Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Bone Loss after Solid Organ Transplantation: A Review of Organ-Specific Considerations
- Kyoung Jin Kim, Jeonghoon Ha, Sang Wan Kim, Jung-Eun Kim, Sihoon Lee, Han Seok Choi, Namki Hong, Sung Hye Kong, Seong Hee Ahn, So Young Park, Ki-Hyun Baek, on Behalf of Metabolic Bone Disease Study Group of Korean Endocrine Society
- Endocrinol Metab. 2024;39(2):267-282. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1939

- 748 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - This review article investigates solid organ transplantation-induced osteoporosis, a critical yet often overlooked issue, emphasizing its significance in post-transplant care. The initial sections provide a comprehensive understanding of the prevalence and multifactorial pathogenesis of transplantation osteoporosis, including factors such as deteriorating post-transplantation health, hormonal changes, and the impact of immunosuppressive medications. Furthermore, the review is dedicated to organ-specific considerations in transplantation osteoporosis, with separate analyses for kidney, liver, heart, and lung transplantations. Each section elucidates the unique challenges and management strategies pertinent to transplantation osteoporosis in relation to each organ type, highlighting the necessity of an organ-specific approach to fully understand the diverse manifestations and implications of transplantation osteoporosis. This review underscores the importance of this topic in transplant medicine, aiming to enhance awareness and knowledge among clinicians and researchers. By comprehensively examining transplantation osteoporosis, this study contributes to the development of improved management and care strategies, ultimately leading to improved patient outcomes in this vulnerable group. This detailed review serves as an essential resource for those involved in the complex multidisciplinary care of transplant recipients.

- Calcium & bone metabolism
- Acromegaly and Bone: An Update
- Andrea Giustina
- Endocrinol Metab. 2023;38(6):655-666. Published online December 22, 2023
- DOI: https://doi.org/10.3803/EnM.2023.601
- 1,547 View
- 125 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
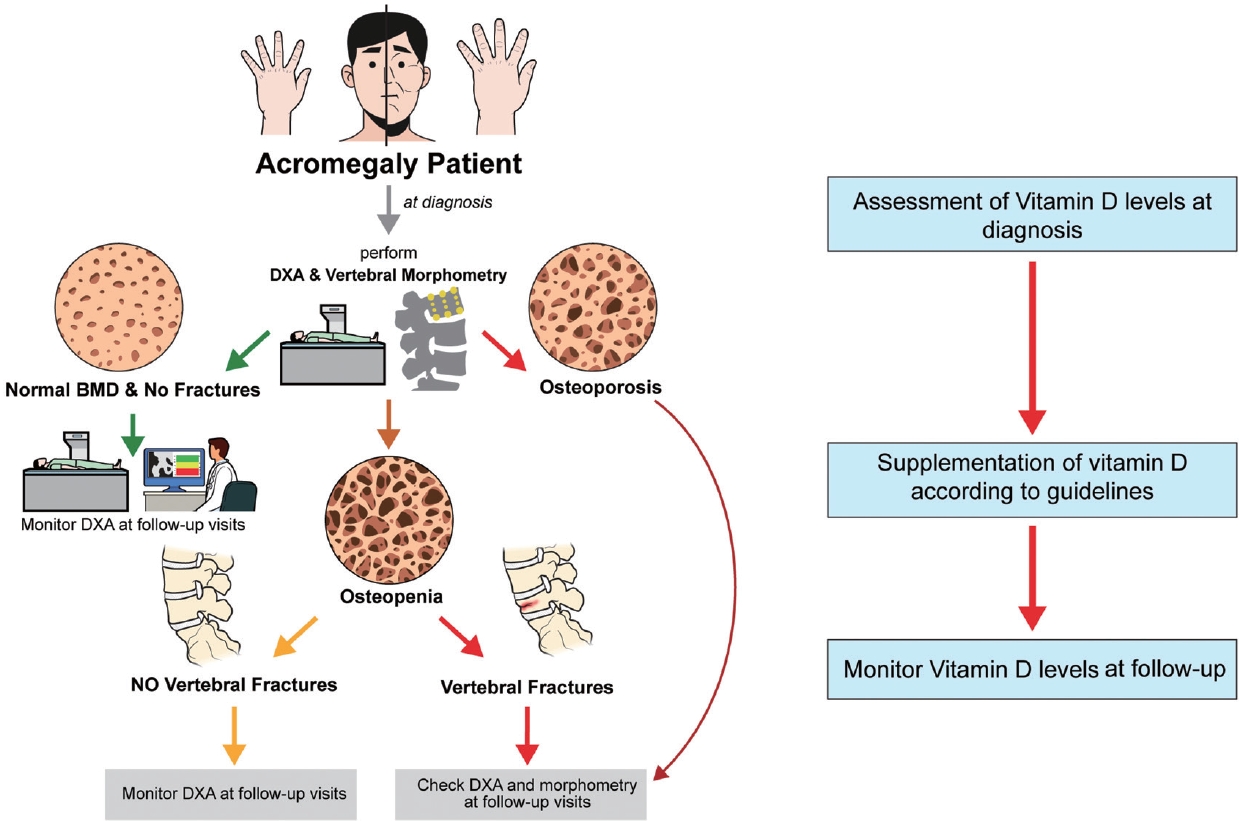
ePub - Since our discovery in 2006 that acromegaly is associated with an increased risk of vertebral fractures, many authors have confirmed this finding in both cross-sectional and prospective studies. Due to the high epidemiological and clinical impact of this newly discovered comorbidity of acromegaly, this topic has progressively become more important and prominent over the years, and the pertinent literature has been enriched by new findings on the pathophysiology and treatment. The aim of this narrative review was to discuss these novel findings, integrating them with the seminal observations, in order to give the reader an updated view of how the field of acromegaly and bone is developing, from strong clinical observations to a mechanistic understanding and possible prevention and treatment.
-
Citations
Citations to this article as recorded by- New insights into the vitamin D/PTH axis in endocrine-driven metabolic bone diseases
Luigi di Filippo, John P. Bilezikian, Ernesto Canalis, Umberto Terenzi, Andrea Giustina
Endocrine.2024;[Epub] CrossRef - Bone health and skeletal fragility in second- and third-line medical therapies for acromegaly: preliminary results from a pilot single center experience
Sabrina Chiloiro, Antonella Giampietro, Amato Infante, Pier Paolo Mattogno, Liverana Lauretti, Alessandro Olivi, Laura De Marinis, Alfredo Pontecorvi, Francesco Doglietto, Antonio Bianchi
Pituitary.2024;[Epub] CrossRef
- New insights into the vitamin D/PTH axis in endocrine-driven metabolic bone diseases

- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2023;38(6):679-689. Published online December 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1760

- 1,300 View
- 66 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Limited longitudinal evidence exists regarding the potential association between smoking status and hip fracture among individuals with type 2 diabetes. We investigated this association using large-scale, nationwide cohort data for the Korean population.
Methods
This nationwide cohort study included 1,414,635 adults aged 40 and older who received Korean National Health Insurance Service health examinations between 2009 and 2012. Subjects with type 2 diabetes were categorized according to their smoking status, amount smoked (pack-years), number of cigarettes smoked per day, and duration of smoking. The results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between smoking status parameters and risk of hip fracture in multivariable Cox proportional hazard regression analysis.
Results
Compared with never-smokers, an increased adjusted HR (aHR) for hip fracture was observed in current smokers (1.681; 95% CI, 1.578 to 1.791), and a comparable aHR for hip fracture was found in former smokers (1.065; 95% CI, 0.999 to 1.136). For former smokers who had smoked 20 pack-years or more, the risk was slightly higher than that for never-smokers (aHR, 1.107; 95% CI, 1.024 to 1.196). The hip fracture risk of female former smokers was similar to that of female current smokers, but the hip fracture risk in male former smokers was similar to that of male never-smokers.
Conclusion
Smoking is associated with an increased risk of hip fracture in patients with type 2 diabetes. Current smokers with diabetes should be encouraged to quit smoking because the risk of hip fracture is greatly reduced in former smokers.

- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
- Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
- Endocrinol Metab. 2023;38(6):690-700. Published online October 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1782

- 1,480 View
- 94 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Acromegaly leads to various skeletal complications, and fragility fractures are emerging as a new concern in patients with acromegaly. Therefore, this study investigated the risk of fractures in Korean patients with acromegaly.
Methods
We used the Korean nationwide claims database from 2009 to 2019. A total of 931 patients with acromegaly who had never used an osteoporosis drug before and were treated with surgery alone were selected as study participants, and a 1:29 ratio of 26,999 age- and sex-matched osteoporosis drug-naïve controls without acromegaly were randomly selected from the database.
Results
The mean age was 46.2 years, and 50.0% were male. During a median follow-up of 54.1 months, there was no difference in the risks of all, vertebral, and non-vertebral fractures between the acromegaly and control groups. However, hip fracture risk was significantly higher (hazard ratio [HR], 2.73; 95% confidence interval [CI], 1.32 to 5.65), and non-hip and non-vertebral fractures risk was significantly lower (HR, 0.40; 95% CI, 0.17 to 0.98) in patients with acromegaly than in controls; these results remained robust even after adjustment for socioeconomic status and baseline comorbidities. Age, type 2 diabetes mellitus, cardio-cerebrovascular disease, fracture history, recent use of acid-suppressant medication, psychotropic medication, and opioids were risk factors for all fractures in patients with acromegaly (all P<0.05).
Conclusion
Compared with controls, patients surgically treated for acromegaly had a higher risk of hip fractures. The risk factors for fracture in patients with acromegaly were consistent with widely accepted risk factors in the general population.

- Calcium & bone metabolism
- Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
- Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
- Endocrinol Metab. 2023;38(6):669-678. Published online September 1, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1734

- 1,598 View
- 90 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Height loss is a simple clinical measure associated with increased fracture risk. However, limited data exists on the association between height loss and fracture risk in postmenopausal Korean women. It is unknown whether this association varies with age.
Methods
Data on height loss over a 6-year period were collected from a community-based longitudinal follow-up cohort (Ansung cohort of the Korean Genome and Epidemiology Study). Incident fractures were defined based on self-reported fractures after excluding those due to severe trauma or toes/fingers. The association between incident fractures and height loss was investigated using a Cox proportional hazards model.
Results
During a median follow-up of 10 years after the second visit, 259/1,806 participants (median age, 64 years) experienced incident fractures. Overall, a 1 standard deviation (SD) decrease in height (1.6 cm/median 5.8 years) was associated with 9% increased risk of fracture (hazard ratio [HR], 1.09; P=0.037), which lost statistical significance after adjustment for covariates. When stratified into age groups (50–59, 60–69, 70 years or older), a 1 SD decrease in height remained a robust predictor of fracture in the 50 to 59 years age group after adjusting for covariates (adjusted hazard ratio [aHR], 1.52; P=0.003), whereas height loss was not an independent predictor of fracture in the 60 to 69 (aHR, 1.06; P=0.333) or the 70 years or older age groups (aHR, 1.05; P=0.700; P for interaction <0.05, for all).
Conclusion
Height loss during the previous 6 years was associated with an increased 10-year fracture risk in postmenopausal women in their 50s.

