang, Tianyu Dong, Di Wu, Chenghao Yan, Yankai Xia
Ecotoxicology and Environmental Safety.2024; 273: 116139. CrossRef - Thyroid-function reference ranges in the diagnosis of thyroid dysfunction in adults
Salman Razvi
Nature Reviews Endocrinology.2024; 20(5): 253. CrossRef - Association between exposure to chemical mixtures and epigenetic ageing biomarkers: Modifying effects of thyroid hormones and physical activity
Wanying Shi, Jianlong Fang, Huimin Ren, Peijie Sun, Juan Liu, Fuchang Deng, Shuyi Zhang, Qiong Wang, Jiaonan Wang, Shilu Tong, Song Tang, Xiaoming Shi
Journal of Hazardous Materials.2024; 469: 134009. CrossRef - DNA Methylation in Autoimmune Thyroid Disease
Nicole Lafontaine, Scott G Wilson, John P Walsh
The Journal of Clinical Endocrinology & Metabolism.2023; 108(3): 604. CrossRef - A Causality between Thyroid Function and Bone Mineral Density in Childhood: Abnormal Thyrotropin May Be Another Pediatric Predictor of Bone Fragility
Dongjin Lee, Moon Ahn
Metabolites.2023; 13(3): 372. CrossRef - Serum Lipidomic Analysis Reveals Biomarkers and Metabolic Pathways of Thyroid Dysfunction
Hua Dong, Wenjie Zhou, Xingxu Yan, Huan Zhao, Honggang Zhao, Yan Jiao, Guijiang Sun, Yubo Li, Zuncheng Zhang
ACS Omega.2023; 8(11): 10355. CrossRef - Developmental and environmental modulation of fecal thyroid hormone levels in wild Assamese macaques (Macaca assamensis)
Verena Behringer, Michael Heistermann, Suchinda Malaivijitnond, Oliver Schülke, Julia Ostner
American Journal of Primatology.2023;[Epub] CrossRef - Prevalence of Functional Alterations and the Effects of Thyroid
Autoimmunity on the Levels of TSH in an Urban Population of Colombia:
A Population-Based Study
Hernando Vargas-Uricoechea, Valentina Agredo-Delgado, Hernando David Vargas-Sierra, María V. Pinzón-Fernández
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(6): 857. CrossRef - Genetic determinants of thyroid function in children
Tessa A Mulder, Purdey J Campbell, Peter N Taylor, Robin P Peeters, Scott G Wilson, Marco Medici, Colin Dayan, Vincent V W Jaddoe, John P Walsh, Nicholas G Martin, Henning Tiemeier, Tim I M Korevaar
European Journal of Endocrinology.2023; 189(2): 164. CrossRef - Relationship between Thyroid CT Density, Volume, and Future TSH Elevation: A 5-Year Follow-Up Study
Tomohiro Kikuchi, Shouhei Hanaoka, Takahiro Nakao, Yukihiro Nomura, Takeharu Yoshikawa, Md Ashraful Alam, Harushi Mori, Naoto Hayashi
Life.2023; 13(12): 2303. CrossRef - Thyroid Stimulating Hormone and Thyroid Hormones (Triiodothyronine and Thyroxine): An American Thyroid Association-Commissioned Review of Current Clinical and Laboratory Status
Katleen Van Uytfanghe, Joel Ehrenkranz, David Halsall, Kelly Hoff, Tze Ping Loh, Carole A. Spencer, Josef Köhrle
Thyroid®.2023; 33(9): 1013. CrossRef - Blood hormones and suicidal behaviour: A systematic review and meta-analysis
Xue-Lei Fu, Xia Li, Jia-Mei Ji, Hua Wu, Hong-Lin Chen
Neuroscience & Biobehavioral Reviews.2022; 139: 104725. CrossRef
- The ageing thyroid: implications for longevity and patient care

- Thyroid
- Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
- Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
- Endocrinol Metab. 2022;37(2):323-332. Published online April 13, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1413
- 3,690 View
- 144 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
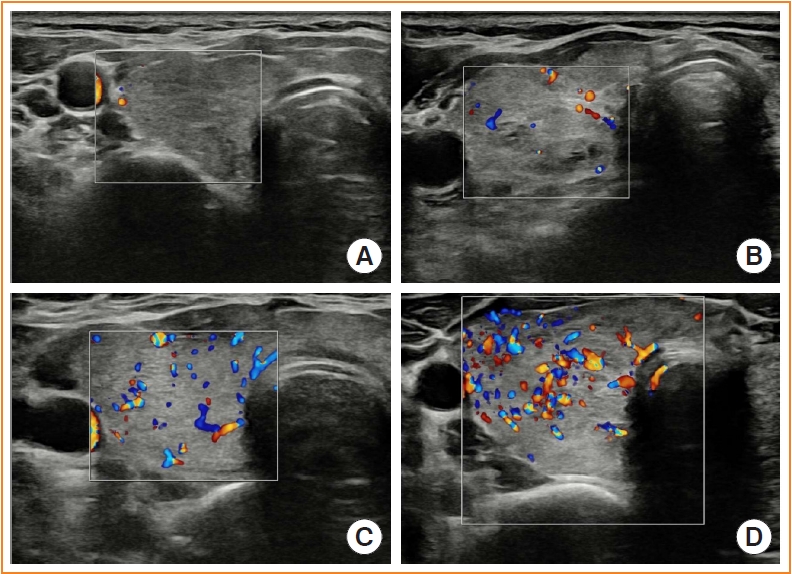
Microvascular ultrasonography (MVUS) is a third-generation Doppler technique that was developed to increase sensitivity compared to conventional Doppler. The purpose of this study was to compare MVUS with conventional color Doppler (CD) and power Doppler (PD) imaging to distinguish Graves’ disease (GD) from destructive thyroiditis (DT).
