Big Data Articles
(National Health Insurance Service Database)
- Page Path
-
HOME
> BROWSE ARTICLES
> Big Data Articles
(National Health Insurance Service Database)
Original Articles
- Diabetes, obesity and metabolism
Big Data Articles (National Health Insurance Service Database) - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
- Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
- Endocrinol Metab. 2023;38(6):770-781. Published online November 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1726
- 1,110 View
- 48 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
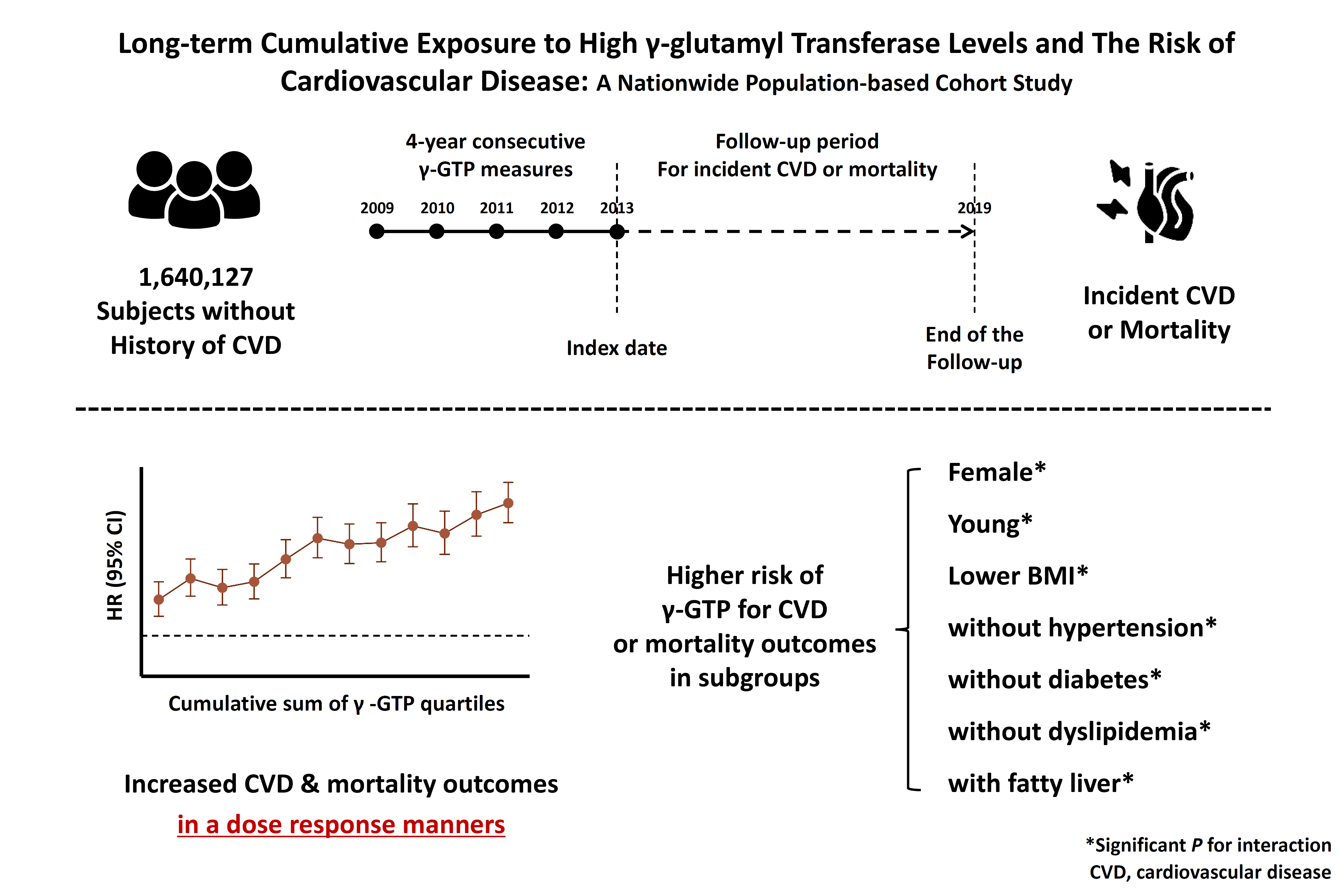
Elevated γ-glutamyl transferase (γ-GTP) levels are associated with metabolic syndrome. We investigated the association of cumulative exposure to high γ-GTP with the risk of cardiovascular disease (CVD) in a large-scale population.
Methods
Using nationally representative data from the Korean National Health Insurance system, 1,640,127 people with 4 years of consecutive γ-GTP measurements from 2009 to 2012 were included and followed up until the end of 2019. For each year of the study period, participants were grouped by the number of exposures to the highest γ-GTP quartile (0–4), and the sum of quartiles (0–12) was defined as cumulative γ-GTP exposure. The hazard ratio for CVD was evaluated using the Cox proportional hazards model.
Results
During the 6.4 years of follow-up, there were 15,980 cases (0.97%) of myocardial infarction (MI), 14,563 (0.89%) of stroke, 29,717 (1.81%) of CVD, and 25,916 (1.58%) of death. Persistent exposure to high γ-GTP levels was associated with higher risks of MI, stroke, CVD, and death than those without such exposure. The risks of MI, stroke, CVD, and mortality increased in a dose-dependent manner according to total cumulative γ-GTP (all P for trend <0.0001). Subjects younger than 65 years, with a body mass index <25 kg/m2, and without hypertension or fatty liver showed a stronger relationship between cumulative γ-GTP and the incidence of MI, CVD, and death.
Conclusion
Cumulative γ-GTP elevation is associated with CVD. γ-GTP could be more widely used as an early marker of CVD risk, especially in individuals without traditional CVD risk factors.

- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
- Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
- Endocrinol Metab. 2023;38(6):690-700. Published online October 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1782

- 1,353 View
- 92 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Acromegaly leads to various skeletal complications, and fragility fractures are emerging as a new concern in patients with acromegaly. Therefore, this study investigated the risk of fractures in Korean patients with acromegaly.
Methods
We used the Korean nationwide claims database from 2009 to 2019. A total of 931 patients with acromegaly who had never used an osteoporosis drug before and were treated with surgery alone were selected as study participants, and a 1:29 ratio of 26,999 age- and sex-matched osteoporosis drug-naïve controls without acromegaly were randomly selected from the database.
Results
The mean age was 46.2 years, and 50.0% were male. During a median follow-up of 54.1 months, there was no difference in the risks of all, vertebral, and non-vertebral fractures between the acromegaly and control groups. However, hip fracture risk was significantly higher (hazard ratio [HR], 2.73; 95% confidence interval [CI], 1.32 to 5.65), and non-hip and non-vertebral fractures risk was significantly lower (HR, 0.40; 95% CI, 0.17 to 0.98) in patients with acromegaly than in controls; these results remained robust even after adjustment for socioeconomic status and baseline comorbidities. Age, type 2 diabetes mellitus, cardio-cerebrovascular disease, fracture history, recent use of acid-suppressant medication, psychotropic medication, and opioids were risk factors for all fractures in patients with acromegaly (all P<0.05).
Conclusion
Compared with controls, patients surgically treated for acromegaly had a higher risk of hip fractures. The risk factors for fracture in patients with acromegaly were consistent with widely accepted risk factors in the general population.

- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2023;38(6):679-689. Published online December 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1760

- 1,181 View
- 66 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Limited longitudinal evidence exists regarding the potential association between smoking status and hip fracture among individuals with type 2 diabetes. We investigated this association using large-scale, nationwide cohort data for the Korean population.
Methods
This nationwide cohort study included 1,414,635 adults aged 40 and older who received Korean National Health Insurance Service health examinations between 2009 and 2012. Subjects with type 2 diabetes were categorized according to their smoking status, amount smoked (pack-years), number of cigarettes smoked per day, and duration of smoking. The results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between smoking status parameters and risk of hip fracture in multivariable Cox proportional hazard regression analysis.
Results
Compared with never-smokers, an increased adjusted HR (aHR) for hip fracture was observed in current smokers (1.681; 95% CI, 1.578 to 1.791), and a comparable aHR for hip fracture was found in former smokers (1.065; 95% CI, 0.999 to 1.136). For former smokers who had smoked 20 pack-years or more, the risk was slightly higher than that for never-smokers (aHR, 1.107; 95% CI, 1.024 to 1.196). The hip fracture risk of female former smokers was similar to that of female current smokers, but the hip fracture risk in male former smokers was similar to that of male never-smokers.
Conclusion
Smoking is associated with an increased risk of hip fracture in patients with type 2 diabetes. Current smokers with diabetes should be encouraged to quit smoking because the risk of hip fracture is greatly reduced in former smokers.

- Diabetes, obesity and metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
- Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee, Committee of Big Data, Korean Endocrine Society
- Endocrinol Metab. 2023;38(5):525-537. Published online September 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1765
- 1,569 View
- 91 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
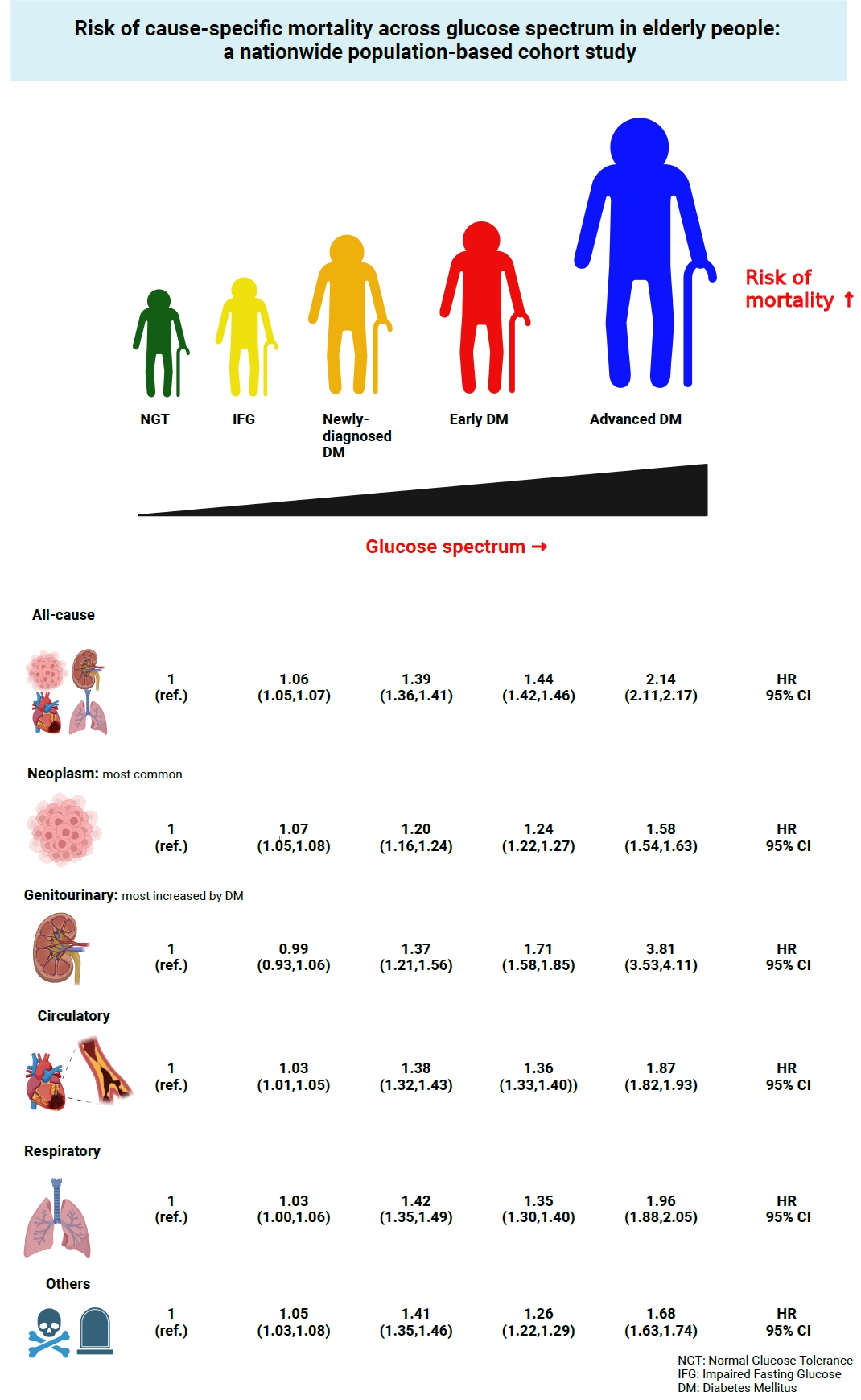
This study investigated the risk of cause-specific mortality according to glucose tolerance status in elderly South Koreans.
Methods
A total of 1,292,264 individuals aged ≥65 years who received health examinations in 2009 were identified from the National Health Information Database. Participants were classified as normal glucose tolerance, impaired fasting glucose, newly-diagnosed diabetes, early diabetes (oral hypoglycemic agents ≤2), or advanced diabetes (oral hypoglycemic agents ≥3 or insulin). The risk of system-specific and disease-specific deaths was estimated using multivariate Cox proportional hazards analysis.
Results
During a median follow-up of 8.41 years, 257,356 deaths were recorded. Diabetes was associated with significantly higher risk of all-cause mortality (hazard ratio [HR], 1.58; 95% confidence interval [CI], 1.57 to 1.60); death due to circulatory (HR, 1.49; 95% CI, 1.46 to 1.52), respiratory (HR, 1.51; 95% CI, 1.47 to 1.55), and genitourinary systems (HR, 2.22; 95% CI, 2.10 to 2.35); and neoplasms (HR, 1.30; 95% CI, 1.28 to 1.32). Diabetes was also associated with a significantly higher risk of death due to ischemic heart disease (HR, 1.70; 95% CI, 1.63 to 1.76), cerebrovascular disease (HR, 1.46; 95% CI, 1.41 to 1.50), pneumonia (HR, 1.69; 95% CI, 1.63 to 1.76), and acute or chronic kidney disease (HR, 2.23; 95% CI, 2.09 to 2.38). There was a stepwise increase in the risk of death across the glucose spectrum (P for trend <0.0001). Stroke, heart failure, or chronic kidney disease increased the risk of all-cause mortality at every stage of glucose intolerance.
Conclusion
A dose-dependent association between the risk of mortality from various causes and severity of glucose tolerance was noted in the elderly population. -
Citations
Citations to this article as recorded by- The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef
- The Characteristics and Risk of Mortality in the Elderly Korean Population