- Calcium & bone metabolism
- Cardiovascular Impact of Calcium and Vitamin D Supplements: A Narrative Review
- Fatima Zarzour, Ahmad Didi, Mohammed Almohaya, David Kendler
- Endocrinol Metab. 2023;38(1):56-68. Published online February 16, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1644
- 4,159 View
- 284 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
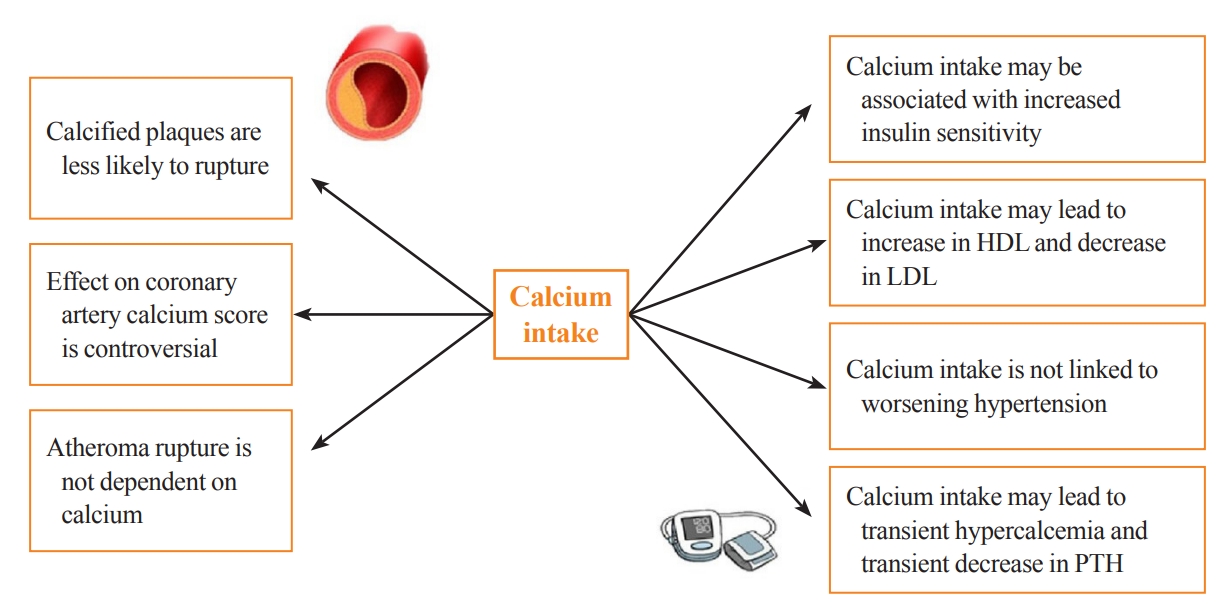
ePub - Calcium and vitamin D play an important role in mineral homeostasis and the maintenance of skeletal health. Calcium and vitamin D supplements have been widely used for fracture prevention in elderly populations. Many trials have studied the effectiveness and cardiovascular safety of calcium and vitamin D supplementation, with disparate results. In this review, we summarize the most important trials and systematic reviews. There is significant heterogeneity in clinical trial design, differences in the nature of trial outcomes (self-reported vs. verified), prior calcium intake, and trial size. Inconsistent results have been reported concerning the effects of calcium and vitamin D supplementation on cardiovascular outcomes. Most current guidelines recommend calcium intake of up to 1,200 mg daily, preferably from the diet, without concern for cardiovascular risk. Recommendations regarding vitamin D supplementation vary widely. There is compelling evidence from well-conducted randomized trials that modest vitamin D supplementation is safe but does not confer cardiovascular benefit or cardiovascular harm.
-
Citations
Citations to this article as recorded by- Evaluating adherence, tolerability and safety of oral calcium citrate in elderly osteopenic subjects: a real-life non-interventional, prospective, multicenter study
Mariangela Rondanelli, Salvatore Minisola, Marco Barale, Daniele Barbaro, Francesca Mansueto, Santina Battaglia, Gloria Bonaccorsi, Santina Caliri, Alessandro Cavioni, Luciano Colangelo, Sabrina Corbetta, Federica Coretti, Giorgia Dito, Valentina Gavioli,
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - Association between Daily Dietary Calcium Intake and the Risk of Cardiovascular Disease (CVD) in Postmenopausal Korean Women
Jae Kyung Lee, Thi Minh Chau Tran, Euna Choi, Jinkyung Baek, Hae-Rim Kim, Heeyon Kim, Bo Hyon Yun, Seok Kyo Seo
Nutrients.2024; 16(7): 1043. CrossRef - Effect of Denosumab on Bone Density in Postmenopausal Osteoporosis: A Comparison with and without Calcium Supplementation in Patients on Standard Diets in Korea
Chaiho Jeong, Jinyoung Kim, Jeongmin Lee, Yejee Lim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha
Journal of Clinical Medicine.2023; 12(21): 6904. CrossRef
- Evaluating adherence, tolerability and safety of oral calcium citrate in elderly osteopenic subjects: a real-life non-interventional, prospective, multicenter study

- Calcium & Bone Metabolism
- Development of a Spine X-Ray-Based Fracture Prediction Model Using a Deep Learning Algorithm
- Sung Hye Kong, Jae-Won Lee, Byeong Uk Bae, Jin Kyeong Sung, Kyu Hwan Jung, Jung Hee Kim, Chan Soo Shin
- Endocrinol Metab. 2022;37(4):674-683. Published online August 5, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1461
- 4,053 View
- 213 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
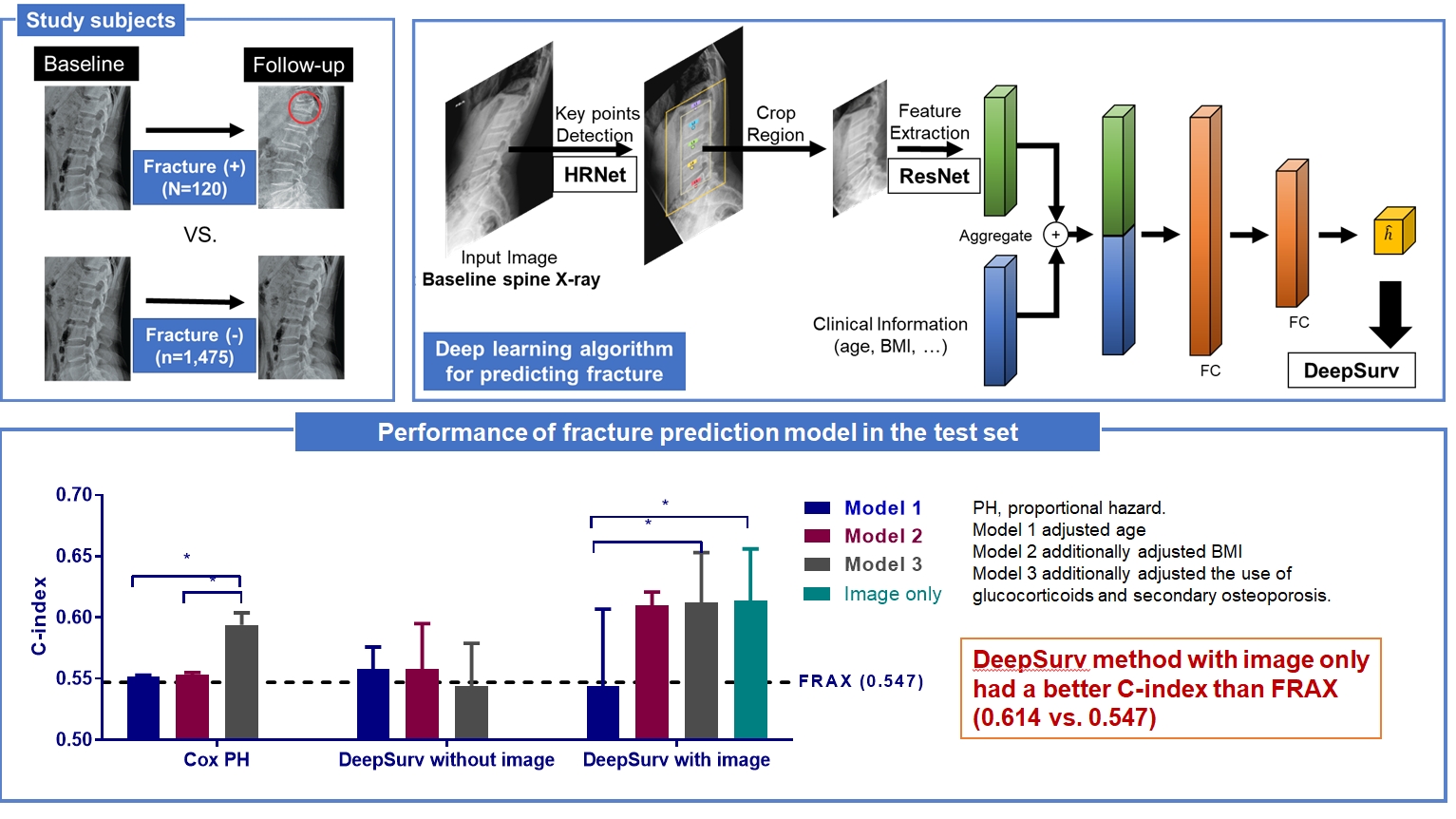
Since image-based fracture prediction models using deep learning are lacking, we aimed to develop an X-ray-based fracture prediction model using deep learning with longitudinal data.
Methods
This study included 1,595 participants aged 50 to 75 years with at least two lumbosacral radiographs without baseline fractures from 2010 to 2015 at Seoul National University Hospital. Positive and negative cases were defined according to whether vertebral fractures developed during follow-up. The cases were divided into training (n=1,416) and test (n=179) sets. A convolutional neural network (CNN)-based prediction algorithm, DeepSurv, was trained with images and baseline clinical information (age, sex, body mass index, glucocorticoid use, and secondary osteoporosis). The concordance index (C-index) was used to compare performance between DeepSurv and the Fracture Risk Assessment Tool (FRAX) and Cox proportional hazard (CoxPH) models.
Results
Of the total participants, 1,188 (74.4%) were women, and the mean age was 60.5 years. During a mean follow-up period of 40.7 months, vertebral fractures occurred in 7.5% (120/1,595) of participants. In the test set, when DeepSurv learned with images and clinical features, it showed higher performance than FRAX and CoxPH in terms of C-index values (DeepSurv, 0.612; 95% confidence interval [CI], 0.571 to 0.653; FRAX, 0.547; CoxPH, 0.594; 95% CI, 0.552 to 0.555). Notably, the DeepSurv method without clinical features had a higher C-index (0.614; 95% CI, 0.572 to 0.656) than that of FRAX in women.
Conclusion
DeepSurv, a CNN-based prediction algorithm using baseline image and clinical information, outperformed the FRAX and CoxPH models in predicting osteoporotic fracture from spine radiographs in a longitudinal cohort. -
Citations
Citations to this article as recorded by- Automated detection of vertebral fractures from X-ray images: A novel machine learning model and survey of the field
Li-Wei Cheng, Hsin-Hung Chou, Yu-Xuan Cai, Kuo-Yuan Huang, Chin-Chiang Hsieh, Po-Lun Chu, I-Szu Cheng, Sun-Yuan Hsieh
Neurocomputing.2024; 566: 126946. CrossRef - Application of radiomics model based on lumbar computed tomography in diagnosis of elderly osteoporosis
Baisen Chen, Jiaming Cui, Chaochen Li, Pengjun Xu, Guanhua Xu, Jiawei Jiang, Pengfei Xue, Yuyu Sun, Zhiming Cui
Journal of Orthopaedic Research.2024; 42(6): 1356. CrossRef - Machine Learning and Deep Learning in Spinal Injury: A Narrative Review of Algorithms in Diagnosis and Prognosis
Satoshi Maki, Takeo Furuya, Masahiro Inoue, Yasuhiro Shiga, Kazuhide Inage, Yawara Eguchi, Sumihisa Orita, Seiji Ohtori
Journal of Clinical Medicine.2024; 13(3): 705. CrossRef - A CT-based Deep Learning Model for Predicting Subsequent Fracture Risk in Patients with Hip Fracture
Yisak Kim, Young-Gon Kim, Jung-Wee Park, Byung Woo Kim, Youmin Shin, Sung Hye Kong, Jung Hee Kim, Young-Kyun Lee, Sang Wan Kim, Chan Soo Shin
Radiology.2024;[Epub] CrossRef - A Novel QCT-Based Deep Transfer Learning Approach for Predicting Stiffness Tensor of Trabecular Bone Cubes
Pengwei Xiao, Tinghe Zhang, Yufei Huang, Xiaodu Wang
IRBM.2024; 45(2): 100831. CrossRef - Deep learning in the radiologic diagnosis of osteoporosis: a literature review
Yu He, Jiaxi Lin, Shiqi Zhu, Jinzhou Zhu, Zhonghua Xu
Journal of International Medical Research.2024;[Epub] CrossRef - Development and Validation of a Convolutional Neural Network Model to Predict a Pathologic Fracture in the Proximal Femur Using Abdomen and Pelvis CT Images of Patients With Advanced Cancer
Min Wook Joo, Taehoon Ko, Min Seob Kim, Yong-Suk Lee, Seung Han Shin, Yang-Guk Chung, Hong Kwon Lee
Clinical Orthopaedics & Related Research.2023; 481(11): 2247. CrossRef - Automated Opportunistic Trabecular Volumetric Bone Mineral Density Extraction Outperforms Manual Measurements for the Prediction of Vertebral Fractures in Routine CT
Sophia S. Goller, Jon F. Rischewski, Thomas Liebig, Jens Ricke, Sebastian Siller, Vanessa F. Schmidt, Robert Stahl, Julian Kulozik, Thomas Baum, Jan S. Kirschke, Sarah C. Foreman, Alexandra S. Gersing
Diagnostics.2023; 13(12): 2119. CrossRef - Machine learning‐based prediction of osteoporosis in postmenopausal women with clinical examined features: A quantitative clinical study
Kainat A. Ullah, Faisal Rehman, Muhammad Anwar, Muhammad Faheem, Naveed Riaz
Health Science Reports.2023;[Epub] CrossRef - Skeletal Fracture Detection with Deep Learning: A Comprehensive Review
Zhihao Su, Afzan Adam, Mohammad Faidzul Nasrudin, Masri Ayob, Gauthamen Punganan
Diagnostics.2023; 13(20): 3245. CrossRef - Deep learning system for automated detection of posterior ligamentous complex injury in patients with thoracolumbar fracture on MRI
Sang Won Jo, Eun Kyung Khil, Kyoung Yeon Lee, Il Choi, Yu Sung Yoon, Jang Gyu Cha, Jae Hyeok Lee, Hyunggi Kim, Sun Yeop Lee
Scientific Reports.2023;[Epub] CrossRef - Vertebra Segmentation Based Vertebral Compression Fracture Determination from Reconstructed Spine X-Ray Images
Srinivasa Rao Gadu, Chandra Sekhar Potala
International Journal of Electrical and Electronics Research.2023; 11(4): 1225. CrossRef - Computer Vision in Osteoporotic Vertebral Fracture Risk Prediction: A Systematic Review
Anthony K. Allam, Adrish Anand, Alex R. Flores, Alexander E. Ropper
Neurospine.2023; 20(4): 1112. CrossRef - A Meaningful Journey to Predict Fractures with Deep Learning
Jeonghoon Ha
Endocrinology and Metabolism.2022; 37(4): 617. CrossRef - New Horizons: Artificial Intelligence Tools for Managing Osteoporosis
Hans Peter Dimai
The Journal of Clinical Endocrinology & Metabolism.2022;[Epub] CrossRef
- Automated detection of vertebral fractures from X-ray images: A novel machine learning model and survey of the field