Methods
This prospective study included 101 subjects (46 GDs, 47 DTs, and eight normal controls) from October 2020 to November 2021. All ultrasonography examinations were performed using microvascular flow technology (MV-Flow). The CD, PD, and MVUS images were semi-quantitatively graded according to blood flow patterns. On the MVUS images, vascularity indices (VIs), which were the ratio (%) of color pixels in the total grayscale pixels in a defined region of interest, were obtained automatically. Receiver operating characteristic curve analysis was performed to verify the diagnostic performance of MVUS. The interclass correlation coefficient and Cohen’s kappa analysis were used to analyze the reliability of MVUS (ClinicalTrials.gov:NCT04879173).
Results
The area under the curve (AUC) for CD, PD, MVUS, and MVUS-VI was 0.822, 0.844, 0.808, and 0.852 respectively. The optimal cutoff value of the MVUS-VI was 24.95% for distinguishing GD and DT with 87% sensitivity and 80.9% specificity. We found a significant positive correlation of MVUS-VI with thyrotropin receptor antibody (r=0.554) and with thyroid stimulating immunoglobulin bioassay (r=0.841). MVUS showed high intra- and inter-observer reliability from various statistical method.
Conclusion
In a real time and quantitative manner, MVUS-VI could be helpful to differentiate GD from thyroiditis in thyrotoxic patients, with less inter-observer variability. -
Citations
Citations to this article as recorded by- Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management
Jin Wang, Ke Wan, Xin Chang, Rui-Feng Mao
World Journal of Diabetes.2024; 15(3): 348. CrossRef - The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Duplex Hemodynamic Parameters of Both Superior and Inferior Thyroid Arteries in Evaluation of Thyroid Hyperfunction Disorders