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
- Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1684
- 1,804 View
- 127 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
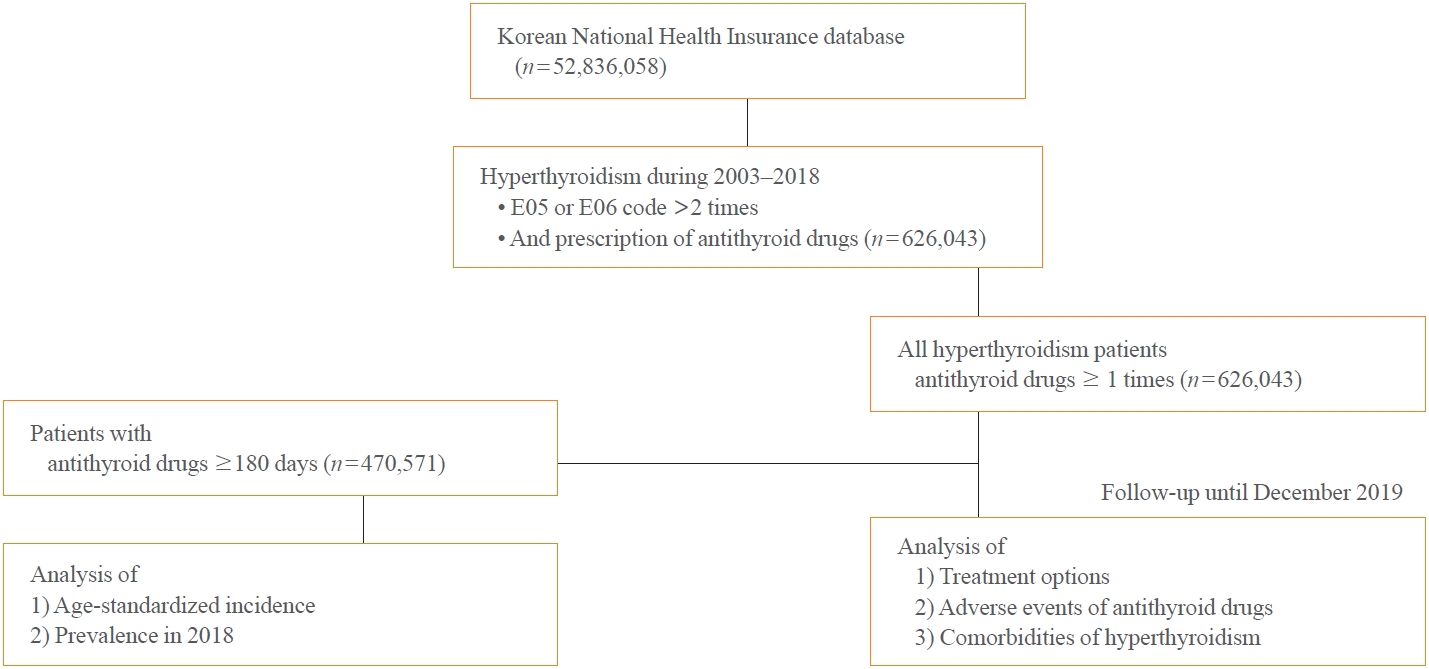
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age. -
Citations
Citations to this article as recorded by- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients

- Adrenal gland
Big Data Articles (National Health Insurance Service Database) - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
- Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
- Endocrinol Metab. 2023;38(2):253-259. Published online March 21, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1607
- 2,587 View
- 103 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
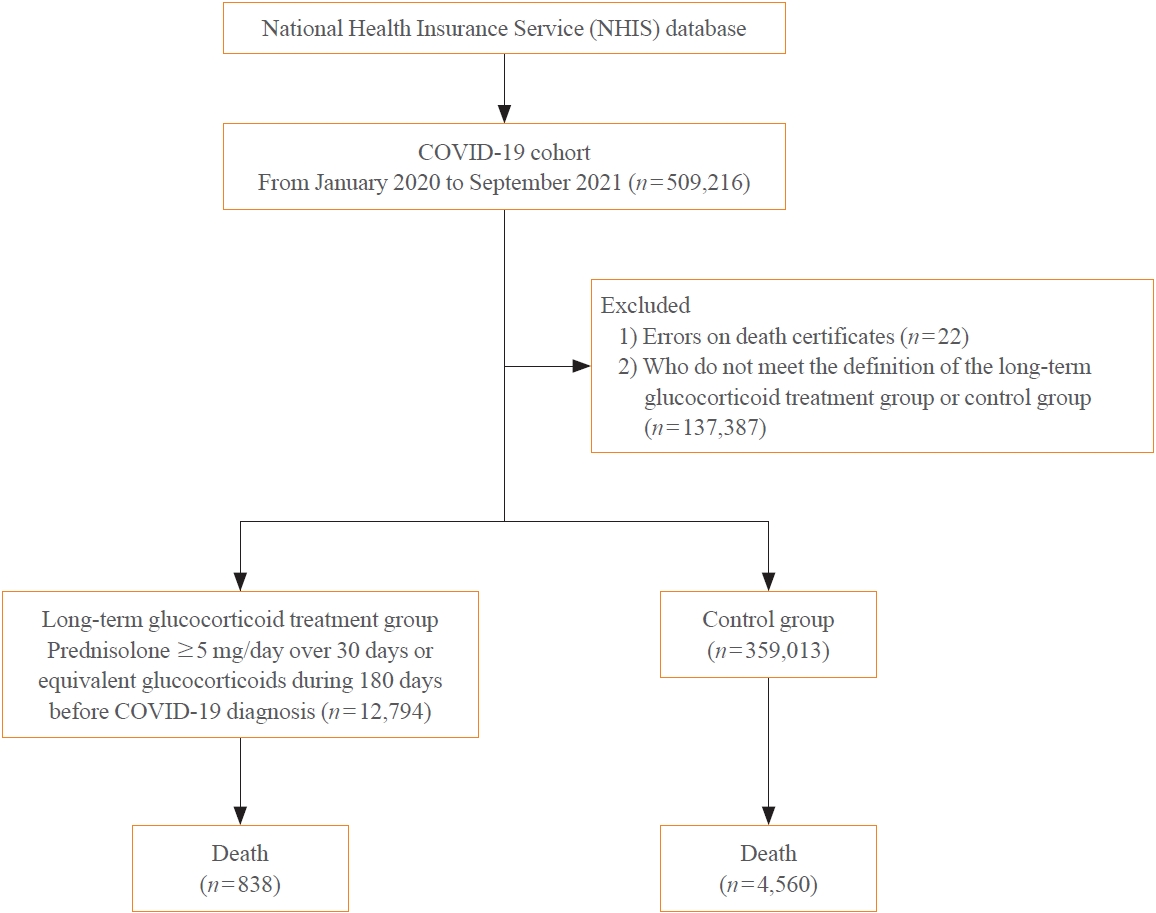
The severity of coronavirus disease 2019 (COVID-19) among patients with long-term glucocorticoid treatment (LTGT) has not been established. We aimed to evaluate the association between LTGT and COVID-19 prognosis.
Methods
A Korean nationwide cohort database of COVID-19 patients between January 2019 and September 2021 was used. LTGT was defined as exposure to at least 150 mg of prednisolone (≥5 mg/day and ≥30 days) or equivalent glucocorticoids 180 days before COVID-19 infection. The outcome measurements were mortality, hospitalization, intensive care unit (ICU) admission, length of stay, and mechanical ventilation.
Results
Among confirmed patients with COVID-19, the LTGT group (n=12,794) was older and had a higher proportion of comorbidities than the control (n=359,013). The LTGT group showed higher in-hospital, 30-day, and 90-day mortality rates than the control (14.0% vs. 2.3%, 5.9% vs. 1.1%, and 9.9% vs. 1.8%, respectively; all P<0.001). Except for the hospitalization rate, the length of stay, ICU admission, and mechanical ventilation proportions were significantly higher in the LTGT group than in the control (all P<0.001). Overall mortality was higher in the LTGT group than in the control group, and the significance remained in the fully adjusted model (odds ratio [OR], 5.75; 95% confidence interval [CI], 5.31 to 6.23) (adjusted OR, 1.82; 95% CI, 1.67 to 2.00). The LTGT group showed a higher mortality rate than the control within the same comorbidity score category.
Conclusion
Long-term exposure to glucocorticoids increased the mortality and severity of COVID-19. Prevention and early proactive measures are inevitable in the high-risk LTGT group with many comorbidities. -
Citations
Citations to this article as recorded by- Glucocorticoids as a Double-Edged Sword in the Treatment of COVID-19: Mortality and Severity of COVID-19 in Patients Receiving Long-Term Glucocorticoid Therapy
Eun-Hee Cho
Endocrinology and Metabolism.2023; 38(2): 223. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef
- Glucocorticoids as a Double-Edged Sword in the Treatment of COVID-19: Mortality and Severity of COVID-19 in Patients Receiving Long-Term Glucocorticoid Therapy