- Calcium & Bone Metabolism
- Effect of Vitamin D Supplementation on Risk of Fractures and Falls According to Dosage and Interval: A Meta-Analysis
- Sung Hye Kong, Han Na Jang, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
- Endocrinol Metab. 2022;37(2):344-358. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1374

- 6,366 View
- 282 Download
- 16 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although recent studies comparing various dosages and intervals of vitamin D supplementation have been published, it is yet to be elucidated whether there is an appropriate dose or interval to provide benefit regarding fracture risk. We aimed to assess the published evidence available to date regarding the putative beneficial effects of vitamin D supplements on fractures and falls according to various dosages and intervals.
Methods
We performed a meta-analysis of randomized controlled studies reporting associations between vitamin D supplementation and the risks of fractures and falls in PubMed, EMBASE, and Cochrane library. Studies with supplements of ergocalciferol or calcitriol, those with a number of event ≤10, or those with a follow-up duration of less than 6 months were also excluded.
Results
Thirty-two studies were included in the final analysis. Vitamin D supplementation with daily dose of 800 to 1,000 mg was associated with lower risks of osteoporotic fracture and fall (pooled relative risk [RR], 0.87; 95% confidence interval [CI], 0.78 to 0.97 and RR, 0.91; 95% CI, 0.85 to 0.98), while studies with <800 or >1,000 mg/day did not. Also, among intervals, daily administration of vitamin D was associated with the reduced risk of falls, while intermittent dose was not. Also, patients with vitamin D deficiency showed a significant risk reduction of falls after vitamin D supplementation.
Conclusion
Daily vitamin D dose of 800 to 1,000 IU was the most probable way to reduce the fracture and fall risk. Further studies designed with various regimens and targeted vitamin D levels are required to elucidate the benefits of vitamin D supplements. -
Citations
Citations to this article as recorded by- Ukrainian Consensus on Diagnosis and Management of Vitamin D Deficiency in Adults
Nataliia Grygorieva, Mykola Tronko, Volodymir Kovalenko, Serhiy Komisarenko, Tetiana Tatarchuk, Ninel Dedukh, Mykola Veliky, Serhiy Strafun, Yulia Komisarenko, Andrii Kalashnikov, Valeria Orlenko, Volodymyr Pankiv, Oleg Shvets, Inna Gogunska, Svitlana Reg
Nutrients.2024; 16(2): 270. CrossRef - Vitamin D Supplementation: A Review of the Evidence Arguing for a Daily Dose of 2000 International Units (50 µg) of Vitamin D for Adults in the General Population
Pawel Pludowski, William B. Grant, Spyridon N. Karras, Armin Zittermann, Stefan Pilz
Nutrients.2024; 16(3): 391. CrossRef - Clinical Characteristics and Outcomes of Limb Fractures in Saudi Children
Lamia Aldhbiban, Fai Alhoshan, Raghad Alomari, Shahad A Almatrafi, Yousef Alanazi, Samir Alsayegh, Haifa Y Alfaraidi, Ayman H Jawadi, Fahad N Aljuraibah
Cureus.2024;[Epub] CrossRef - The interplay of rheumatoid arthritis and osteoporosis: exploring the pathogenesis and pharmacological approaches
Nikhil Gupta, Navjot Kanwar, Anchal Arora, Kavin Khatri, Abhinav Kanwal
Clinical Rheumatology.2024; 43(5): 1421. CrossRef - The multi-faceted nature of age-associated osteoporosis
A.E. Smit, O.C. Meijer, E.M. Winter
Bone Reports.2024; 20: 101750. CrossRef - Vitamin D Deficiency in Patients With Low-Energy Hip Fractures in Accordance With the Mediterranean Paradox
Christos Konstantinidis, Ourania Psoma, Christos Kotsias, Vasileios Panagiotopoulos , Sotiris Plakoutsis, Dimitrios Tsiampas, Dimitrios Vardakas, Dimitrios Giotis
Cureus.2024;[Epub] CrossRef - Effect of vitamin D, calcium, or combined supplementation on fall prevention: a systematic review and updated network meta-analysis
Long Tan, Ruiqian He, Xiaoxue Zheng
BMC Geriatrics.2024;[Epub] CrossRef - Association of vitamin and/or nutritional supplements with fall among patients with diabetes: A prospective study based on ACCORD and UK Biobank
Lingfang He, Tianqi Ma, Guogang Zhang, Xunjie Cheng, Yongping Bai
Frontiers in Nutrition.2023;[Epub] CrossRef - Vitamin D and Calcium in Osteoporosis, and the Role of Bone Turnover Markers: A Narrative Review of Recent Data from RCTs
Gavriela Voulgaridou, Sousana K. Papadopoulou, Paraskevi Detopoulou, Despoina Tsoumana, Constantinos Giaginis, Foivi S. Kondyli, Evgenia Lymperaki, Agathi Pritsa
Diseases.2023; 11(1): 29. CrossRef - Recent advances in the identification of related factors and preventive strategies of hip fracture
Yaohui Yu, Yudan Wang, Xiaoli Hou, Faming Tian
Frontiers in Public Health.2023;[Epub] CrossRef - Can Nutrition Contribute to a Reduction in Sarcopenia, Frailty, and Comorbidities in a Super-Aged Society?
Sadao Yoshida, Ryo Shiraishi, Yuki Nakayama, Yasuko Taira
Nutrients.2023; 15(13): 2991. CrossRef - Safety Profile of Vitamin D in Italy: An Analysis of Spontaneous Reports of Adverse Reactions Related to Drugs and Food Supplements
Valentina Maggini, Giada Crescioli, Ilaria Ippoliti, Eugenia Gallo, Francesca Menniti-Ippolito, Adelaide Chiaravalloti, Vittorio Mascherini, Roberto Da Cas, Simona Potenza, Giulia Gritti, Maria Galiulo, Laura Sottosanti, Alfredo Vannacci, Niccolò Lombardi
Journal of Clinical Medicine.2023; 12(14): 4726. CrossRef - Cholecalciferol Use Is Associated With a Decreased Risk of Incident Morphometric Vertebral Fractures in Acromegaly
Sabrina Chiloiro, Stefano Frara, Irene Gagliardi, Antonio Bianchi, Antonella Giampietro, Margherita Medici, Agnese Allora, Luigi di Filippo, Maria Rosaria Ambrosio, Alfredo Pontecorvi, Maria Chiara Zatelli, Laura De Marinis, Andrea Giustina
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): e58. CrossRef - Proceedings of the 2023 Santa Fe Bone Symposium: Progress and Controversies in the Management of Patients with Skeletal Diseases
E. Michael Lewiecki, Teresita Bellido, John P. Bilezikian, Jacques P. Brown, Azeez Farooki, Christopher S. Kovacs, Brendan Lee, William D. Leslie, Michael R. McClung, Mark L. Prasarn, Deborah E. Sellmeyer
Journal of Clinical Densitometry.2023; 26(4): 101432. CrossRef - Diagnosis, prevention and treatment of vitamin D deficiency in adults: Ukrainian experts consensus statement
N.V. Grygorieva, M.D. Tronko, V.M. Kovalenko, S.V. Komisarenko, T.F. Tatarchuk, N.V. Dedukh, M.M. Veliky, S.S. Strafun, Y.I. Komisarenko, A.V. Kalashnikov, V.L. Orlenko, V.I. Pankiv, O.V. Shvets, I.V. Gogunska, S.I. Regeda
PAIN, JOINTS, SPINE.2023; 13(2): 60. CrossRef - Serum 25-Hydroxyvitamin D Level Is Negatively Associated with Fatigue in Elderly Maintenance Hemodialysis Patients
Menglin Pang, Lin Chen, Na Jiang, Mengmeng Jiang, Baofeng Wang, Lili Wang, Xiao-yan Jia
Kidney and Blood Pressure Research.2023; 48(1): 231. CrossRef - Vitamin D for Clinical Diseases in Women: An Indispensable Factor in Medicine and Dentistry
Dario Calafiore, Leonzio Fortunato, Mario Migliario
Journal of Clinical Medicine.2022; 11(11): 3104. CrossRef - Malnutrition in Older Adults—Effect on Falls and Fractures: A Narrative Review
Malgorzata Kupisz-Urbanska, Ewa Marcinowska-Suchowierska
Nutrients.2022; 14(15): 3123. CrossRef - Role of vitamin D supplementation in the management of musculoskeletal diseases: update from an European Society of Clinical and Economical Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) working group
Thierry Chevalley, Maria Luisa Brandi, Kevin D. Cashman, Etienne Cavalier, Nicholas C. Harvey, Stefania Maggi, Cyrus Cooper, Nasser Al-Daghri, Oliver Bock, Olivier Bruyère, Mario Miguel Rosa, Bernard Cortet, Alfonso J. Cruz-Jentoft, Antonio Cherubini, Bes
Aging Clinical and Experimental Research.2022; 34(11): 2603. CrossRef - The Relationship of Osteoporosis with Menopause: Review of Article
Hadeel Anwar Alsarraje, *Liqaa Khalel Alhyali
International Journal of Research in Medical Sciences and Technology.2022; 14(01): 127. CrossRef
- Ukrainian Consensus on Diagnosis and Management of Vitamin D Deficiency in Adults