Maha Assem Hussein, Alaa Abdel Hamid, Rasha M Abdel Samie, Elshaymaa Hussein, Shereen Sadik Elsawy
International Journal of General Medicine.2022; Volume 15: 7131. CrossRef - Case 5: A 41-Year-Old Woman With Palpitation
Jiwon Yang, Kabsoo Shin, Jeongmin Lee, Jeonghoon Ha, Dong-Jun Lim, Han-Sang Baek
Journal of Korean Medical Science.2022;[Epub] CrossRef - Microvascular assessment of fascio-cutaneous flaps by ultrasound: A large animal study
Guillaume Goudot, Yanis Berkane, Eloi de Clermont-Tonnerre, Claire Guinier, Irina Filz von Reiterdank, Antonia van Kampen, Korkut Uygun, Curtis L. Cetrulo, Basak E. Uygun, Anahita Dua, Alexandre G. Lellouch
Frontiers in Physiology.2022;[Epub] CrossRef
- Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management

- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,302 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
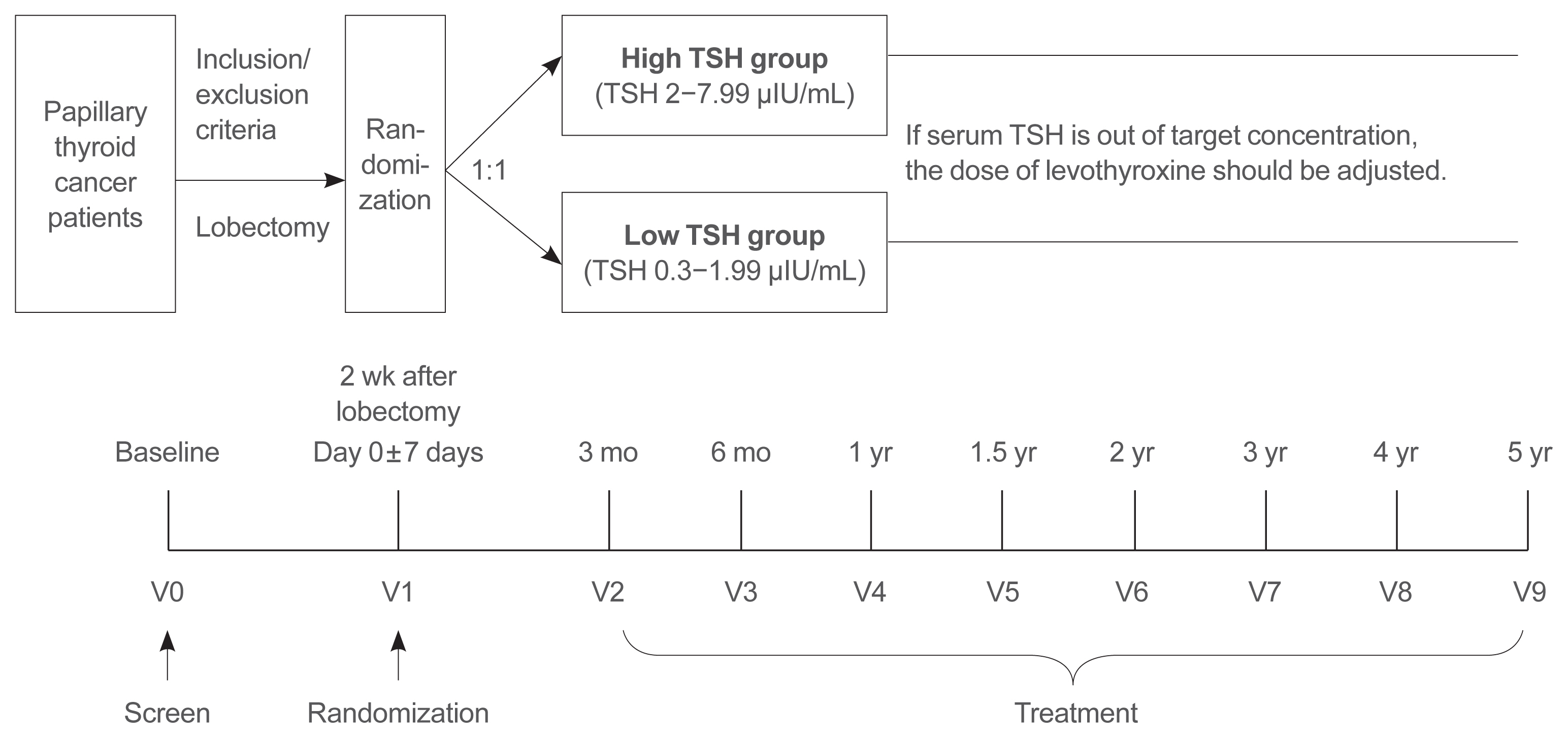
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Endocrine Research
- DEHP Down-Regulates Tshr Gene Expression in Rat Thyroid Tissues and FRTL-5 Rat Thyrocytes: A Potential Mechanism of Thyroid Disruption
- Min Joo Kim, Hwan Hee Kim, Young Shin Song, Ok-Hee Kim, Kyungho Choi, Sujin Kim, Byung-Chul Oh, Young Joo Park
- Endocrinol Metab. 2021;36(2):447-454. Published online March 31, 2021
- DOI: https://doi.org/10.3803/EnM.2020.920
- 5,064 View
- 145 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
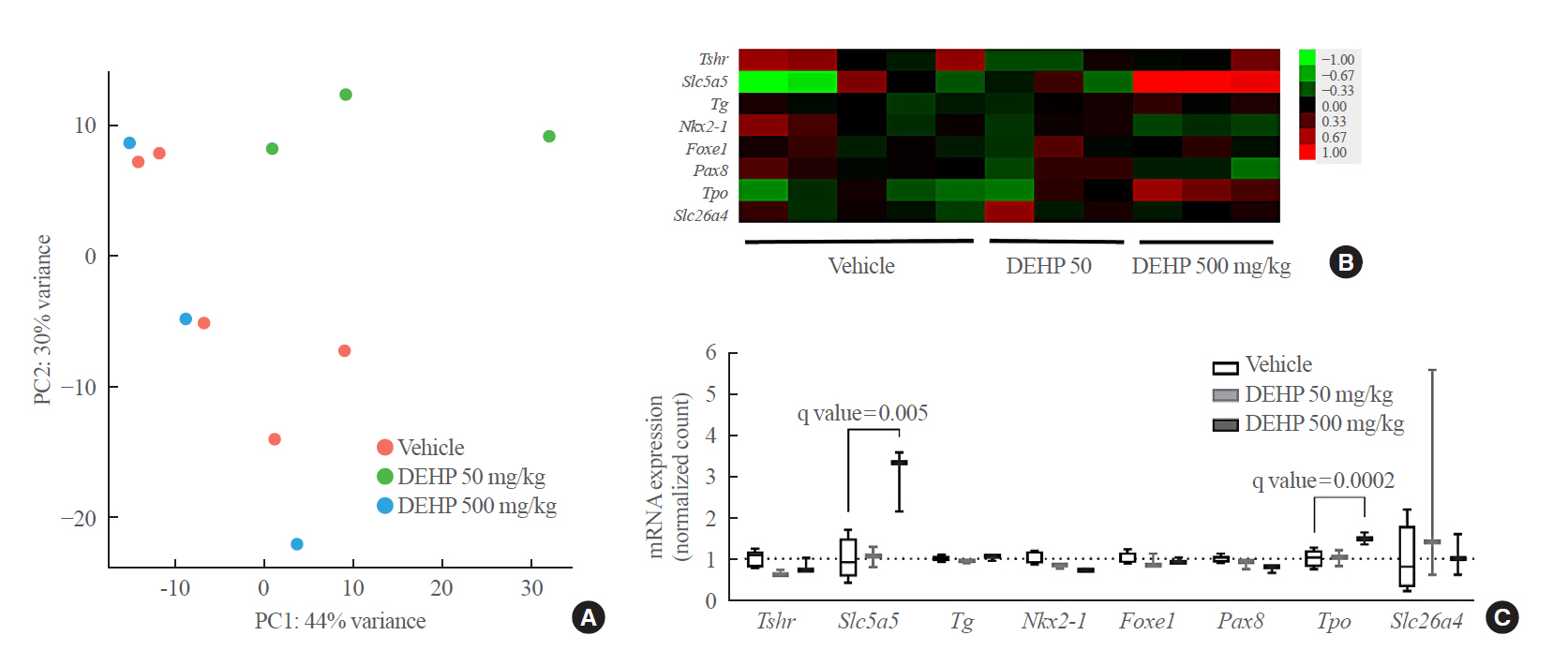
ePub - Background
Di-2-ethylhexyl phthalate (DEHP) is known to disrupt thyroid hormonal status. However, the underlying molecular mechanism of this disruption is unclear. Therefore, we investigated the direct effects of DEHP on the thyroid gland.