- Diabetes, obesity and metabolism
Big Data Articles (National Health Insurance Service Database) - Risk for Newly Diagnosed Type 2 Diabetes Mellitus after COVID-19 among Korean Adults: A Nationwide Matched Cohort Study
- Jong Han Choi, Kyoung Min Kim, Keeho Song, Gi Hyeon Seo
- Endocrinol Metab. 2023;38(2):245-252. Published online April 5, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1662
- 2,249 View
- 120 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Coronavirus disease 2019 (COVID-19) can cause various extrapulmonary sequelae, including diabetes. However, it is unclear whether these effects persist 30 days after diagnosis. Hence, we investigated the incidence of newly diagnosed type 2 diabetes mellitus (T2DM) in the post-acute phase of COVID-19.
Methods
This cohort study used data from the Health Insurance Review and Assessment Service, a representative national healthcare database in Korea. We established a cohort of 348,180 individuals diagnosed with COVID-19 without a history of diabetes between January 2020 and September 2021. The control group consisted of sex- and age-matched individuals with neither a history of diabetes nor COVID-19. We assessed the hazard ratios (HR) of newly diagnosed T2DM patients with COVID-19 compared to controls, adjusted for age, sex, and the presence of hypertension and dyslipidemia.
Results
In the post-acute phase, patients with COVID-19 had an increased risk of newly diagnosed T2DM compared to those without COVID-19 (adjusted HR, 1.30; 95% confidence interval [CI], 1.27 to 1.33). The adjusted HRs of non-hospitalized, hospitalized, and intensive care unit-admitted patients were 1.14 (95% CI, 1.08 to 1.19), 1.34 (95% CI, 1.30 to 1.38), and 1.78 (95% CI, 1.59 to 1.99), respectively. The risk of T2DM in patients who were not administered glucocorticoids also increased (adjusted HR, 1.29; 95% CI, 1.25 to 1.32).
Conclusion
COVID-19 may increase the risk of developing T2DM beyond the acute period. The higher the severity of COVID-19 in the acute phase, the higher the risk of newly diagnosed T2DM. Therefore, T2DM should be included as a component of managing long-term COVID-19. -
Citations
Citations to this article as recorded by- New-Onset Diabetes Mellitus in COVID-19: A Scoping Review
Anca Pantea Stoian, Ioana-Cristina Bica, Teodor Salmen, Wael Al Mahmeed, Khalid Al-Rasadi, Kamila Al-Alawi, Maciej Banach, Yajnavalka Banerjee, Antonio Ceriello, Mustafa Cesur, Francesco Cosentino, Alberto Firenze, Massimo Galia, Su-Yen Goh, Andrej Janez,
Diabetes Therapy.2024; 15(1): 33. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef
- New-Onset Diabetes Mellitus in COVID-19: A Scoping Review

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
- Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
- Endocrinol Metab. 2023;38(1):129-138. Published online January 27, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1609

- 2,133 View
- 156 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The severity of gestational diabetes mellitus (GDM) is associated with adverse pregnancy outcomes. We aimed to generate a risk model for predicting insulin-requiring GDM before pregnancy in Korean women.
Methods
A total of 417,210 women who received a health examination within 52 weeks before pregnancy and delivered between 2011 and 2015 were recruited from the Korean National Health Insurance database. The risk prediction model was created using a sample of 70% of the participants, while the remaining 30% were used for internal validation. Risk scores were assigned based on the hazard ratios for each risk factor in the multivariable Cox proportional hazards regression model. Six risk variables were selected, and a risk nomogram was created to estimate the risk of insulin-requiring GDM.
Results
A total of 2,891 (0.69%) women developed insulin-requiring GDM. Age, body mass index (BMI), current smoking, fasting blood glucose (FBG), total cholesterol, and γ-glutamyl transferase were significant risk factors for insulin-requiring GDM and were incorporated into the risk model. Among the variables, old age, high BMI, and high FBG level were the main contributors to an increased risk of insulin-requiring GDM. The concordance index of the risk model for predicting insulin-requiring GDM was 0.783 (95% confidence interval, 0.766 to 0.799). The validation cohort’s incidence rates for insulin-requiring GDM were consistent with the risk model’s predictions.
Conclusion
A novel risk engine was generated to predict insulin-requiring GDM among Korean women. This model may provide helpful information for identifying high-risk women and enhancing prepregnancy care. -
Citations
Citations to this article as recorded by- Establishment and validation of a nomogram to predict the neck contracture after skin grafting in burn patients: A multicentre cohort study
Rui Li, Yangyang Zheng, Xijuan Fan, Zilong Cao, Qiang Yue, Jincai Fan, Cheng Gan, Hu Jiao, Liqiang Liu
International Wound Journal.2023; 20(9): 3648. CrossRef - Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus
Anna S. Koefoed, H. David McIntyre, Kristen S. Gibbons, Charlotte W. Poulsen, Jens Fuglsang, Per G. Ovesen
Reproductive Medicine.2023; 4(3): 133. CrossRef - Prepregnancy Glucose Levels Within Normal Range and Its Impact on Obstetric Complications in Subsequent Pregnancy: A Population Cohort Study
Ho Yeon Kim, Ki Hoon Ahn, Geum Joon Cho, Soon-Cheol Hong, Min-Jeong Oh, Hai-Joong Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - The CHANGED Score—A New Tool for the Prediction of Insulin Dependency in Gestational Diabetes
Paul Rostin, Selina Balke, Dorota Sroka, Laura Fangmann, Petra Weid, Wolfgang Henrich, Josefine Theresia Königbauer
Journal of Clinical Medicine.2023; 12(22): 7169. CrossRef
- Establishment and validation of a nomogram to predict the neck contracture after skin grafting in burn patients: A multicentre cohort study

Review Article
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
- Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
- Endocrinol Metab. 2023;38(1):10-24. Published online February 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.102
- 3,738 View
- 262 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - The Korean National Health Information Database (NHID) contains big data combining information obtained from the National Health Insurance Service and health examinations. Data are provided in the form of a cohort, and the NHID can be used to conduct longitudinal studies and research on rare diseases. Moreover, data on the cause and date of death are provided by Statistics Korea. Research and publications based on the NHID have increased explosively in the field of endocrine disorders. However, because the data were not collected for research purposes, studies using the NHID have limitations, particularly the need for the operational definition of diseases. In this review, we describe the characteristics of the Korean NHID, operational definitions of endocrine diseases used for research, and an overview of recent studies in endocrinology using the Korean NHID.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Diabetes severity and the risk of depression: A nationwide population-based study
Yunjung Cho, Bongsung Kim, Hyuk-Sang Kwon, Kyungdo Han, Mee Kyoung Kim
Journal of Affective Disorders.2024; 351: 694. CrossRef - Information Bias Might Exaggerate Lung Cancer Risk of Patients With Rheumatoid Arthritis
Nobuyuki Horita, Kaoru Takase-Minegishi
Journal of Thoracic Oncology.2024; 19(2): 348. CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
Endocrinology and Metabolism.2023; 38(6): 690. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study