- Calcium & Bone Metabolism
- Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature
- Wei Lin Tay, Donovan Tay
- Endocrinol Metab. 2022;37(2):183-194. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1369

- 16,609 View
- 916 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Denosumab, which has been approved for the treatment of osteoporosis since 2010, is a fully humanised monoclonal antibody against a cytokine, receptor activator of nuclear factor kappa B ligand (RANKL), involved in bone resorption. Continued use of denosumab results in a potent and sustained decrease in bone turnover, an increase in bone mineral density (BMD), and a reduction in vertebral and hip fractures. The anti-resorptive effects of denosumab are reversible upon cessation, and this reversal is accompanied by a transient marked increase in bone turnover that is associated with bone loss, and of concern, an increased risk of multiple vertebral fractures. In this review, we outline the effects of denosumab withdrawal on bone turnover markers, BMD, histomorphometry, and fracture risk. We provide an update on recent clinical trials that sought to answer how clinicians can transition away from denosumab safely with follow-on therapy to mitigate bone loss and summarise the recommendations of various international guidelines.
-
Citations
Citations to this article as recorded by- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury
Christopher M. Cirnigliaro, Michael F. La Fountaine, J. Scott Parrott, Steven C. Kirshblum, Susan J. Sauer, Sue A. Shapses, Isa A. McClure, William A. Bauman
Osteoporosis International.2023; 34(4): 741. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef
- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury

- Calcium & Bone Metabolism
Big Data Articles (National Health Insurance Service Database) - Hip Fracture Risk According to Diabetic Kidney Disease Phenotype in a Korean Population
- Seung Eun Lee, Juhwan Yoo, Kyoung-Ah Kim, Kyungdo Han, Han Seok Choi
- Endocrinol Metab. 2022;37(1):148-158. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1315
- 3,686 View
- 120 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
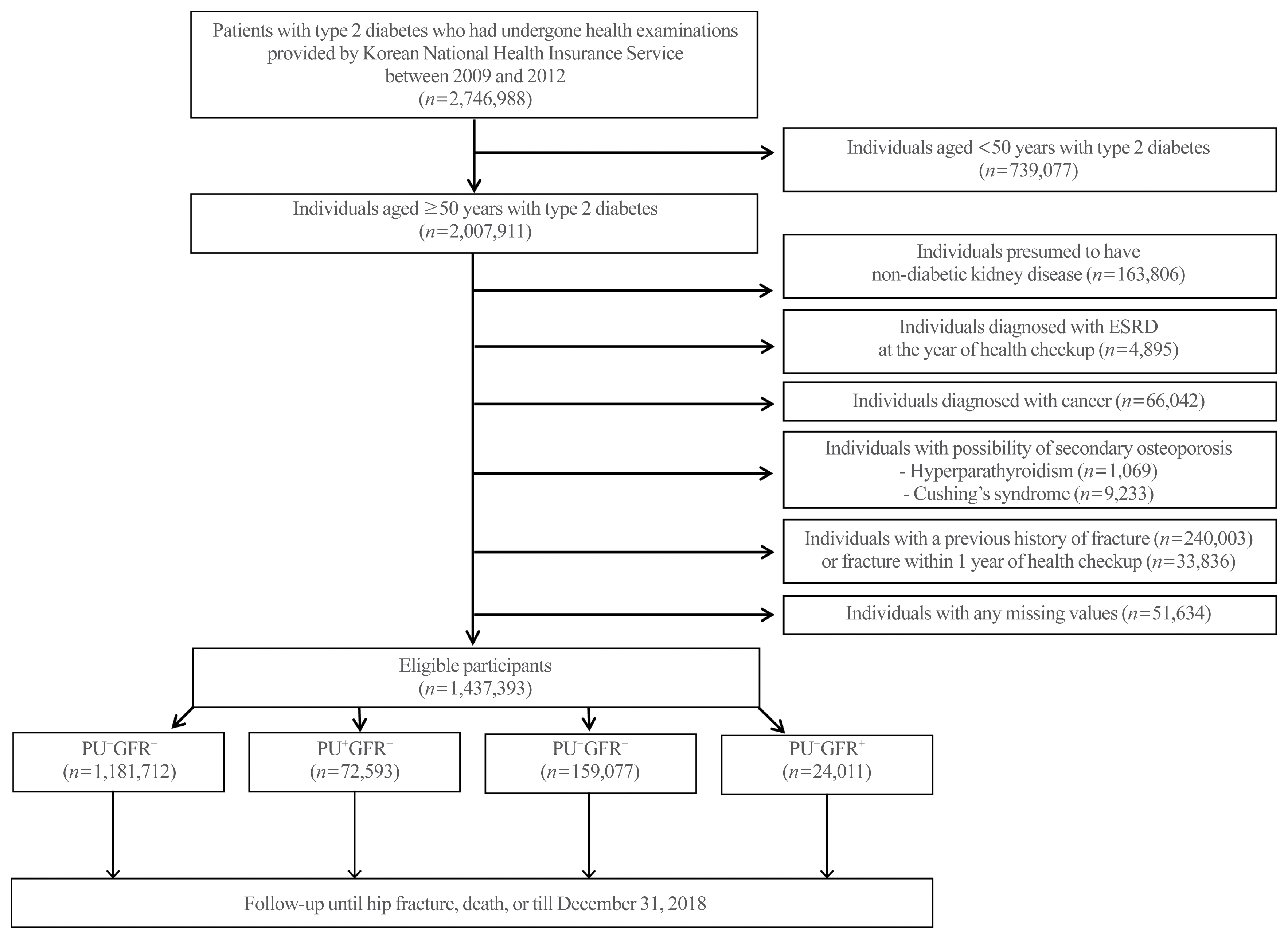
Diabetic kidney disease (DKD) is associated with an elevated risk of fractures. However, little is known about the association between proteinuric or non-proteinuric DKD and the risk of hip fracture. Thus, we investigated the incidence of hip fractures among Korean adults with type 2 diabetes mellitus (T2DM) stratified by DKD phenotype.
Methods
In this retrospective cohort study using the Korean National Health Insurance Service database, patients with T2DM who received at least one general health checkup between 2009 and 2012 were followed until the date of hip fracture, death, or December 31, 2018. We classified the DKD phenotype by proteinuria and estimated glomerular filtration rate (eGFR), as follows: no DKD (PU−GFR−), proteinuric DKD with normal eGFR (PU+GFR−), non-proteinuric DKD with reduced eGFR (PU−GFR+), and proteinuric DKD with reduced eGFR (PU+GFR+)
Results
The cumulative incidence of hip fractures was highest in the PU+GFR+ group, followed by the PU−GFR+ group and the PU+GFR− group. After adjustment for confounding factors, the hazard ratio (HR) for hip fracture was still highest in the PU+GFR+ group. However, the PU+GFR− group had a higher HR for hip fracture than the PU−GFR+ group (PU+GFR+ : HR, 1.69; 95% confidence interval [CI], 1.57 to 1.81; PU+GFR− : HR, 1.37; 95% CI, 1.30 to 1.46; PU−GFR+ : HR, 1.20; 95% CI, 1.16 to 1.24 using the PU−GFR− group as the reference category).
Conclusion
The present study demonstrated that DKD was significantly associated with a higher risk of hip fracture, with proteinuria as a major determinant. -
Citations
Citations to this article as recorded by- Proteinuria screening and risk of bone fracture: a retrospective cohort study using a nationwide population-based database
Akira Okada, Akira Honda, Hideaki Watanabe, Yusuke Sasabuchi, Shotaro Aso, Kayo Ikeda Kurakawa, Masaomi Nangaku, Toshimasa Yamauchi, Hideo Yasunaga, Hirotaka Chikuda, Takashi Kadowaki, Satoko Yamaguchi
Clinical Kidney Journal.2024;[Epub] CrossRef - Fracture risks associated with sodium-glucose cotransporter-2 inhibitors in type 2 diabetes patients across eGFR and albuminuria categories: A population-based study in Hong Kong
David Tak Wai Lui, Tingting Wu, Eric Ho Man Tang, Ivan Chi Ho Au, Chi Ho Lee, Yu Cho Woo, Kathryn Choon Beng Tan, Carlos King Ho Wong
Diabetes Research and Clinical Practice.2023; 197: 110576. CrossRef - Diagnose und Management der Osteoporose bei Diabetes mellitus (Update 2023)
Christian Muschitz, Alexandra Kautzky-Willer, Yvonne Winhofer, Martina Rauner, Judith Haschka, Daniel Cejka, Robert Wakolbinger-Habel, Peter Pietschmann
Wiener klinische Wochenschrift.2023; 135(S1): 207. CrossRef - Association between exercise and risk of fractures in new-onset type 2 diabetes: a retrospective cohort study
Seung Eun Lee, Juhwan Yoo, Bong-Seong Kim, Kyoung-Ah Kim, Kyungdo Han, Han Seok Choi
Archives of Osteoporosis.2023;[Epub] CrossRef - Two-Year Changes in Diabetic Kidney Disease Phenotype and the Risk of Heart Failure: A Nationwide Population-Based Study in Korea
Seung Eun Lee, Juhwan Yoo, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
Diabetes & Metabolism Journal.2023; 47(4): 523. CrossRef
- Proteinuria screening and risk of bone fracture: a retrospective cohort study using a nationwide population-based database