Methods
DEHP (vehicle, 50 mg/kg, and 500 mg/kg) was administered to Sprague-Dawley rats for 2 weeks. The expression of the thyroid hormone synthesis pathway in rat thyroid tissues was analyzed through RNA sequencing analysis, quantitative reverse transcription-polymerase chain reaction (RT-PCR), and immunohistochemical (IHC) staining. DEHP was treated to FRTL-5 rat thyroid cells, and an RT-PCR analysis was performed. A reporter gene assay containing the promoter of thyroid stimulating hormone receptor (TSHR) in Nthy-ori 3-1 human thyroid cells was constructed, and luciferase activity was determined.
Results
After DEHP treatment, the free thyroxine (T4) and total T4 levels in rats significantly decreased. RNA sequencing analysis of rat thyroid tissues showed little difference between vehicle and DEHP groups. In the RT-PCR analysis, Tshr expression was significantly lower in both DEHP groups (50 and 500 mg/kg) compared to that in the vehicle group, and IHC staining showed that TSHR expression in the 50 mg/kg DEHP group significantly decreased. DEHP treatment to FRTL-5 cells significantly down-regulated Tshr expression. DEHP treatment also reduced luciferase activity in a reporter gene assay for TSHR.
Conclusion
Although overall genetic changes in the thyroid hormone synthesis pathway are not clear, DEHP exposure could significantly down-regulate Tshr expression in thyroid glands. Down-regulation of Tshr gene appears to be one of potential mechanisms of thyroid disruption by DEHP exposure. -
Citations
Citations to this article as recorded by- ARTS is essential for di-2-ethylhexyl phthalate (DEHP)-induced apoptosis of mouse Leydig cells
Yue Li, Linlin Xu, Chaoju Hao, Si Yang, Jinglei Wang, Jiaxiang Chen
Ecotoxicology and Environmental Safety.2024; 270: 115882. CrossRef - Thyroid dysfunction caused by exposure to environmental endocrine disruptors and the underlying mechanism: A review
Jie He, Jie Xu, Mucong Zheng, Kai Pan, Lilin Yang, Lina Ma, Chuyang Wang, Jie Yu
Chemico-Biological Interactions.2024; 391: 110909. CrossRef - Intrauterine exposure to di(2-ethylhexyl) phthalate (DEHP) disrupts the function of the hypothalamus-pituitary-thyroid axis of the F1 rats during adult life
Érica Kássia Sousa-Vidal, Guilherme Henrique, Renata Elen Costa da Silva, Caroline Serrano-Nascimento
Frontiers in Endocrinology.2023;[Epub] CrossRef - Drinking water disinfection byproduct iodoacetic acid affects thyroid hormone synthesis in Nthy-ori 3–1 cells
Jingyi Xiao, Yujie Sha, Yuwen Huang, Kunling Long, Huan Wu, Yan Mo, Qiyuan Yang, Shengkun Dong, Qiang Zeng, Xiao Wei
Ecotoxicology and Environmental Safety.2023; 257: 114926. CrossRef - Assessment of five typical environmental endocrine disruptors and thyroid cancer risk: a meta-analysis
Yuyao Yang, Xiaoyue Bai, Juan Lu, Ronghao Zou, Rui Ding, Xiaohui Hua