Original Articles
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Metformin and Cervical Cancer Risk in Patients with Newly Diagnosed Type 2 Diabetes: A Population-Based Study in Korea
- Hyun Min Kim, Min Jin Kang, Sun Ok Song
- Endocrinol Metab. 2022;37(6):929-937. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1613
- Correction in: Endocrinol Metab 2023;38(1):174
- 2,446 View
- 218 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Cervical cancer is a prevalent malignancy that is a major health problem for women worldwide. The cancer-preventive properties of metformin are well-known, but insufficient data have been reported regarding its relationship to cervical cancer. Therefore, in a nationwide population-based study, we investigated the association between metformin use and cervical cancer incidence in patients with newly diagnosed type 2 diabetes.
Methods
This retrospective cohort study used the Korean National Health Insurance claims database. Individuals newly diagnosed with type 2 diabetes between January 2005 and December 2009 were included. The occurrence of cervical cancer was explored by matching for age, economic status, region of residence, and use of anti-diabetic medication.
Results
In total, 66,013 metformin users and 64,756 non-users were analyzed. Cervical cancer occurred in 219 metformin users (0.33%) and 274 metformin non-users (0.42%) (hazard ratio [HR], 0.783; 95% confidence interval [CI], 0.655 to 0.036; P=0.007). Moreover, cervical cancer risk was considerably reduced in those treated with a high dose (>1,200,000 mg) or for an extended period (≥2,000 days) compared to non-users (HR, 0.151; 95% CI, 0.093 to 0.243; P<0.001; and HR, 0.141; 95% CI, 0.077 to 0.258; P<0.001). The incidence was also significantly lower in metformin users among those over 50 years old (HR, 0.791; 95% CI, 0.650 to 0.961; P<0.001).
Conclusion
Metformin use in patients with newly diagnosed diabetes was associated with a lower risk of cervical cancer in Korea. Furthermore, a significant association was found between the use of metformin and cervical cancer in a dose- and duration-dependent manner and among those over 50 years old. -
Citations
Citations to this article as recorded by- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp
Mohamad Ali Hijazi, André Gessner, Nahed El-Najjar
Cancers.2023; 15(12): 3199. CrossRef - Network-based drug repurposing for HPV-associated cervical cancer
Faheem Ahmed, Young Jin Yang, Anupama Samantasinghar, Young Woo Kim, Jeong Beom Ko, Kyung Hyun Choi
Computational and Structural Biotechnology Journal.2023; 21: 5186. CrossRef - The Use of Metformin and Postoperative Insulin Pump Were Predictive Factors for Outcomes of Diabetic Colorectal Cancer Patients after Surgery
Xu-Rui Liu, Fei Liu, Zi-Wei Li, Quan Lv, Xin-Peng Shu, Lian-Shuo Li, Yue Tong, Wei Zhang, Dong Peng
Nutrition and Cancer.2023; 75(10): 1926. CrossRef
- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Recent Changes in the Incidence of Thyroid Cancer in Korea between 2005 and 2018: Analysis of Korean National Data
- Yun Mi Choi, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
- Endocrinol Metab. 2022;37(5):791-799. Published online October 11, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1533
- 2,769 View
- 195 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
In this study, we evaluated the recent changes in the standardized, age-specific, stage-specific incidence rates (IRs) of thyroid cancer in Korea and compared them with the incidence data reported by the Surveillance, Epidemiology, and End Results Program.
Methods
The analysis was conducted using the incidence data (2005 to 2018) from the Statistics Korea and Korea Central Cancer Registry.
Results
The age-standardized IR (SIR) of thyroid cancer increased from 24.09 per 100,000 in 2005 to 74.83 in 2012 (annual percent change [APC], 14.5). From 2012 to 2015, the SIR decreased to 42.52 (APC, –17.9) and then remained stable until 2018 (APC, 2.1). This trend was similar in both men and women. Regarding age-specific IRs, the IRs for ages of 30 years and older showed a trend similar to that of the SIR; however, for ages below 30 years, no significant reduction was observed from the vertex of IR in 2015. Regarding stage-specific IRs, the increase was more prominent in those with regional disease (APC, 17.4) than in those with localized disease until 2012; then, the IR decreased until 2015 (APC, –16.1). The average APC from 2005 to 2018 increased in men, those under the age of 30 years, and those with regional disease.
Conclusion
The SIR in Korea peaked in 2012 and decreased until 2015 and then remained stable until 2018. However, in young individuals under the age of 30 years, the IR did not significantly decrease but tended to increase again. In terms of stage-specific IRs, the sharpest increase was seen among those with regional disease. -
Citations
Citations to this article as recorded by- Comparison of postoperative pain between transoral and conventional thyroidectomy: a propensity score-matched analysis
Min Kyu Park, Van Cuong Nguyen, Eugene Kim, Chang Myeon Song, Yong Bae Ji, Jin Hyeok Jeong, Kyung Tae
Surgical Endoscopy.2024; 38(3): 1512. CrossRef - Contents analysis of thyroid cancer-related information uploaded to YouTube by physicians in Korea: endorsing thyroid cancer screening, potentially leading to overdiagnosis
EunKyo Kang, HyoRim Ju, Soojeong Kim, Juyoung Choi
BMC Public Health.2024;[Epub] CrossRef - Bilateral axillo-breast approach robotic total thyroidectomy without isthmectomy: a case report
Hyeji Kim, Hyeonuk Hwang, Hyungju Kwon
The Ewha Medical Journal.2024;[Epub] CrossRef - Association between Consumption of Iodine-Rich Foods and Thyroid Cancer Prevalence: Findings from a Large Population-Based Study
Yu-Jin Kwon, Hye-Sun Lee, Sang-Wook Kang, Ji-Won Lee
Nutrients.2024; 16(7): 1041. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Survival Comparison of Incidentally Found versus Clinically Detected Thyroid Cancers: An Analysis of a Nationwide Cohort Study
Shinje Moon, Eun Kyung Lee, Hoonsung Choi, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 81. CrossRef - Cumulative exposure to metabolic syndrome increases thyroid cancer risk in young adults: a population-based cohort study
Jinyoung Kim, Kyungdo Han, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2023; 38(4): 526. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Long-Term Changes in the Mortality Rates of Thyroid Cancer in Korea: Analysis of Korean National Data from 1985 to 2020
Yun Mi Choi, Min-Ju Kim, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
Endocrinology and Metabolism.2023; 38(5): 588. CrossRef - Age and Post-Lobectomy Recurrence after Endoscopic or Robotic Thyroid Surgery: A Retrospective Cohort Study of 2348 Papillary Thyroid Carcinoma Patients
Jin-Seong Cho, Yong-Min Na, Hee Kyung Kim
Cancers.2023; 15(23): 5506. CrossRef
- Comparison of postoperative pain between transoral and conventional thyroidectomy: a propensity score-matched analysis