- Calcium & Bone Metabolism
Big Data Articles (National Health Insurance Service Database) - 10-Year Fracture Risk in Postmenopausal Women with Osteopenia and Osteoporosis in South Korea
- Yeon-Hee Baek, Sun Wook Cho, Han Eol Jeong, Ju Hwan Kim, Yunji Hwang, Jeffrey L. Lange, Ju-Young Shin
- Endocrinol Metab. 2021;36(6):1178-1188. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1215
- 5,449 View
- 250 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
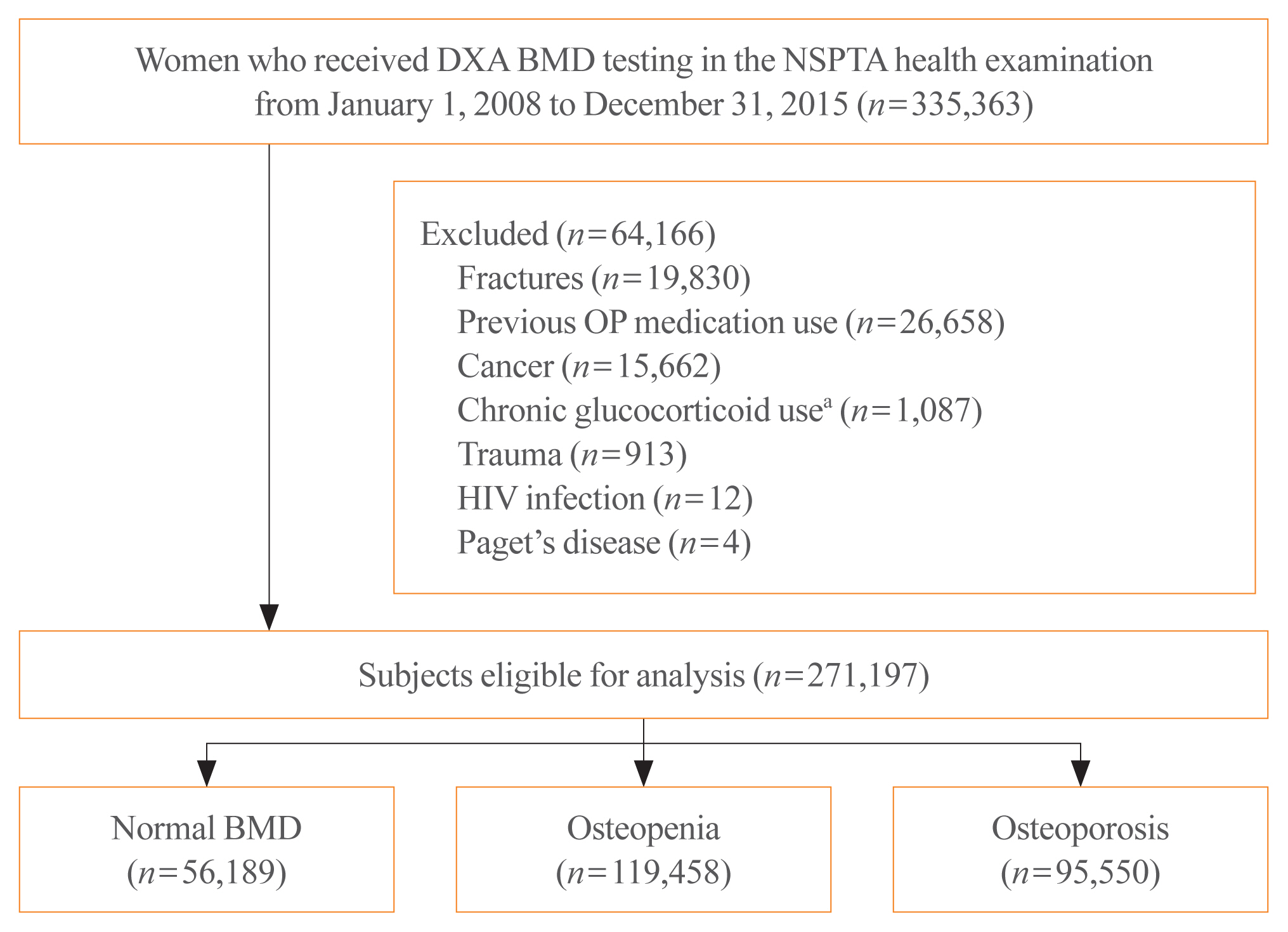
ePub - Background
In South Korea, women aged 66 years are eligible for complimentary bone mineral density (BMD) screening via the National Screening Program for Transitional Ages. We aimed to evaluate the 10-year fracture risk in women receiving BMD screening between January 2008 and December 2015.
Methods
BMD was classified as normal (T-score ≥–1.0 standard deviation [SD]), osteopenia (T-score <–1.0 SD and >–2.5 SD), and osteoporosis (T score ≤–2.5 SD) from dual-energy X-ray absorptiometry. Follow-up continued from the screening date until a diagnosis for clinical fragility fracture (including sites of the vertebrae, hip, pelvis, clavicle, humerus, forearm, wrist, lower leg, and ankle), censored at the earliest date of trauma, death, or December 2017; fracture was ascertained using diagnostic codes from the National Health Insurance Service database. A multivariable Cox proportional hazard model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of fracture in women with osteopenia or osteoporosis relative to women with normal BMD.
Results
Among the 271,197 women screened, 44.0% had osteopenia and 35.2% had osteoporosis. The 10 year cumulative incidence of fragility fractures was 31.1%, 37.5%, and 44.3% in women with normal BMD, osteopenia, and osteoporosis, respectively. Fracture risk was higher in women with osteopenia (HR, 1.31; 95% CI, 1.28 to 1.34) and osteoporosis (HR, 1.68; 95% CI, 1.64 to 1.72) than in women with normal BMD.
Conclusion
Women with osteopenia and women with osteoporosis, identified by the national BMD screening program, demonstrated a substantially elevated risk of fracture. -
Citations
Citations to this article as recorded by- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women
S. Han, S. Kim, E.J. Yeh, H.S. Suh
Osteoporosis International.2024; 35(2): 339. CrossRef - Duration of osteoporosis treatment to reduce the risk of subsequent osteoporotic fracture and all-cause mortality in elderly hip fracture patients in a Korean real-world study
Soong Joon Lee, Minjoon Cho, Hojoon Lee, Hyuna Lim, Jae Hyup Lee
Archives of Osteoporosis.2024;[Epub] CrossRef - Do Patients with Benign Paroxysmal Positional Vertigo Have a Higher Prevalence of Osteoporosis? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Keunho Kim, Yeonjoo Choi
Journal of Personalized Medicine.2024; 14(3): 303. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Chronic airway disease as a major risk factor for fractures in osteopenic women: Nationwide cohort study
Sung Hye Kong, Ae Jeong Jo, Chan Mi Park, Kyun Ik Park, Ji Eun Yun, Jung Hee Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biomimetic Porous Magnesium Alloy Scaffolds Promote the Repair of Osteoporotic Bone Defects in Rats through Activating the Wnt/β-Catenin Signaling Pathway
Yuanchao Zhu, Gaozhi Jia, Yifei Yang, Jian Weng, Su Liu, Mengwei Zhang, Geng Zhang, Haotian Qin, Yixiao Chen, Qi Yang, Guangyin Yuan, Fei Yu, Hui Zeng
ACS Biomaterials Science & Engineering.2023; 9(6): 3435. CrossRef - Correlation between bone mineral density and bone metabolic markers in postmenopausal women with osteoporotic fractures at different C-terminal telopeptide of type 1 collagen levels: a retrospective analysis study
Xiaonan Zhu, Lin Chen, Ling Pan, Yuexi Zeng, Qiang Fu, Yanbin Liu, Yongde Peng, Yufan Wang, Li You
Menopause.2023; 30(11): 1139. CrossRef - Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
Endocrinology and Metabolism.2023; 38(6): 669. CrossRef - A Meaningful Journey to Predict Fractures with Deep Learning
Jeonghoon Ha
Endocrinology and Metabolism.2022; 37(4): 617. CrossRef - The Efficacy of Selective Estrogen Receptor Modulators Monotherapies in Postmenopausal Women with Osteopenia
Kyung Wook Kim, Young Il Kim, Ki-Choul Kim
Journal of Bone Metabolism.2022; 29(3): 185. CrossRef - Correlation of Psoas Muscle Index with Fragility Vertebral Fracture: A Retrospective Cross-Sectional Study of Middle-Aged and Elderly Women
Yihui Zhang, Yilihamu Dilixiati, Wei Jiang, Xiufeng Cao, Yuanyuan Chen, Hui Guo, Christian-Heinz Anderwald
International Journal of Endocrinology.2022; 2022: 1. CrossRef
- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women