Frontiers in Endocrinology.2023;[Epub] CrossRef - Investigation of the effects of phthalates on in vitro thyroid models with RNA-Seq and ATAC-Seq
Marta Nazzari, Mírian Romitti, Duncan Hauser, Daniel J. Carvalho, Stefan Giselbrecht, Lorenzo Moroni, Sabine Costagliola, Florian Caiment
Frontiers in Endocrinology.2023;[Epub] CrossRef - Di(2-ethylhexyl) phthalate (DEHP) and thyroid: biological mechanisms of interference and possible clinical implications
Xueting Zhang, Wen Qi, Qi Xu, Xu Li, Liting Zhou, Lin Ye
Environmental Science and Pollution Research.2022; 29(2): 1634. CrossRef - The possible thyroid disruptive effect of di-(2-ethyl hexyl) phthalate and the potential protective role of selenium and curcumin nanoparticles: a toxicological and histological study
Naima Abd El-Halim Sherif, Asmaa El-Banna, Rehab Ahmed Abdel-Moneim, Zahraa Khalifa Sobh, Manal Ibrahim Fathy Balah
Toxicology Research.2022; 11(1): 108. CrossRef - Environmental disruption of reproductive rhythms
Marie-Azélie Moralia, Clarisse Quignon, Marine Simonneaux, Valérie Simonneaux
Frontiers in Neuroendocrinology.2022; 66: 100990. CrossRef - Endocrine-disruptor endpoints in the ovary and thyroid of adult female rats exposed to realistic doses of di-(2-ethylhexyl) phthalate
Amel Jebara, Asma Beltifa, Guissepa Di Bella, Lotfi Mabrouk, Hedi Ben Mansour
Journal of Water and Health.2022; 20(8): 1256. CrossRef - The influence of sunitinib and sorafenib, two tyrosine kinase inhibitors, on development and thyroid system in zebrafish larvae
Gang Wei, Cao-xu Zhang, Yu Jing, Xia Chen, Huai-dong Song, Liu Yang
Chemosphere.2022; 308: 136354. CrossRef - Role of estrogen receptors in thyroid toxicity induced by mono (2-ethylhexyl) phthalate via endoplasmic reticulum stress: An in vitro mechanistic investigation
Qi Xu, Liting Zhou, Hyonju Ri, Xu Li, Xueting Zhang, Wen Qi, Lin Ye
Environmental Toxicology and Pharmacology.2022; 96: 104007. CrossRef
- ARTS is essential for di-2-ethylhexyl phthalate (DEHP)-induced apoptosis of mouse Leydig cells

- Clinical Study
- Subclinical Hypothyroidism Affects the Long-Term Outcomes of Patients Who Undergo Coronary Artery Bypass Grafting Surgery but Not Heart Valve Surgery
- Hana Kim, Sung Hye Kong, Jae Hoon Moon, Sang Yoon Kim, Kay-Hyun Park, Jun Sung Kim, Joong Haeng Choh, Young Joo Park, Cheong Lim
- Endocrinol Metab. 2020;35(2):308-318. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.308
- 6,521 View
- 152 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
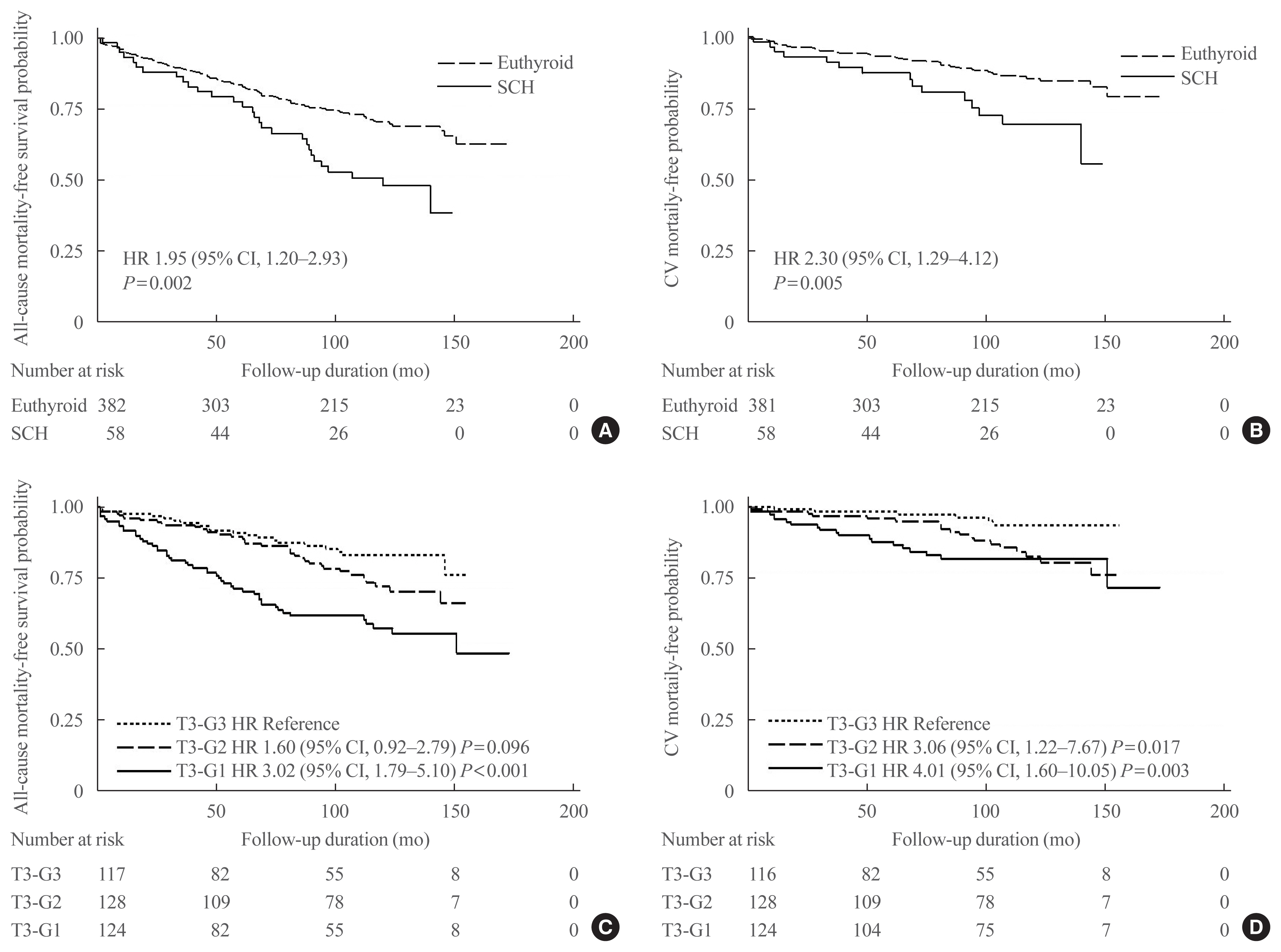
ePub - Background
The aim of this study was to determine the associations between subclinical hypothyroidism (SCH) and long-term cardiovascular outcomes after coronary artery bypass grafting (CABG) or heart valve surgery (HVS).
Methods
We retrospectively reviewed and compared all-cause mortality, cardiovascular mortality, and cardiovascular events in 461 patients who underwent CABG and 104 patients who underwent HVS.