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Association among Current Smoking, Alcohol Consumption, Regular Exercise, and Lower Extremity Amputation in Patients with Diabetic Foot: Nationwide Population-Based Study
- Yoon Jae Lee, Kyung-Do Han, Jun Hyeok Kim
- Endocrinol Metab. 2022;37(5):770-780. Published online October 12, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1519
- 3,273 View
- 202 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
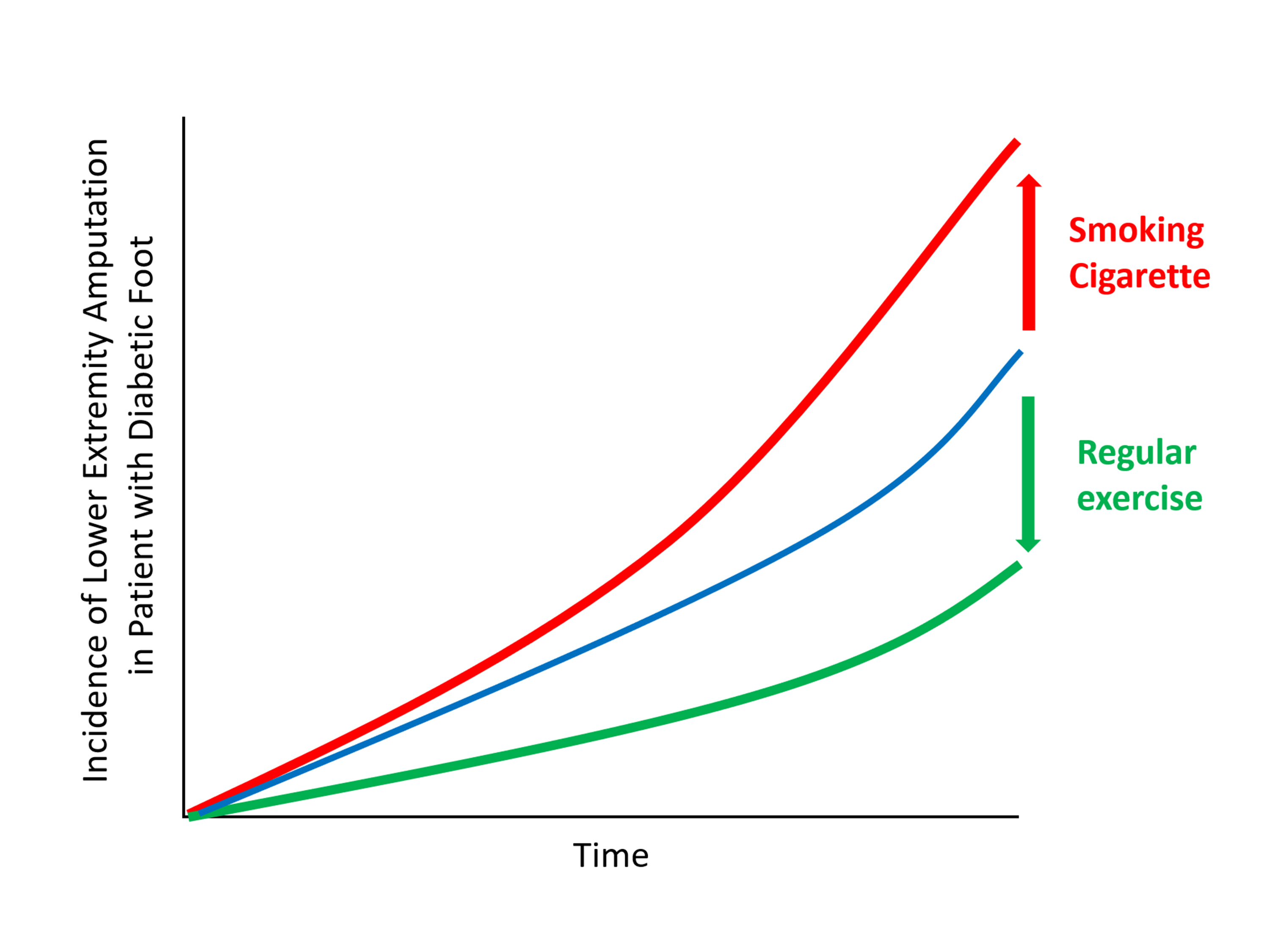
The present study investigates whether modifiable behavioral factors of current cigarette smoking, heavy alcohol consumption, and regular exercise are associated with risk of lower extremity amputation (LEA) in diabetic patients.
Methods
A total of 2,644,440 diabetic patients (aged ≥20 years) was analyzed using the database of the Korean National Health Insurance Service. Cox proportional hazard regression was used to assess adjusted hazard ratios (HRs) for the behavioral factors with risk of LEA under adjustment for potential confounders.
Results
The risk of LEA was significantly increased by current cigarette smoking and heavy alcohol consumption (HR, 1.436; 95% confidence interval [CI], 1.367 to 1.508 and HR, 1.082; 95% CI, 1.011 to 1.158) but significantly decreased with regular exercise (HR, 0.745; 95% CI, 0.706 to 0.786) after adjusting for age, sex, smoking, alcohol consumption, exercise, low income, hypertension, dyslipidemia, body mass index, using insulin or oral antidiabetic drugs, and diabetic duration. A synergistically increased risk of LEA was observed with larger number of risky behaviors.
Conclusion
Modification of behaviors of current smoking, heavy alcohol intake, and exercise prevents LEA and can improve physical, emotional, and social quality of life in diabetic patients. -
Citations
Citations to this article as recorded by- Adjuvant effect of antimicrobial photodynamic therapy (aPDT) in the treatment of diabetic foot ulcers: A case series
Rita de Cassia Ferreira, Rebeca Boltes Cecatto, Silvana Torres Perez, Raquel Agnelli Mesquita‐Ferrari, Sandra Kalil Bussadori, Cinthya Cosme Duran, Anna Carolina Tempestini Horliana, Kristianne Porta Santos Fernandes
Journal of Biophotonics.2024;[Epub] CrossRef - Factors associated with diabetic foot ulcers and lower limb amputations in type 1 and type 2 diabetes supported by real‐world data from the German/Austrian DPV registry
Alexander J. Eckert, Stefan Zimny, Marcus Altmeier, Ana Dugic, Anton Gillessen, Latife Bozkurt, Gabriele Götz, Wolfram Karges, Frank J. Wosch, Stephan Kress, Reinhard W. Holl
Journal of Diabetes.2024;[Epub] CrossRef - Investigating Diabetic Foot Pathophysiology and Amputation Prevention Strategies through Behavioral Modification
Jun Hyeok Kim
Journal of Wound Management and Research.2023; 19(3): 167. CrossRef
- Adjuvant effect of antimicrobial photodynamic therapy (aPDT) in the treatment of diabetic foot ulcers: A case series