- Bone Metabolism
- Operationalizing Treat-to-Target for Osteoporosis
- E. Michael Lewiecki
- Endocrinol Metab. 2021;36(2):270-278. Published online March 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.970
- 5,713 View
- 302 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
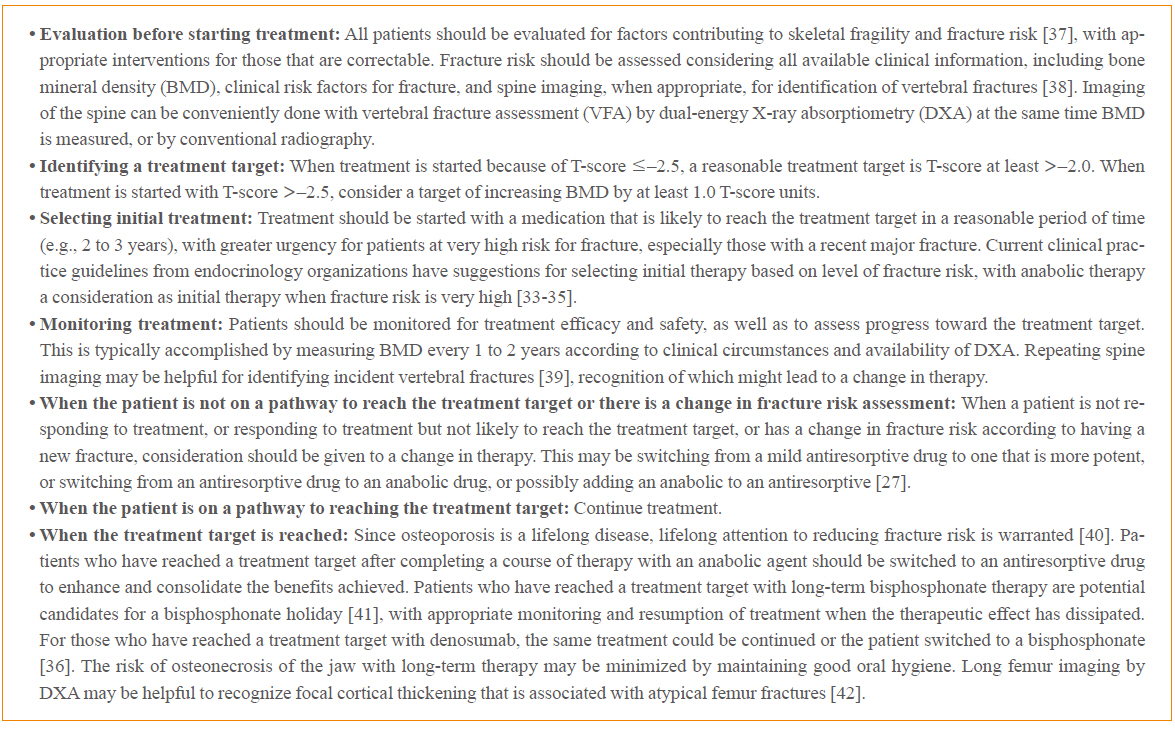
ePub - Treat-to-target (TTT) for osteoporosis is a concept for individualizing patient treatment decisions that focuses on achieving an acceptable level of fracture risk rather than response to treatment alone. While a response to treatment is essential in order to achieve an acceptable level of risk, it is not necessarily sufficient. Some patients have a good response to treatment yet remain at high level of fracture risk. Since there is no way to directly measure bone strength in patients treated for osteoporosis, a surrogate measurement must be used. Bone mineral density (BMD) is commonly used to select patients for treatment and has emerged as the most useful surrogate for assessing reduction of fracture risk after treatment is started. Recent large meta-regression studies have shown a robust correlation between larger increases in BMD with treatment and greater reductions in fracture risk. Application of TTT for osteoporosis involves assessing fracture risk before starting treatment and initiating treatment with an agent that is most likely to reduce fracture risk to an acceptable level, represented by a target BMD T-score, over a reasonable period of time. This review offers suggestions for implementing TTT for osteoporosis in clinical practice and managing patients who fail or succeed in reaching the target. More study is needed to fully validate the use of TTT for osteoporosis for initiating and modifying treatments to reduce fracture risk.
-
Citations
Citations to this article as recorded by- Treatment sequencing using the dual amylin and calcitonin receptor agonist KBP-336 and semaglutide results in durable weight loss
Anna Thorsø Larsen, Morten A. Karsdal, Kim Henriksen
European Journal of Pharmacology.2023; 954: 175837. CrossRef - Osteoporosis: Spotlight on current approaches to pharmacological treatment
Dilşad Sindel
Turkish Journal of Physical Medicine and Rehabilitation.2023; 69(2): 140. CrossRef - Postmenopausal Osteoporosis
Caren G. Solomon, Marcella Donovan Walker, Elizabeth Shane
New England Journal of Medicine.2023; 389(21): 1979. CrossRef - Prevalence and Risk Factors of T-Score Spine-Hip Discordance in Patients with Osteoporotic Vertebral Compression Fracture
Byung-Ho Yoon, Ho Won Kang, Su Min Kim, Young Do Koh
Journal of Bone Metabolism.2022; 29(1): 43. CrossRef - Pharmacological treatment of osteoporosis: 2022 update
Yunkyung Jeon, In-Joo Kim
Journal of the Korean Medical Association.2022; 65(4): 241. CrossRef
- Treatment sequencing using the dual amylin and calcitonin receptor agonist KBP-336 and semaglutide results in durable weight loss

- Bone Metabolism
- Growth and Age-Related Abnormalities in Cortical Structure and Fracture Risk
- Ego Seeman
- Endocrinol Metab. 2015;30(4):419-428. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.419
- 4,521 View
- 65 Download
- 23 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Vertebral fractures and trabecular bone loss have dominated thinking and research into the pathogenesis and the structural basis of bone fragility during the last 70 years. However, 80% of all fractures are non-vertebral and occur at regions assembled using large amounts of cortical bone; only 20% of fractures are vertebral. Moreover, ~80% of the skeleton is cortical and ~70% of all bone loss is cortical even though trabecular bone is lost more rapidly than cortical bone. Bone is lost because remodelling becomes unbalanced after midlife. Most cortical bone loss occurs by intracortical, not endocortical remodelling. Each remodelling event removes more bone than deposited enlarging existing canals which eventually coalesce eroding and thinning the cortex from 'within.' Thus, there is a need to study the decay of cortical as well as trabecular bone, and to develop drugs that restore the strength of both types of bone. It is now possible to accurately quantify cortical porosity and trabecular decay
in vivo . The challenges still to be met are to determine whether measurement of porosity identifies persons at risk for fracture, whether this approach is compliments information obtained using bone densitometry, and whether changes in cortical porosity and other microstructural traits have the sensitivity to serve as surrogates of treatment success or failure.-
Citations
Citations to this article as recorded by- Differences in bone accrual over one year in young girls with obesity compared to Normal weight controls
Vibha Singhal, Snimarjot Kaur, Lea Abou Haidar, Hang Lee, Miriam A. Bredella, Madhusmita Misra
Bone.2023; 172: 116757. CrossRef - The age-related characteristics in bone microarchitecture, osteoclast distribution pattern, functional and transcriptomic alterations of BMSCs in mice
QianKun Yang, ZhiYuan Wei, XiaoYu Wei, Jie Zhang, Yong Tang, Xiang Zhou, Pan Liu, Ce Dou, Fei Luo
Mechanisms of Ageing and Development.2023; 216: 111877. CrossRef - Bilateral asymmetry of bone density adjacent to pelvic sarcomas: A retrospective study using computed tomography
Andrew J. Baines, Ata Babazadeh‐Naseri, Nicholas J. Dunbar, Valerae O. Lewis, Benjamin J. Fregly
Journal of Orthopaedic Research.2022; 40(3): 644. CrossRef - The effect of short-term high-caloric feeding and fasting on bone microarchitecture
Miriam A. Bredella, Pouneh K. Fazeli, Jenna Bourassa, Clifford J. Rosen, Mary L. Bouxsein, Anne Klibanski, Karen K. Miller
Bone.2022; 154: 116214. CrossRef - Image-based radiodensity profilometry measures early remodeling at the bone-callus interface in sheep
Tianyi Ren, Karina Klein, Brigitte von Rechenberg, Salim Darwiche, Hannah L. Dailey
Biomechanics and Modeling in Mechanobiology.2022; 21(2): 615. CrossRef - The action of oxytocin on the bone of senescent female rats
Luís Fernando Gadioli Santos, Fernanda Fernandes-Breitenbach, Rafael Augusto Santos Silva, Damáris Raíssa Santos, Melise Jacon Peres-Ueno, Edilson Ervolino, Antonio Hernandes Chaves-Neto, Rita Cássia Menegati Dornelles
Life Sciences.2022; 297: 120484. CrossRef - Cortical bone material / compositional properties in growing children and young adults aged 1.5–23 years, as a function of gender, age, metabolic activity, and growth spurt
S. Gamsjaeger, F. Rauch, F.H. Glorieux, E.P. Paschalis
Bone.2022; 165: 116548. CrossRef - Age-, Site-, and Sex-Specific Normative Centile Curves for HR-pQCT-Derived Microarchitectural and Bone Strength Parameters in a Chinese Mainland Population
Fan Yu, Yuping Xu, Yanfang Hou, Yuanyuan Lin, Ruizhi Jiajue, Yan Jiang, Ou Wang, Mei Li, Xiaoping Xing, Li Zhang, Ling Qin, Evelyn Hsieh, Weibo Xia
Journal of Bone and Mineral Research.2020; 35(11): 2159. CrossRef - Suboptimal bone microarchitecure in adolescent girls with obesity compared to normal-weight controls and girls with anorexia nervosa
Vibha Singhal, Smriti Sanchita, Sonali Malhotra, Amita Bose, Landy Paola Torre Flores, Ruben Valera, Fatima Cody Stanford, Meghan Slattery, Jennifer Rosenblum, Mark A. Goldstein, Melanie Schorr, Kathryn E. Ackerman, Karen K. Miller, Anne Klibanski, Miriam
Bone.2019; 122: 246. CrossRef - Paget’s Disease of Long Bones: Microstructural Analyses of Historical Bone Samples
Elena Nebot, Patrick Heimel, Stefan Tangl, Martin Dockner, Janina Patsch, Gerhard W. Weber, Michael Pretterklieber, Maria Teschler-Nicola, Peter Pietschmann
Calcified Tissue International.2019; 105(1): 15. CrossRef - Adding Marrow Adiposity and Cortical Porosity to Femoral Neck Areal Bone Mineral Density Improves the Discrimination of Women With Nonvertebral Fractures From Controls
Roger Zebaze, Marit Osima, Minh Bui, Marko Lukic, Xiaofang Wang, Ali Ghasem-Zadeh, Erik F Eriksen, Angela Vais, Catherine Shore-Lorenti, Peter R Ebeling, Ego Seeman, Åshild Bjørnerem
Journal of Bone and Mineral Research.2019; 34(8): 1451. CrossRef - Assessing Cortical Thickness in Human Tibiae With Sonography vs Computed Tomography: A Pilot Study
Sundus H. Mohammad, Randee L. Hunter, Rachel L. Tatarski, Angela N. Butwin, Kevin D. Evans
Journal of Diagnostic Medical Sonography.2018; 34(3): 170. CrossRef - Understanding age-induced cortical porosity in women: Is a negative BMU balance in quiescent osteons a major contributor?
Christina M. Andreasen, Jean-Marie Delaisse, Bram C.J. van der Eerden, Johannes P.T.M. van Leeuwen, Ming Ding, Thomas L. Andersen
Bone.2018; 117: 70. CrossRef - Intracortical Bone Mechanics Are Related to Pore Morphology and Remodeling in Human Bone
Lydia P Bakalova, Christina M Andreasen, Jesper Skovhus Thomsen, Annemarie Brüel, Ellen-Margrethe Hauge, Birgitte Jul Kiil, Jean-Marie Delaisse, Thomas Levin Andersen, Mariana E Kersh
Journal of Bone and Mineral Research.2018; 33(12): 2177. CrossRef - Diversity in intracortical remodeling in the human femoral bone: A novel view point with the morphological analysis of secondary osteons
Junichiro Maeda, Kazunobu Saiki, Hisayoshi Kondo, Hiroaki Matsuo, Takeshi Imamura, Keiko Ogami-Takamura, Keishi Okamoto, Masato Tomita, Makoto Osaki, Toshiyuki Tsurumoto
Journal of Orthopaedic Science.2018; 23(6): 1079. CrossRef - Women with fracture, unidentified by FRAX, but identified by cortical porosity, have a set of characteristics that contribute to their increased fracture risk beyond high FRAX score and high cortical porosity
Rita Kral, Marit Osima, Roald Vestgaard, Elin Richardsen, Åshild Bjørnerem
Bone.2018; 116: 259. CrossRef - Response to “Clinical Evaluation of Bone Strength and Fracture Risk”
Anne B. Loucks, Brian C. Clark, Lyn Bowman
Current Osteoporosis Reports.2017; 15(4): 396. CrossRef - Ovarian hormone depletion affects cortical bone quality differently on different skeletal envelopes
E.P. Paschalis, S. Gamsjaeger, N. Hassler, K. Klaushofer, D. Burr
Bone.2017; 95: 55. CrossRef - Chronic Hyperglycemia Modulates Rat Osteoporotic Cortical Bone Microarchitecture into Less Fragile Structures
Cristina de Mello-Sampayo, Alaíde Alves Agripino, Duarte Stilwell, Bruno Vidal, Ana Luisa Fernando, Beatriz Silva-Lima, Maria Fátima Vaz, Helena Canhão, M. Cristina Marques
International Journal of Endocrinology.2017; 2017: 1. CrossRef - The Association of Higher Plasma Macrophage Migration Inhibitory Factor Levels with Lower Bone Mineral Density and Higher Bone Turnover Rate in Postmenopausal Women
Hyeonmok Kim, Seong Hee Ahn, Chaeho Shin, Seung Hun Lee, Beom-Jun Kim, Jung-Min Koh
Endocrinology and Metabolism.2016; 31(3): 454. CrossRef - Intraskeletal variation in human cortical osteocyte lacunar density: Implications for bone quality assessment
Randee L. Hunter, Amanda M. Agnew
Bone Reports.2016; 5: 252. CrossRef - The Bindex®ultrasound device: reliability of cortical bone thickness measures and their relationship to regional bone mineral density
Martin Behrens, Sabine Felser, Anett Mau-Moeller, Matthias Weippert, Johannes Pollex, Ralf Skripitz, Philipp K E Herlyn, Dagmar-C Fischer, Sven Bruhn, Hans-Christof Schober, Volker Zschorlich, Thomas Mittlmeier
Physiological Measurement.2016; 37(9): 1528. CrossRef
- Differences in bone accrual over one year in young girls with obesity compared to Normal weight controls