Results
During a mean±standard deviation follow-up duration of 7.6±3.8 years, there were 187 all-cause deaths, 97 cardiovascular deaths, 127 major adverse cardiovascular events (MACE), 11 myocardial infarctions, one unstable angina, 70 strokes, 30 hospitalizations due to heart failure, 101 atrial fibrillation, and 33 coronary revascularizations. The incidence of all-cause mortality after CABG was significantly higher in patients with SCH (n=36, 55.4%) than in euthyroid patients (n=120, 30.3%), with a hazard ratio of 1.70 (95% confidence interval, 1.10 to 2.63; P=0.018) after adjustment for age, sex, current smoking status, body mass index, underlying diseases, left ventricular dysfunction, and emergency operation. Interestingly, low total triiodothyronine (T3) levels in euthyroid patients who underwent CABG were significantly associated with increased risks of all-cause mortality, cardiovascular mortality, and MACE, but those associations were not observed in HVS patients. Both free thyroxine and thyroid-stimulating hormone levels in euthyroid patients were not related with any cardiovascular outcomes in either the CABG or HVS group.
Conclusion
SCH or low total T3 might be associated with a poor prognosis after CABG, but not after HVS, implying that preoperative thyroid hormonal status may be important in ischemic heart disease patients. -
Citations
Citations to this article as recorded by- Subclinical hypothyroidism and clinical outcomes after cardiac surgery: A systematic review and meta-analysis
Michele Dell’Aquila, Camilla S. Rossi, Tulio Caldonazo, Gianmarco Cancelli, Lamia Harik, Giovanni J. Soletti, Kevin R. An, Jordan Leith, Hristo Kirov, Mudathir Ibrahim, Michelle Demetres, Arnaldo Dimagli, Mohamed Rahouma, Mario Gaudino
JTCVS Open.2024; 18: 64. CrossRef - The Association Between Hypothyroidism Treatment and Mortality in Patients Hospitalized in Surgical Wards
Hiba Masri-Iraqi, Yaron Rudman, Carmel Friedrich Dubinchik, Idit Dotan, Talia Diker-Cohen, Liat Sasson, Tzipora Shochat, Ilan Shimon, Eyal Robenshtok, Amit Akirov
Endocrine Research.2023; 48(2-3): 68. CrossRef - Mid-term outcomes of patients with subclinical hypothyroidism after coronary bypass surgery
Dong Zhao, Wei Zhao, Chuangshi Wang, Fei Xu, Wei Zhao, Xieraili Tiemuerniyazi, Hao Ma, Wei Feng
Interdisciplinary CardioVascular and Thoracic Surgery.2023;[Epub] CrossRef - Thyroid Pathology in High-Risk Cardiac Surgery Patients with Coronary Artery Disease
Olena K. Gogayeva, Anatoliy V. Rudenko, Vasyl V. Lazoryshynets, Serhii A. Rudenko, Tetiana A. Andrushchenko
Ukrainian Journal of Cardiovascular Surgery.2022; 30(1 (46)): 9. CrossRef - High-TSH Subclinical Hypothyroidism Is Associated With Postoperative Mortality in Acute Type A Aortic Dissection
Shi-Pan Wang, Yuan Xue, Hai-Yang Li, Wen-Jian Jiang, Hong-Jia Zhang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Triiodothyronine improves contractile recovery of human atrial trabeculae after hypoxia/reoxygenation
Petra Kleinbongard, Philipp Kuthan, Chantal Eickelmann, Philipp Jakobs, Joachim Altschmied, Judith Haendeler, Arjang Ruhparwar, Matthias Thielmann, Gerd Heusch
International Journal of Cardiology.2022; 363: 159. CrossRef - Hypothyroidism Is Correlated with Ventilator Complications and Longer Hospital Days after Coronary Artery Bypass Grafting Surgery in a Relatively Young Population: A Nationwide, Population-Based Study
Jiun-Yu Lin, Pei-Chi Kao, Yi-Ting Tsai, Chi-Hsiang Chung, Wu-Chien Chien, Chih-Yuan Lin, Chieh-Hua Lu, Chien-Sung Tsai
Journal of Clinical Medicine.2022; 11(13): 3881. CrossRef - Minor perturbations of thyroid homeostasis and major cardiovascular endpoints—Physiological mechanisms and clinical evidence
Patrick Müller, Melvin Khee-Shing Leow, Johannes W. Dietrich
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2021; 36(3): 500. CrossRef
- Subclinical hypothyroidism and clinical outcomes after cardiac surgery: A systematic review and meta-analysis

- Thyroid
- Update on Thyroid Hormone Levels and Thyroid Dysfunction in the Korean Population Based on Data from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- Jae Hoon Chung
- Endocrinol Metab. 2020;35(1):7-13. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.7
- 6,963 View
- 150 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
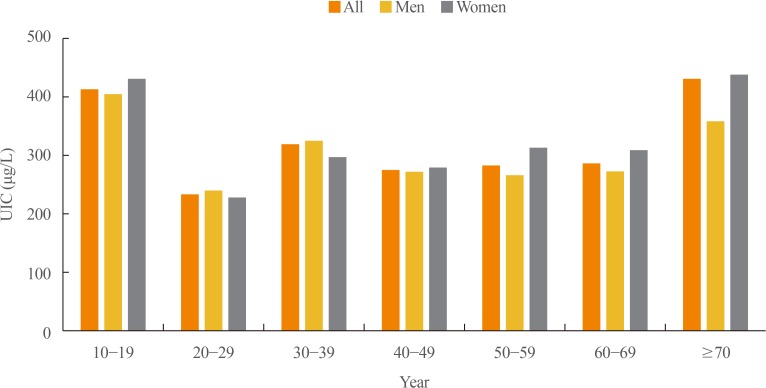
ePub In 2017, the first Korean nationwide data on serum thyroid stimulating hormone (TSH) levels, serum free thyroxine (fT4) levels, and urinary iodine concentration (UIC) were published based on a population of 7,061 Koreans who participated in the Korea National Health and Nutrition Examination Survey VI. The mean TSH level was 2.16 mIU/L, with a reference interval of 0.59 to 7.03 mIU/L (men 2.09 mIU/L, women 2.24 mIU/L,