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
- Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
- Endocrinol Metab. 2022;37(5):759-769. Published online October 5, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1515
- 3,171 View
- 192 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
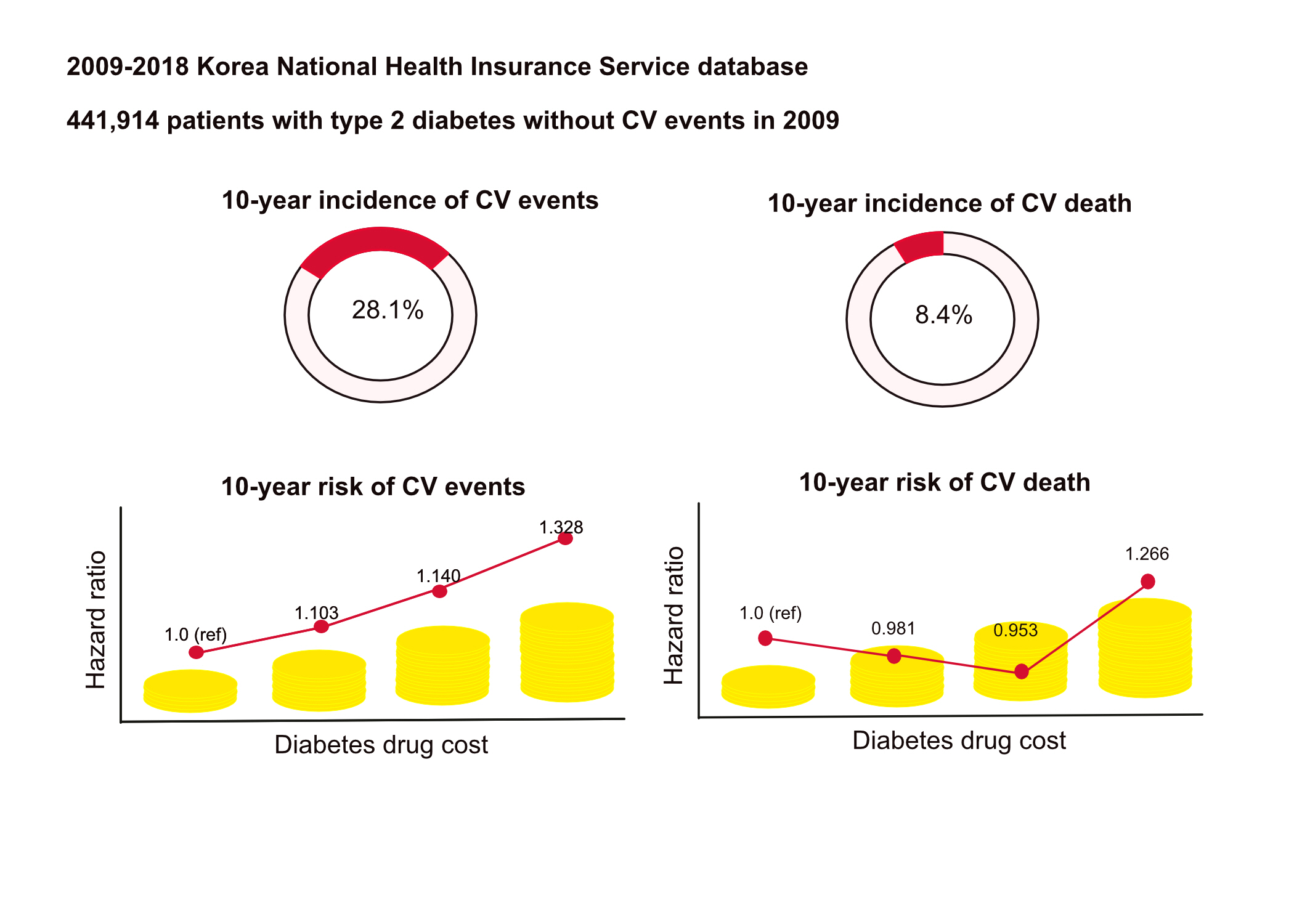
This study aimed to investigate the long-term effects of diabetes drug costs on cardiovascular (CV) events and death.
Methods
This retrospective observational study used data from 2009 to 2018 from the National Health Insurance in Korea. Among the patients with type 2 diabetes, those taking antidiabetic drugs and who did not have CV events until 2009 were included. Patients were divided into quartiles (Q1 [lowest]–4 [highest]) according to the 2009 diabetes drug cost. In addition, the 10-year incidences of CV events (non-fatal myocardial infarction, stroke, hospitalization for heart failure, and coronary revascularization) and CV death (death due to CV events) were analyzed.
Results
A total of 441,914 participants were enrolled (median age, 60 years; men, 57%). CV events and death occurred in 28.1% and 8.36% of the patients, respectively. The 10-year incidences of CV events and deaths increased from Q1 to 4. After adjusting for sex, age, income, type of diabetes drugs, comorbidities, and smoking and drinking status, the risk of CV events significantly increased according to the sequential order of the cost quartiles. In contrast, the risk of CV death showed a U-shaped pattern, which was the lowest in Q3 (hazard ratio [HR], 0.953; 95% confidence interval [CI], 0.913 to 0.995) and the highest in Q4 (HR, 1.266; 95% CI, 1.213 to 1.321).
Conclusion
Diabetes drug expenditure affects 10-year CV events and mortality. Therefore, affording an appropriate diabetes drug cost at a similar risk of CV is an independent protective factor against CV death. -
Citations
Citations to this article as recorded by- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef
- Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
- Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
- Endocrinol Metab. 2022;37(3):466-474. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1440
- 3,888 View
- 138 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
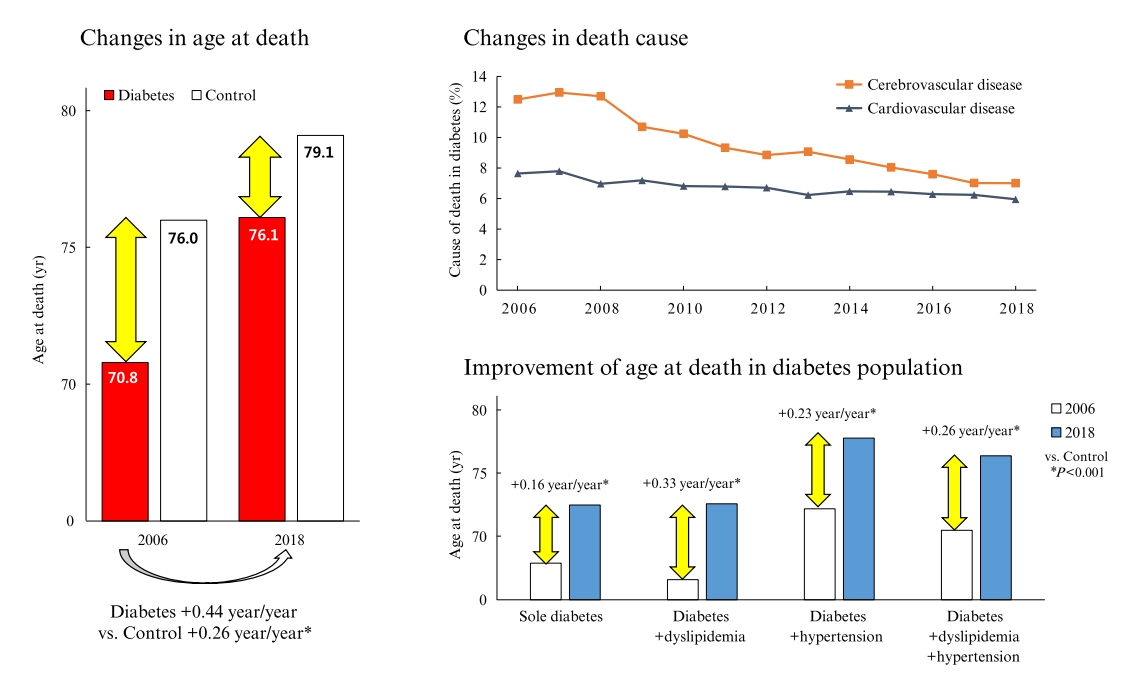
Diabetes is a leading cause of death that is responsible for 1.6 million annual deaths worldwide. However, the life expectancy and age at death of people with diabetes have been a matter of debate.
Methods
The National Health Insurance Service claims database, merged with death records from the National Statistical Information Service in Korea from 2006 to 2018, was analyzed.
Results
In total, 1,432,567 deaths were collected. The overall age at death increased by 0.44 and 0.26 year/year in the diabetes and control populations, respectively. The disparity in the mean age at death between the diabetes and control populations narrowed from 5.2 years in 2006 to 3.0 years in 2018 (p<0.001). In a subgroup analysis according to the presence of comorbid diseases, the number and proportion of deaths remained steady in the group with diabetes only, but steadily increased in the groups with diabetes combined with dyslipidemia and/or hypertension. Compared to the control population, the increase in the mean death age was higher in the population with diabetes. This trend was more prominent in the groups with dyslipidemia and/or hypertension than in the diabetes only group. Deaths from vascular disease and diabetes decreased, whereas deaths from cancer and pneumonia increased. The decline in the proportion of deaths from vascular disease was greater in the diabetes groups with hypertension and/or dyslipidemia than in the control population.
Conclusion
The age at death in the population with diabetes increased more steeply and reached a comparable level to those without diabetes. -
Citations
Citations to this article as recorded by- Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study
Iee-Ho Choi, Sang-Woo Yeom, Sun-Young Kim, Jihye You, Jong-Seung Kim, Minsun Kim
Children.2023; 10(2): 358. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef
- Analysis of Cause-of-Death Mortality in Children and Young Adults with Diabetes: A Nationwide 10-Year Follow-Up Cohort Study