- Bone Metabolism
- Epidemiology of Osteoporosis and Osteoporotic Fractures in South Korea
- Young-Kyun Lee, Byung-Ho Yoon, Kyung-Hoi Koo
- Endocrinol Metab. 2013;28(2):90-93. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.90
- 4,984 View
- 61 Download
- 40 Web of Science
- 44 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Several epidemiologic studies suggested that osteoporosis and osteoporotic fractures are not uncommon in South Korea. However, these previous cohort studies had limitations that may have influenced their results and the generalizability of the study conclusions, including small sample sizes, inclusion of only women, enrollment of participants from specific areas, and nonrandom selection of participants. Recently, epidemiologic studies using a nationwide claim register have been performed to overcome these limitations through collaboration between the Korean Society of Bone and Mineral Research and Health Insurance Review Assessments. Our review of the Korean Nationwide-database Osteoporosis Study could be helpful to obtain accurate incidence and prevalence estimations of osteoporosis and osteoporosis-related fractures in Korea.
-
Citations
Citations to this article as recorded by- The 2024 Guidelines for Osteoporosis - Korean Society of Menopause
Dong Ock Lee, Yeon Hee Hong, Moon Kyoung Cho, Young Sik Choi, Sungwook Chun, Youn-Jee Chung, Seung Hwa Hong, Kyu Ri Hwang, Jinju Kim, Hoon Kim, Dong-Yun Lee, Sa Ra Lee, Hyun-Tae Park, Seok Kyo Seo, Jung-Ho Shin, Jae Yen Song, Kyong Wook Yi, Haerin Paik, J
Journal of Menopausal Medicine.2024; 30(1): 1. CrossRef - Tuberculosis and osteoporotic fracture risk: development of individualized fracture risk estimation prediction model using a nationwide cohort study
Hayoung Choi, Jungeun Shin, Jin-Hyung Jung, Kyungdo Han, Wonsuk Choi, Han Rim Lee, Jung Eun Yoo, Yohwan Yeo, Hyun Lee, Dong Wook Shin
Frontiers in Public Health.2024;[Epub] CrossRef - Prevalence of osteoporosis and incidence of related fractures in developed economies in the Asia Pacific region: a systematic review
Manju Chandran, Katherine Brind’Amour, Saeko Fujiwara, Yong-Chan Ha, Hai Tang, Jawl-Shan Hwang, James Tinker, John A. Eisman
Osteoporosis International.2023; 34(6): 1037. CrossRef - Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial
Chaiho Jeong, Jeonghoon Ha, Jun-Il Yoo, Young-Kyun Lee, Jung Hee Kim, Yong-Chan Ha, Yong-Ki Min, Dong-Won Byun, Ki-Hyun Baek, Ho Yeon Chung
Journal of Bone Metabolism.2023; 30(2): 189. CrossRef - Risk of Fractures in Thyroid Cancer Patients With Postoperative Hypoparathyroidism: A Nationwide Cohort Study in Korea
Seong Hee Ahn, You Jin Lee, Seongbin Hong, Jung Wee Park, Ye Jhin Jeon, Bit‐Na Yoo, Yong‐Chan Ha, Jean Kyung Bak, Ha Young Kim, Young‐Kyun Lee
Journal of Bone and Mineral Research.2023; 38(9): 1268. CrossRef - Impact of changes in physical activity and incident fracture after acute ischemic stroke
Dae young Cheon, Kyung-Do Han, Jeen Hwa Lee, Kyung-Ho Yu, Bo Young Choi, Minwoo Lee
Scientific Reports.2023;[Epub] CrossRef - Associations between Long-Term Air Pollution Exposure and Risk of Osteoporosis-Related Fracture in a Nationwide Cohort Study in South Korea
Seulkee Heo, Honghyok Kim, Sera Kim, Seung-Ah Choe, Garam Byun, Jong-Tae Lee, Michelle L. Bell
International Journal of Environmental Research and Public Health.2022; 19(4): 2404. CrossRef - Significance of Measuring Lumbar Spine 3-Dimensional Computed Tomography Hounsfield Units to Predict Screw Loosening
Kyeong Hwan Kim, Tae-Hwan Kim, Seok Woo Kim, Ji Hee Kim, Heui Seung Lee, In Bok Chang, Joon Ho Song, Yong-Kil Hong, Jae Keun Oh
World Neurosurgery.2022; 165: e555. CrossRef - Risk of osteoporotic fracture in older patients under antihypertensive treatment
Oh Kyung Kwon, Sun-Hwa Kim, Si-Hyuck Kang, Young-Kyun Lee, Chang-Hwan Yoon, Hae-Young Lee, Tae-Jin Youn, In-Ho Chae, Cheol-Ho Kim
European Journal of Preventive Cardiology.2021; 28(11): e12. CrossRef - Risk factors for subsequent vertebral fractures following a previous hip fracture
Sang-Min Park, Sung Jun Go, Heesoo Han, Jung Wee Park, Young-Kyun Lee, Ho-Joong Kim, Jin S. Yeom, Kyung-Hoi Koo
Journal of Bone and Mineral Metabolism.2021; 39(2): 193. CrossRef - Characteristics of Osteoporosis & Osteoporotic Fractures in Korea Based on Health Insurance Review and Assessment (HIRA) Database: 2009–2017
Ho-Seok Oh, Sung-Kyu Kim, Hyoung-Yeon Seo
Healthcare.2021; 9(3): 324. CrossRef - Association between Irritable Bowel Syndrome and Risk of Osteoporosis in Korean Premenopausal Women
Sang-Yeoup Lee, Hye-Rim Hwang, Yu-Hyeon Yi, Jin-Mi Kim, Yun-Jin Kim, Jeong-Gyu Lee, Young-Hye Cho, Young-Jin Tak, Seung Hun Lee, Eun Ju Park, Youngin Lee
Medical Principles and Practice.2021; 30(6): 527. CrossRef - Association Between Acetylcholinesterase Inhibitors and Osteoporotic Fractures in Older Persons With Alzheimer's Disease
Dae Yeon Won, Seong Jun Byun, Jin Sook Jeong, Ju-Young Shin
Journal of the American Medical Directors Association.2020; 21(8): 1128. CrossRef - High Circulating Sphingosine 1-Phosphate is a Risk Factor for Osteoporotic Fracture Independent of Fracture Risk Assessment Tool
Seung Hun Lee, Jee Yang Lee, Kyeong-Hye Lim, Young-Sun Lee, Seong-Hee Kim, Sooyoung Choi, Seong-Hwan Cho, Jung-Min Koh
Calcified Tissue International.2020; 107(4): 362. CrossRef - Osteoporosis and Osteoporotic Fracture Fact Sheet in Korea
Seong Hee Ahn, Sang-Min Park, So Young Park, Jun-Il Yoo, Hyoung-Seok Jung, Jae-Hwi Nho, Se Hwa Kim, Young-Kyun Lee, Yong-Chan Ha, Sunmee Jang, Tae-Young Kim, Ha Young Kim
Journal of Bone Metabolism.2020; 27(4): 281. CrossRef - Assessing the effects of National Health Insurance reimbursement policy revisions for anti-osteoporotic drugs in Korean women aged 50 or older
Ja Seo Koo, Seong Hwan Moon, Hankil Lee, Sohee Park, Yun Mi Yu, Hye-Young Kang, Robert Daniel Blank
PLOS ONE.2020; 15(12): e0244759. CrossRef - The Epidemiology of Fracture in Patients with Acute Ischemic Stroke in Korea
Kyung Bok Lee, Jung-Gon Lee, Beom Joon Kim, Jun Yup Kim, Keon-Joo Lee, Moon-Ku Han, Jong-Moo Park, Kyusik Kang, Yong-Jin Cho, Hong-Kyun Park, Keun-Sik Hong, Tai Hwan Park, Soo Joo Lee, Mi-Sun Oh, Kyung-Ho Yu, Byung-Chul Lee, Jae-Kwan Cha, Dae-Hyun Kim, Jo
Journal of Korean Medical Science.2019;[Epub] CrossRef - Osteoporosis detection in panoramic radiographs using a deep convolutional neural network-based computer-assisted diagnosis system: a preliminary study
Jae-Seo Lee, Shyam Adhikari, Liu Liu, Ho-Gul Jeong, Hyongsuk Kim, Suk-Ja Yoon
Dentomaxillofacial Radiology.2019; 48(1): 20170344. CrossRef - Medical Big Data Is Not Yet Available: Why We Need Realism Rather than Exaggeration
Hun-Sung Kim, Dai-Jin Kim, Kun-Ho Yoon
Endocrinology and Metabolism.2019; 34(4): 349. CrossRef - Adherence to a Mediterranean Diet and Bone Mineral Density in Spanish Premenopausal Women
Jesús Pérez-Rey, Raúl Roncero-Martín, Sergio Rico-Martín, Purificación Rey-Sánchez, Juan Pedrera-Zamorano, María Pedrera-Canal, Fidel López-Espuela, Jesús Lavado García
Nutrients.2019; 11(3): 555. CrossRef - Effect of Training and Testing Condition of Convolutional Neural Network on evaluating Osteoporosis
Jae-Yun Kim, Jae-Seo Lee, Byung-Cheol Kang, Hyongsuk Kim, Shyam Adhikari, Liu Liu, Suk-Ja Yoon
The Korean Journal of Oral and Maxillofacial Pathology.2019; 43(3): 73. CrossRef - Comparison of intraoperative radiation exposure with and without use of distal targeting device: a randomized control study
Jun-Il Yoo, Hojin Jeong, Jaeboem Na, Sang-Youn Song, Jung-Taek Kim, Yong-Han Cha, Chan Ho Park
Archives of Orthopaedic and Trauma Surgery.2019; 139(11): 1579. CrossRef - Anemia and Risk of Fractures in Older Korean Adults: A Nationwide Population-Based Study
Eun Ae Lee, Dong Wook Shin, Jun Hyun Yoo, Hyeon Young Ko, Su Min Jeong
Journal of Bone and Mineral Research.2019; 34(6): 1049. CrossRef - Elevated ceramides 18:0 and 24:1 with aging are associated with hip fracture risk through increased bone resorption
Beom-Jun Kim, Jin Young Lee, So Jeong Park, Seung Hum Lee, Su Jung Kim, Hyun Ju Yoo, Sarah I. Rivera De Pena, Meghan McGee-Lawrence, Carlos M. Isales, Jung-Min Koh, Mark W. Hamrick
Aging.2019; 11(21): 9388. CrossRef - Effect of improved medication adherence on health care costs in osteoporosis patients
Hyemin Cho, Ji-Hye Byun, Inmyung Song, Ha Y. Kim, Yong-Chan Ha, Tae-Young Kim, Young-Kyun Lee, Sunmee Jang
Medicine.2018; 97(30): e11470. CrossRef - Osteoporosis and fracture after gastrectomy for stomach cancer
Gi Hyeon Seo, Hae Yeon Kang, Eun Kyung Choe
Medicine.2018; 97(17): e0532. CrossRef - Inflammation inhibitory effect of water extract from pumpkin’s tendril
Ha-Na Jeong, Ju-Hee Choi, Ha-Nul Lee, So-Hyeon Lee, Soon-Chang Cho, Jong-Hwan Park, Young-Min Kim
Korean Journal of Food Preservation.2017; 24(8): 1122. CrossRef - Strong familial association of bone mineral density between parents and offspring: KNHANES 2008–2011
H. S. Choi, J. H. Park, S. H. Kim, S. Shin, M. J. Park
Osteoporosis International.2017; 28(3): 955. CrossRef - Vertebral bone attenuation on low-dose chest CT: quantitative volumetric analysis for bone fragility assessment
Y. W. Kim, J. H. Kim, S. H. Yoon, J. H. Lee, C.-H. Lee, C. S. Shin, Y. S. Park
Osteoporosis International.2017; 28(1): 329. CrossRef - Factors Affecting Bone Mineral Density Measurement after Fracture in South Korea
Jin-Woo Kim, Yong-Chan Ha, Young-Kyun Lee
Journal of Bone Metabolism.2017; 24(4): 217. CrossRef - Femoral geometry, bone mineral density, and the risk of hip fracture in premenopausal women: a case control study
Dong-Hwa Lee, Kyong Yeun Jung, A Ram Hong, Jung Hee Kim, Kyoung Min Kim, Chan Soo Shin, Seong Yeon Kim, Sang Wan Kim
BMC Musculoskeletal Disorders.2016;[Epub] CrossRef - The Association of Higher Plasma Macrophage Migration Inhibitory Factor Levels with Lower Bone Mineral Density and Higher Bone Turnover Rate in Postmenopausal Women
Hyeonmok Kim, Seong Hee Ahn, Chaeho Shin, Seung Hun Lee, Beom-Jun Kim, Jung-Min Koh
Endocrinology and Metabolism.2016; 31(3): 454. CrossRef - Oral Bisphosphonates and Upper Gastrointestinal Cancer Risks in Asians with Osteoporosis: A Nested Case-Control Study Using National Retrospective Cohort Sample Data from Korea
Sun-Young Jung, Hyun Soon Sohn, Eun-Ja Park, Hae Sun Suh, Ji-Won Park, Jin-Won Kwon, Chi-Ling Chen
PLOS ONE.2016; 11(3): e0150531. CrossRef - The effects of body mass index on the hereditary influences that determine peak bone mass in mother–daughter pairs (KNHANES V)
K. M. Kim, Y. J. Kim, S. H. Choi, S. Lim, J. H. Moon, J. H. Kim, S. W. Kim, H. C. Jang, C. S. Shin
Osteoporosis International.2016; 27(6): 2057. CrossRef - Low Bone Mineral Density Is Associated with Tooth Loss in Postmenopausal Women: A Nationwide Representative Study in Korea
Soyeon Ji, Young Jin Tak, Dong Hun Han, Yun Jin Kim, Sang Yeoup Lee, Jeong Gyu Lee, Dong Wook Jeong, Min Ji Kim
Journal of Women's Health.2016; 25(11): 1159. CrossRef - The circulating sphingosine-1-phosphate level predicts incident fracture in postmenopausal women: a 3.5-year follow-up observation study
S. J. Bae, S. H. Lee, S. H. Ahn, H.-M. Kim, B.-J. Kim, J.-M. Koh
Osteoporosis International.2016; 27(8): 2533. CrossRef - Is central skeleton bone quality a predictor of the severity of proximal humeral fractures?
Seung Yeol Lee, Soon-Sun Kwon, Tae Hoon Kim, Sang-Jin Shin
Injury.2016; 47(12): 2777. CrossRef - Association of the TREML2 and HTR1E Genetic Polymorphisms with Osteoporosis
Dongju Jung, Hyun-Seok Jin
Biomedical Science Letters.2015; 21(4): 181. CrossRef - A Large National Cohort Study of the Association between Bisphosphonates and Osteonecrosis of the Jaw in Patients with Osteoporosis
J.-W. Kwon, E.-J. Park, S.-Y. Jung, H.S. Sohn, H. Ryu, H.S. Suh
Journal of Dental Research.2015; 94(9_suppl): 212S. CrossRef - Reliability and validity of lower extremity computed tomography as a screening tool for osteoporosis
S. Y. Lee, S.-S. Kwon, H. S. Kim, J. H. Yoo, J. Kim, J. Y. Kim, B. C. Min, S. J. Moon, K. H. Sung
Osteoporosis International.2015; 26(4): 1387. CrossRef - Osteoporosis in Healthy South Indian Males and the Influence of Life Style Factors and Vitamin D Status on Bone Mineral Density
Sahana Shetty, Nitin Kapoor, Dukhabandhu Naik, Hesarghatta Shyamasunder Asha, Suresh Prabu, Nihal Thomas, Mandalam Subramaniam Seshadri, Thomas Vizhalil Paul
Journal of Osteoporosis.2014; 2014: 1. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Association of osteoporosis susceptibility genes with bone mineral density and bone metabolism related markers in Koreans: The Chungju Metabolic Disease Cohort (CMC) study
Se Eun Park, Ki Won Oh, Won Young Lee, Ki Hyun Baek, Kun Ho Yoon, Ho Young Son, Won Chul Lee, Moo Il Kang
Endocrine Journal.2014; 61(11): 1069. CrossRef - Management of Osteoporosis: Who to Treat, What to Use, and for How Long?
Sang Wan Kim
Korean Journal of Medicine.2013; 85(4): 364. CrossRef
- The 2024 Guidelines for Osteoporosis - Korean Society of Menopause