P <0.001). A U-shaped association was found between serum TSH levels and age. The mean fT4 level was 1.25 ng/dL, and its reference interval was 0.92 to 1.60 ng/dL (men 1.29 ng/dL, women 1.20 ng/dL,P <0.0001). Serum fT4 levels decreased with age (P for trend <0.0001). Serum thyroid peroxidase antibody (TPOAb) was detected in 7.30% of participants (men 4.33%, women 10.62%). TPOAb titers tended to increase with age, and were higher in women than in men. The median UIC was 294 µg/L, and UIC showed a U-shaped relationship with age. According to the World Health Organization recommendations, only 23% of participants were in the adequate range of iodine intake, while 65% were in the above requirements or excessive, and 12% in insufficient. The prevalence of overt hyperthyroidism and hypothyroidism in Koreans was 0.34% to 0.54% and 0.73% to 1.43%, respectively.-
Citations
Citations to this article as recorded by- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey
Eunji Mun, Hye Ah Lee, Jung Eun Choi, Rosie Lee, Kyung Hee Kim, Hyesook Park, Hae Soon Kim
Children.2024; 11(3): 370. CrossRef - Diagnostic Value of Carotid Plaque Assessment with AIS Based on Quantitative Parameters of Dual-Layer Detector Spectral CT
Xiaoying Meng, Fei Li, Wenpei Wu, Juncang Wu
International Journal of General Medicine.2024; Volume 17: 1263. CrossRef - Hyperthyroidism
Sun Y. Lee, Elizabeth N. Pearce
JAMA.2023; 330(15): 1472. CrossRef - Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
Endocrinology and Metabolism.2023; 38(6): 729. CrossRef - Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2021; 36(3): 500. CrossRef - Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 790. CrossRef
- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey

- Clinical Study
- Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study
- Mijin Kim, Bo Hyun Kim, Hyungi Lee, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
- Endocrinol Metab. 2020;35(1):106-114. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.106
- 6,121 View
- 120 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
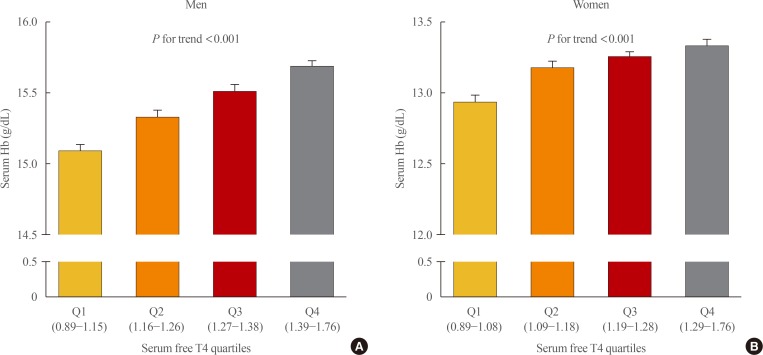
ePub Background Studies on the relationship between thyroid function and anemia in the euthyroid range are scarce. We aimed to evaluate the association between anemia and serum free thyroxine (fT4) and thyrotropin (TSH) in euthyroid adults.
Methods Data on 5,352 participants aged ≥19 years were obtained from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015). Anemia was defined as hemoglobin (Hb) <13 and <12 g/dL for men and women, respectively.
Results Overall, 6.1% of participants had anemia, and more women (9.9%) had anemia than men (2.8%,
P <0.001). In multivariate analysis, serum fT4 levels, but not TSH, were positively associated with serum Hb levels in both sexes (P <0.001, each). Serum Hb levels linearly reduced across decreasing serum fT4 quartile groups in both sexes (P <0.001, each). After adjusting for potential confounding factors, participants with low-normal fT4 had 4.4 (P =0.003) and 2.8 times (P <0.001) higher risk for anemia than those with high-normal fT4 among men and women, respectively. When participants were divided into two groups at 50 years of age, in younger participants, men and women with the first quartile were at higher risk of anemia than men with the second quartile (odds ratio [OR], 3.3;P =0.029) and women with the forth quartile (OR, 3.2;P <0.001), respectively. This association was not observed in older participants.Conclusion These results suggest that a low-normal level of serum fT4 was associated with a lower serum Hb level and a higher risk of anemia in euthyroid adults, especially in younger participants.
-
Citations
Citations to this article as recorded by- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank
Nicolien A van Vliet, Annelies E P Kamphuis, Wendy P J den Elzen, Gerard J Blauw, Jacobijn Gussekloo, Raymond Noordam, Diana van Heemst
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e643. CrossRef - Thyroid function, pernicious anemia and erythropoiesis: a two-sample Mendelian randomization study
Alisa D Kjaergaard, Alexander Teumer, Eirini Marouli, Panos Deloukas, Aleksander Kuś, Rosalie Sterenborg, Bjørn O Åsvold, Marco Medici, Christina Ellervik
Human Molecular Genetics.2022; 31(15): 2548. CrossRef - Changes of hematological indices in patients with diffuse toxic goiter
F. H. Saidova, L. M. Ahmedova, Zh. B. Aslanova, N. A. Najafov
Klinicheskaia khirurgiia.2021; 88(3-4): 76. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Zheng Feei Ma
Endocrinology and Metabolism.2020; 35(2): 484. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2020; 35(3): 669. CrossRef
- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank

- Clinical Characteristics of Graves' Disease Patients with Undetectable Thyrotropin Binding Inhibitor Immunoglubulin (TB2).