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Repeated Low High-Density Lipoprotein Cholesterol and the Risk of Thyroid Cancer: A Nationwide Population- Based Study in Korea
- Jinyoung Kim, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2022;37(2):303-311. Published online April 6, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1332
- 4,644 View
- 154 Download
- 12 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
High-density lipoprotein cholesterol (HDL-C) plays an important role in the reverse cholesterol transport pathway and prevents atherosclerosis-mediated disease. It has also been suggested that HDL-C may be a protective factor against cancer. However, an inverse correlation between HDL-C and cancer has not been established, and few studies have explored thyroid cancer.
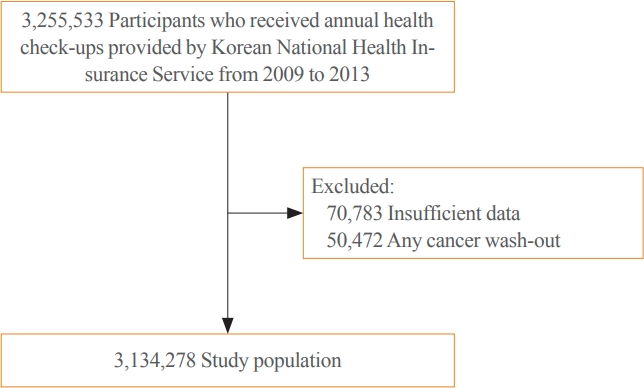
Methods
The study participants received health checkups provided by the Korean National Health Insurance Service from 2009 to 2013 and were followed until 2019. Considering the variability of serum HDL-C level, low HDL-C level was analyzed by grouping based on four consecutive health checkups. The data analysis was performed using univariate and multivariate Cox proportional hazard regression models.
Results
A total of 3,134,278 total study participants, thyroid cancer occurred in 16,129. In the crude model, the hazard ratios for the association between repeatedly measured low HDL-C levels and thyroid cancer were 1.243, 1.404, 1.486, and 1.680 (P for trend <0.01), respectively, which were significant even after adjusting for age, sex, lifestyle factors, and metabolic diseases. The subgroup analysis revealed that low HDL-C levels likely had a greater impact on the group of patients with central obesity (P for interaction= 0.062), high blood pressure (P for interaction=0.057), impaired fasting glucose (P for interaction=0.051), and hyperlipidemia (P for interaction=0.126).
Conclusion
Repeatedly measured low HDL-C levels can be considered a risk factor for cancer as well as vascular disease. Low HDL-C levels were associated with the risk of thyroid cancer, and this correlation was stronger in a metabolically unhealthy population. -
Citations
Citations to this article as recorded by- Association between total cholesterol levels and all-cause mortality among newly diagnosed patients with cancer
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Scientific Reports.2024;[Epub] CrossRef - Association between organophosphate flame retardant exposure and lipid metabolism: data from the 2013–2014 National Health and Nutrition Examination Survey
Fu-Jen Cheng, Kai-Fan Tsai, Kuo-Chen Huang, Chia-Te Kung, Wan-Ting Huang, Huey-Ling You, Shau-Hsuan Li, Chin-Chou Wang, Wen-Chin Lee, Hsiu-Yung Pan
Frontiers in Public Health.2024;[Epub] CrossRef - Low serum total cholesterol levels predict inferior prognosis of patients with POEMS syndrome
Jue Zhang, Ting Zhang, Ye Yao, Xuxing Shen, Yuanyuan Jin, Run Zhang, Lijuan Chen
Discover Oncology.2024;[Epub] CrossRef - Lipoprotein alterations in endocrine disorders - a review of the recent developments in the field
Michal Olejarz, Ewelina Szczepanek-Parulska, Marek Ruchala
Frontiers in Endocrinology.2024;[Epub] CrossRef - Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort
Xue Xiao, Yi Huang, Fetemeh Sadeghi, Maria Feychting, Niklas Hammar, Fang Fang, Zhe Zhang, Qianwei Liu
Cancers.2023; 15(2): 520. CrossRef - Altered serum lipid levels are associated with prognosis of diffuse large B cell lymphoma and influenced by utility of rituximab
Fei Wang, Luo Lu, HuiJuan Chen, Yanhua Yue, Yanting Sun, Feng Yan, Bai He, Rongrong Lin, Weiying Gu
Annals of Hematology.2023; 102(2): 393. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - High-density lipoprotein cholesterol and carcinogenesis
Meijuan Tan, Shijie Yang, Xiequn Xu
Trends in Endocrinology & Metabolism.2023; 34(5): 303. CrossRef - Low Serum Cholesterol Level Is a Significant Prognostic Factor That Improves CLL-IPI in Chronic Lymphocytic Leukaemia
Rui Gao, Kaixin Du, Jinhua Liang, Yi Xia, Jiazhu Wu, Yue Li, Bihui Pan, Li Wang, Jianyong Li, Wei Xu
International Journal of Molecular Sciences.2023; 24(8): 7396. CrossRef - Do metabolic factors increase the risk of thyroid cancer? a Mendelian randomization study
Weiwei Liang, FangFang Sun
Frontiers in Endocrinology.2023;[Epub] CrossRef - Assessment of causal association between differentiated thyroid cancer and disordered serum lipid profile: a Mendelian randomization study
Qiang Ma, Yu Li, Lijuan An, Liang Guo, Xiaokang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Risk factors and diagnostic prediction models for papillary thyroid carcinoma
Xiaowen Zhang, Yuyang Ze, Jianfeng Sang, Xianbiao Shi, Yan Bi, Shanmei Shen, Xinlin Zhang, Dalong Zhu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Exposure to multiple trace elements and thyroid cancer risk in Chinese adults: A case-control study
Jia-liu He, Hua-bing Wu, Wen-lei Hu, Jian-jun Liu, Qian Zhang, Wei Xiao, Ming-jun Hu, Ming Wu, Fen Huang
International Journal of Hygiene and Environmental Health.2022; 246: 114049. CrossRef
- Association between total cholesterol levels and all-cause mortality among newly diagnosed patients with cancer


 KES
KES

 First
First Prev
Prev