- Pregnancy-induced Osteoporosis Combined with Multiple Compression Fractures: A Case Report.
- Ji Eun Lee, Jin Sun Jang, Sun Hee Ko, Min Hee Kim, Dong Jun Lim, Moo Il Kang, Bong Yun Cha, Sook Hee Hong, Ja seong Bae, Kyeoung Sik Ryu
- Endocrinol Metab. 2011;26(2):150-154. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.150
- 2,109 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pregnancy associated osteoporosis (PAO) is a rare condition. It may affect women during pregnancy or after the delivery and it can induce severe back pain. Physicians can find multiple compression fractures on the plain images of these patients. However, little is known about PAO, including the prevalence, the cause, the risk factors and the prognosis. Herein we report on a case of PAO in a 38-year-old female who suffered from severe back pain induced by multiple vertebral compression fractures. After excluding the possibility of unknown malignancy, the patient underwent vertebroplasty to improve the clinical symptom. The bone biopsy results confirmed multiple benign acute compression fractures. The patient was treated with oral bisphosphonate, calcium and vitamin D. She showed clinical improvement without developing any additional vertebral fracture. When young women during pregnancy or just after the delivery complain of persistent back pain, PAO should be considered in the differential diagnosis, and early recognition and treatment are needed for PAO.
-
Citations
Citations to this article as recorded by- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures
Eun Yeong Choe, Je Eun Song, Kyeong Hye Park, Hannah Seok, Eun Jig Lee, Sung-Kil Lim, Yumie Rhee
Journal of Bone and Mineral Metabolism.2012; 30(5): 596. CrossRef
- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures


 KES
KES

 First
First Prev
Prev