- Bo Youn Cho, Won Bae Kim, Hong Gyu Lee, Chang Soon Koh, Seong Yeon Kim, Seok In Lee, Jae Seok Chun, Kyung Soo Park
- J Korean Endocr Soc. 1996;11(1):68-74. Published online November 7, 2019
- 1,610 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Graves disease is an autoimmune disease caused by TSH receptor antibodies. Thyrotropin binding inhibitor immunoglobulins(TBII) are detected in most Graves patients, but some patients have no TBII activities in their sera. It is unknown whether the clinical features of TBII-positive patients are different from those of TBII-negative patients. Methods: To evaluate the prevalence of TBII-negative Graves' patients and its clinical differences from TBII-positive patients, we examined TBII by radioreceptor assay in 686 consecutive untreated Graves patients. We found 84 TBII-negative patients(15 men and 69 women, mean age ±EM: 40.9±.4 years) and compared their clinical characteristics with 87 TBII-positive patients (22 men and 65 women, mean age±EM: 39.9±.5 years) who were selected randomly from the same patients group. Results: In this study, TBII was undetectable in 12.2% of patients with Graves' disease(84 of 686). TBII-negative group had a less weight loss than TBII-positive group. However, there was no significant differences in age, sex ratio, prevalence of ophthalmopathy, duration of illness and positive rate of family history for thyroid diseases between TBII-negative and -positive groups. Serum total T or T levels were not different from each other, but T3-uptake was significantly higher in TBII-positive group than that in TBII-negative group, suggesting that the free hormone levels in TBII-negative group might be lower. The thyroid uptake of 99mTcO4 was significantly higher in TBII positive group than that in TBII-negative group. Thyroid autoantibodies, including antimicrosomal and antithyroglobulin antibodies were detected in almost all patients but there were no differences in titers and positive rate between TBII-negative and -positive groups. Conclusion: Although TBII-negative Graves patients showed less weight loss and low 99mTc04 thyroidal uptake compare to TBII-positive patients, the clinical and immunological characteristics of TBII-negative patients are not different from TBII-positive one.

- Identification of TPA - Response Element (TRE) in the Rat Thyrotropin - Releasing Hormone (TRH) Gene.
- Woon Won Jung, Young Kil Choi, In Myung Yang, Kwang Sik Seo, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim, Young Kil Choi, Seung Joon Park
- J Korean Endocr Soc. 1994;10(3):200-213. Published online November 6, 2019
- 1,216 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - There are two potential imperfect copies of the TRE consensus sequence between -47 and -113bp position on 5' upstream of the rat TRH gene. The upstream element(5'-TGcCgTCA-3') is located between -101 bp and -94 bp, and the downstream element(5'-TGAcCTCA-3') is positioned between -59bp and -52bp relative to the stranscription start site. The downstream variant differs from the consensus sequence of TRE(AP-1)(5'-TGACTCA-3'), by addition of one nucleotide. As there is no direct evidence that TPA stimulates the transcription of rat TRH gene, and there is no study to define TRE of the rat TRH gene, we performed Northern blot assay, transient gene expression study and gel shift assay to identify TRE. TRH mRNA expression of CA77 cells was increased about 2-2.5 fold 30 min after TPA stimulation. When PC12 cells were stimulated by TPA after transfection of the plasmids containing serially deleted 5'upstream of the rat TRH gene ligated to luciferase gene, the transcription of luciferase gene was increased more than 3.2 fold with the plasmid pTRH(-600/84)Luc and pTRH(-113/84)Luc. However, the transcriptional activation was remarkably decreased less than 1.6 fold with pTRH(-77/84)Luc, pTRH(-47/84)Luc, and pTRH(6/84)Luc. The plasmid containing the sequence of -108/-79 did not show any significant activation in both of basal and TPA-stimulated transcription, whereas the plasmid containing the sequence of -70/-41 showed a slight but significant transcriptional activation by TPA. The plasmid containing the sequence of -114/-47 showed remarkable increase in basal transcription and TPA induced transcription of luciferase gene. Gel shift assay revealed that the oligonucleotides spanning -108/-79 and -70/-41 bound to c-Jun, whereas the oligonucleotides spanning -40/1, 1/30, 31/60, 61/84 did not bind. The oligonucleotide of -70/-41 bound to c-Jun with higher affinity compared to that of -108/-79. The one base pair mutant of -70/-41(deletion of C from the middle of TGACCTCA) bound to c-Jun with higher affinity, whereas the one base pair replaced mutant(C to G) bound with lower affinity compared to the wild type oligonucleotide. These results suggest that the rat TRH gene expression is stimulated by TPA to a smaller degree compared to that of other genes, and the two elements act cooperatively as TRE. The downstream TRE variant is mainly responsible for TPA response and c-Jun binding, and the upstream variant play a permissive role for transcriptional activation. The addition of one nucleotide C in the downstream element may be responsible for the relatively lower response of the rat TRH gene to TPA.


 KES
KES

 First
First Prev
Prev



